A closer look at individuals who died from opioid overdose during the overdose crisis
Opioid overdose carries a massive individual and societal toll. Less well appreciated, however, is the risk for overdose conferred by stimulants like cocaine and amphetamines, and their interaction with opioids. While certain risk factors for opioid overdose are well known and appreciated, factors affecting risk for overdose from opioids alone versus risk for overdose from opioids in combination with other drugs are less well understood.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
This study helped characterize opioid deaths in a U.S. state hit particularly hard by the opioid epidemic – Massachusetts – while also examining how stimulants may fit into the picture so providers and policy makers can better address the current opioid crisis. To this end, the authors describe individual and demographic factors that may heighten risk for opioid overdose, either alone, or in combination with other drugs.
HOW WAS THIS STUDY CONDUCTED?
Barocas and colleagues analyzed data from the Massachusetts Public Health Data Warehouse – a dataset supported by several Massachusetts government agencies that was assembled to address the opioid epidemic. Using these records, the authors analyzed opioid overdose deaths among persons 11 years of age and older from January 1, 2014 through December 31, 2015, excluding cases where individuals died as a result of suicide, assault, or homicide. Cases were only included in the analysis if toxicology reports showed the presence of opioids, with or without stimulants and other drugs.
Based on toxicology reports, the authors divided the population into three mutually exclusive groups: (1) opioid-related deaths with opioids only, (2) opioid-related deaths with opioids and another substances (i.e., benzodiazepines, alcohol, marijuana, gabapentin, or clonidine) but not including stimulants (i.e., cocaine or amphetamines), and (3) opioid-related deaths with opioids and stimulants with or without another substance.
WHAT DID THIS STUDY FIND?
Between 2014 and 2015, the authors identified a total of 2,928 opioid-related overdoses in Massachusetts, and 2,244 (77%) that had accompanying toxicology results. Of these opioid-related deaths for which toxicology results were available, 72% involved fentanyl or heroin without prescription opioids; 9% involved prescription opioids (e.g., oxycodone, hydrocodone) without fentanyl or heroin; 19% involved both. Additionally, 83% of these opioid-related deaths involved another substance in addition to opioids. Specifically, 17% (n= 389) had opioids only; 47% (n= 1,047) had opioids and another non-stimulant substance; 36% (n= 808) had opioids plus stimulants with or without another substance.
More than half (54%) of all overdoses occurred in people with a co-occurring mental health disorder including major depression, bipolar disorder, or schizophrenia. Results showed that persons with a psychiatric disorder other than substance use disorder were 56% more likely to overdose with opioids and stimulants than with opioids alone, compared to those without a psychiatric disorder other than substance use disorder.
Also, persons in age groupings 25 – 44, and 45 and older were 84% and 70% more likely than the youngest age group (ages 11 – 24) to overdose with a combination of opioids and stimulants, versus opioids alone. Similarly, residents of rural areas were about half as likely (0.52) as residents of non-rural areas to overdose with a combination of opioids and stimulants, versus opioids alone. Further, persons with recent incarceration were about half as likely (0.53 times) as those without recent incarceration to die of opioids in combination with other non-stimulant substances, versus opioids alone.
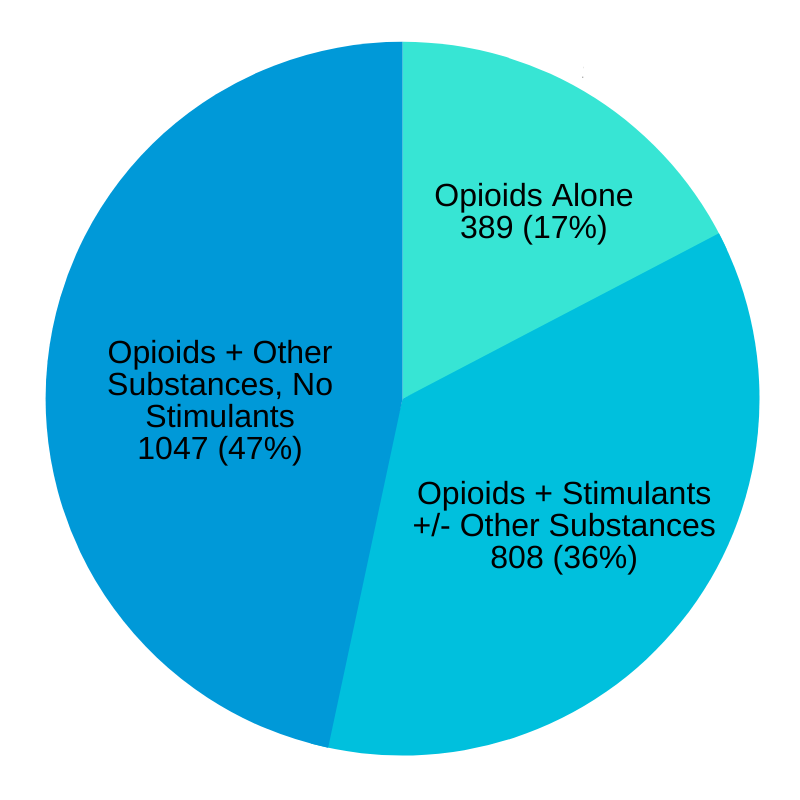
Figure 1. Data retrieved from Barocas et al., 2019. Opioid-related overdose deaths in the state of Massachusetts from 2014 to 2015. The pie chart represents the 2,244 identified overdose related deaths for which toxicology reports were available, showing only 17% of cases involved opioids alone, while 36% involved opioids plus stimulants (with or without other drugs), and 47% of cases involved opioids and other drugs, but not stimulants.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study highlights the high prevalence of the involvement of drugs other than opioids in opioid-related overdoses in the state of Massachusetts. Specifically, 5 out of 6 overdoses (83%) involved another substance in addition to an opioid, and 19% of all deaths involved both heroin or fentanyl and prescription opioids.
This study also shows how co-occurring psychiatric disorders might heighten risk for overdose. Over half of all overdoses occurred in individuals with a co-occurring psychiatric disorders. These individuals were also more likely to die with other substances – with or without stimulants – than opioids alone, suggesting greater, high-risk multi-substance use among these people.
It is also noteworthy that the youngest age group (ages 11 – 24) were less likely than the older age groups (25 – 44, and 45 and older) to die with both opioids and stimulants like methamphetamine in their system. Though youth is typically associated with greater poly-substance use, it could be that the youngest age group here has less drug experience and died before transitioning to the use of other substances.
Results also showed that the majority of overdose deaths (93%) occurred in non-rural areas, and that those living in non-rural areas were much more likely to die of a combination of opioids and stimulants, than with opioids alone. This of course should not be taken to mean that overdoses aren’t frequent in rural areas and rural areas aren’t adversely impacted by the current overdose crisis. Rather, these statistics most likely reflect the population distribution in Massachusetts, a state in which the majority of the population lives in non-rural areas. More overdoses are likely to occur in non-rural areas because more people live there.
Recent incarceration is a well-known risk factor for opioid overdose, because individuals coming out of prison typically have reduced physiological tolerance to opioids, and except in certain states, have limited access to life saving opioid use disorder medications such as buprenorphine (commonly known by its brand name Subutex, or when combined with naloxone, known by the brand name Suboxone). It is not clear why persons with recent incarceration were more likely than those without recent incarceration to die of opioids alone, versus opioids in combination with other non-stimulant substances. It is possible that those recently incarcerated, compared to those not, represent two distinct populations, but more research is needed to clarify this.
Taken together, these findings highlight the importance of adequately addressing modifiable risk factors such as access to mental health services, homelessness, and incarceration when addressing the opioid overdose crisis. Moreover, a singular focus on opioid use disorder may not be sufficient. Any kind of lasting, sustained plan to address the current overdose crisis might need to take into consideration stimulants and other substance use, particularly benzodiazepines and alcohol. Interventions aimed at decreasing overdose risk may need to account for multi-substance use, and not focus exclusively on opioid use.
- LIMITATIONS
-
- The authors note that while the Public Health Dataset individually links multiple data sets, in most cases these datasets are comprised of administrative data that may be incomplete.
- They also note that they did not include all possible drugs found in toxicology; rather, they chose the ones most likely to be involved in opioid overdoses. This means cases of overdose involving other opioid + other drug combinations could have been missed in this analysis.
- It is not clear to what degree substances other than opioids played into the overdose fatalities reported in this study. While sedative hypnotics like alcohol and benzodiazepines have well known additive effects when combined with opioids that can increase risk for overdose, stimulant opioid interaction effects and the risk this combination confers for overdose is less well understood.
BOTTOM LINE
- For individuals and families seeking recovery: The authors found that the majority of opioid overdose deaths also involved other drugs, and that individuals with other psychiatric disorders (in addition to substance use disorder) were more likely to overdose with opioids and stimulants than with opioids alone. Also, those living in non-rural areas were much more likely than residents of rural areas to overdose with a combination of opioids and stimulants, than with opioids alone. Additionally, persons with recent incarceration were significantly more likely than those without recent incarceration to die of opioids alone, versus opioids in combination with other non-stimulant substances. A comprehensive and sustained approach to addressing opioid use disorder in the U.S. will ideally target substance use more broadly, and its psychosocial determinants like mental health and homelessness that can increase overdose risk. In other words, drugs other than opioids and individual factors may amplify overdose risk and should be treatment targets.
- For treatment professionals and treatment systems: The authors found that the majority of opioid overdose deaths also involved opioids in combination with other drugs, and that individuals with other psychiatric disorders (in addition to substance use disorder) were more likely to overdose with opioids and stimulants than with opioids alone. Also, those living in non-rural areas were much more likely than residents of rural areas to overdose with a combination of opioids and stimulants, than with opioids alone. Additionally, persons with recent incarceration were significantly more likely than those without recent incarceration to die of opioids alone, versus opioids in combination with other non-stimulant substances. A comprehensive and sustained approach to addressing opioid use disorder in the U.S. will ideally target substance use more broadly, and its psychosocial determinants like mental health and homelessness that can increase overdose risk. Drugs other than opioids can interact with opioids in expected as well as unknown ways and contribute to the current opioid overdose crisis. Opioid use cessation should not be the sole treatment target, rather, overdose risk may be reduced if other substance use is concurrently targeted.
- For scientists: The authors found that the majority of opioid overdose deaths also involved other drugs, and that individuals with other psychiatric disorders (in addition to substance use disorder) were more likely to overdose with opioids and stimulants than with opioids alone. Also, those living in non-rural areas were much more likely than residents of rural areas to overdose with a combination of opioids and stimulants, than with opioids alone. Additionally, persons with recent incarceration were significantly more likely than those without recent incarceration to die of opioids alone, versus opioids in combination with other non-stimulant substances. A comprehensive and sustained approach to addressing opioid use disorder in the U.S. will ideally target other substance use in addition to opioids, and its psychosocial determinants like mental health and homelessness that can underlie overdose risk. Drugs other than opioids interact with opioids in expected as well as unknown ways and contribute to the current opioid overdose crisis. Research is needed to improve our understanding of the role of opioid/other drug interactions in overdose fatalities. Also, more work is needed to better understand the social determinants of overdose death.
- For policy makers: The authors found that the majority of opioid overdose deaths involved other drugs, and that individuals with other psychiatric disorders (in addition to substance use disorder) were more likely to overdose with opioids and stimulants than with opioids alone. Also, those living in non-rural areas were much more likely than residents of rural areas to overdose with a combination of opioids and stimulants, than with opioids alone. Additionally, persons with recent incarceration were significantly more likely than those without recent incarceration to die of opioids alone, versus opioids in combination with other non-stimulant substances. A comprehensive and sustained approach to addressing opioid use disorder in the U.S. will ideally target substance use more broadly, and its psychosocial determinants like mental health and homelessness that can underlie overdose risk. Drugs other than opioids interact with opioids in expected as well as unknown ways and contribute to the current opioid overdose crisis. Also, these findings highlight the pressing need for integration of opioid use disorder treatments such as buprenorphine into prisons to protect individuals from overdose shortly after release.
CITATIONS
Barocas, J. A., Wang, J., Marshall, B. D. L., LaRochelle, M. R., Bettano, A., Bernson, D., . . . Walley, A. Y. (2019). Sociodemographic factors and social determinants associated with toxicology confirmed polysubstance opioid-related deaths. Drug and Alcohol Dependence, 200, 59-63. doi: 10.1016/j.drugalcdep.2019.03.014

