Toward improving opioid use disorder treatment for American Indian/Alaska Native individuals
White communities have been hit hard by the current opioid crisis contributing to declining life expectancy, also known as “deaths of despair,” but American Indians/Alaska Natives have fared even worse. Overdose rates have peaked among American Indians and efforts are stifled by a lack of information about this group. This rare national study uncovered a lead on how to reduce overdose among American Indian/Alaska Native people.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
American Indians/Alaska Natives had the highest per capita overdose rates compared to other racial groups. In order to know why they are disproportionately affected, researchers must search for clinical and social factors to which they are disproportionately exposed. Pharmaceutical options for opioid use disorder are considered “best practice,” front-line treatments that provide overdose protection, but the degree to which they are currently available and used among American Indian/Alaska Natives is not well understood. This study sought to fill this knowledge gap in the hope of saving more lives.
HOW WAS THIS STUDY CONDUCTED?
Researchers used two national databases to estimate availability and use of medications for opioid use disorder among American Indians/Alaska Natives across the U.S. Availability of medication was estimated using the 2018 National Survey on Substance Abuse Treatment Services (N-SSATS). Utilization of medication was estimated using the 2017 Treatment Episode Dataset (TEDS).
Availability estimations among facilities serving American Indian/Alaska Natives were broken down into proportion of facilities that offer any FDA approved medication for any purpose (e.g., withdrawal management, detoxification, or ongoing treatment), vs. facilities that offered agonist medications (i.e., methadone or buprenorphine) for ongoing treatment. Geographical differences in availability were mapped across states among facilities that offer any FDA-approved medication.
Utilization estimations measured the proportion of American Indian/Alaska Native client admissions relative to all other racial groups that received medication for opioid use disorder. A sub-group analysis tested American Indian/Alaska Natives were more likely to receive medication for tapering/withdrawal vs. continued treatment by excluding admission to detoxification settings. Geographical differences across states were mapped.
Factors that disproportionately affect the use of medication among American Indian/Alaska Native clients compared to other racial groups were identified while equating the groups on clinical, sociodemographic, regional, and treatment characteristics.
WHAT DID THIS STUDY FIND?
Availability of agonist medications (i.e., methadone or buprenorphine) for ongoing treatment as opposed to detoxification alone was slightly lower among facilities serving American Indian and Alaska Natives compared to facilities not explicitly serving them (22.4% vs. 27.6%, p<.001).
Availability of any FDA-approved medication for the treatment of opioid use disorder was similar between facilities that served American Indians/Alaska Natives and facilities that did not explicitly serve them (39.5% vs. 40.6 %, p = 0.43). Figure 1 displays geographical differences across states.
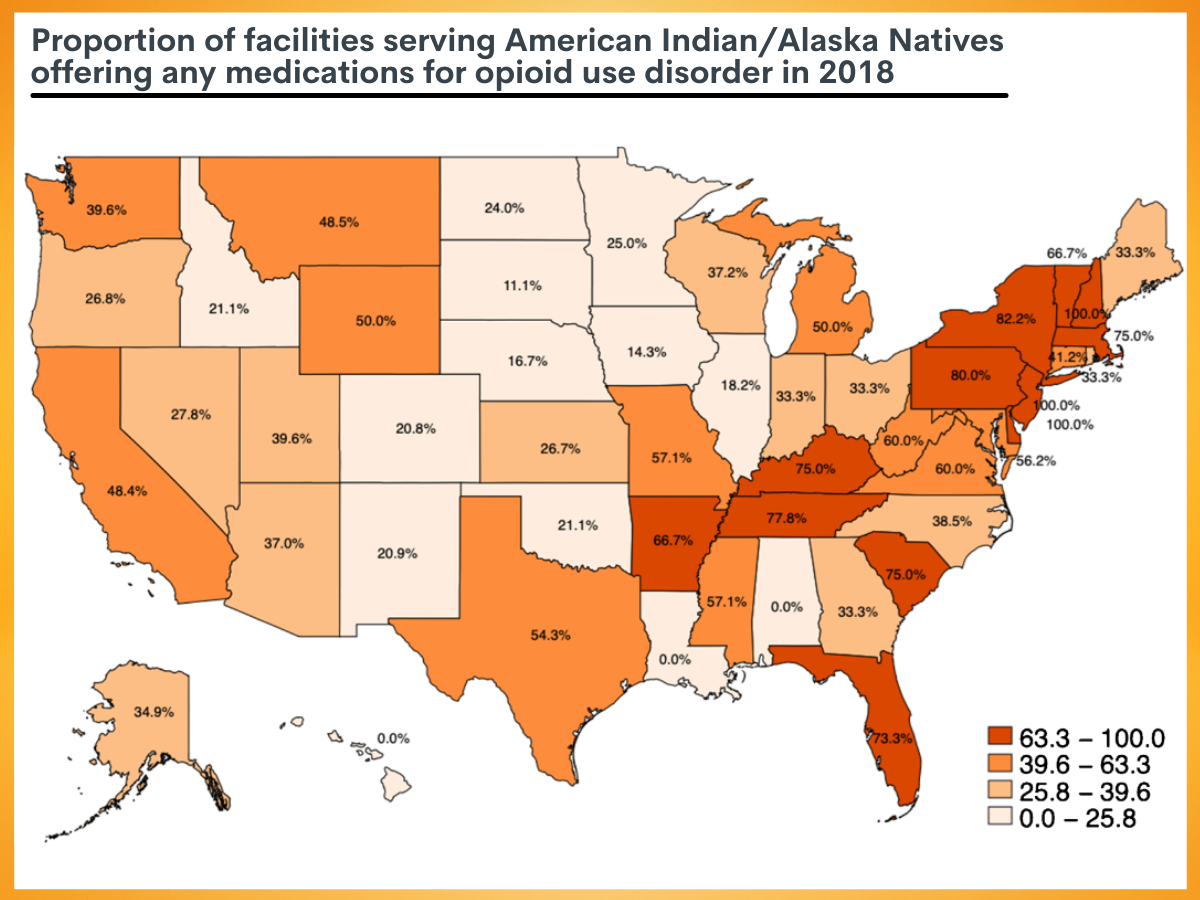
Figure 1. Proportion of facilities serving American Indian/Alaska Natives offering any medications for opioid use disorder in 2018. Figure content taken from Krawczyk et al., 2021.
Use of medication for opioid use disorder among American Indian/Alaska Natives was slightly higher compared to other groups (40.04 % vs. 38.63 %, p = 0.009). However, in non-detoxification settings, American Indian/Alaska Natives had slightly lower utilization rates than other racial groups (44.4 % vs. 46.7 %, p < 0.001), indicating that more American Indian/Alaska Natives are receiving medication for tapering/withdrawal purposes rather than ongoing treatment compared to other racial/ethnic groups. Figure 2 displays geographical differences across states in medication use.
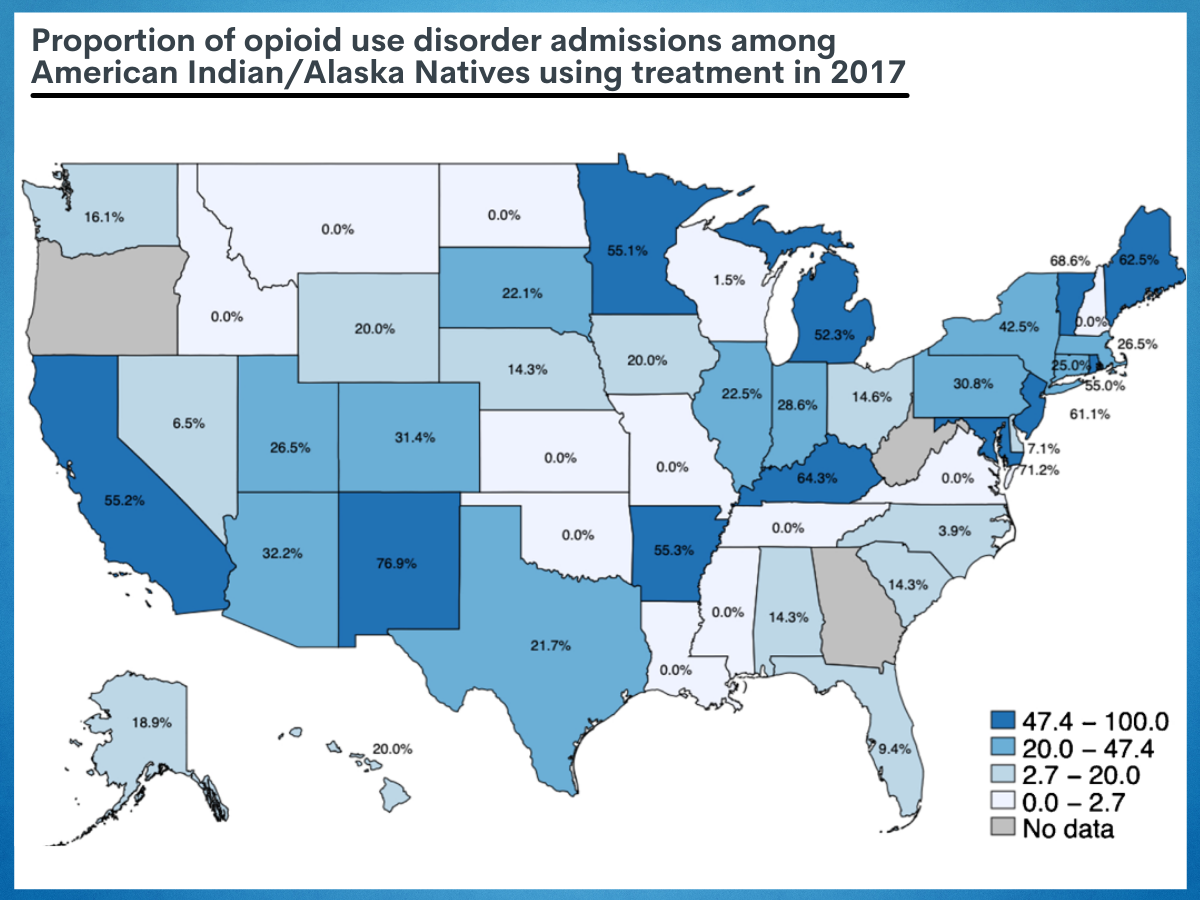
Figure 2. Proportion of opioid use disorder admissions among American Indian/Alaska Natives using treatment in 2017. Figure content taken from Krawczyk et al., 2021.
Factors that disproportionately effect medication use for opioid use disorder among American Indians/Alaska Natives.
A few factors also differed in their association with medication use among American Indians/Alaska Natives compared to other groups. Hispanic ethnic identity was associated with greater odds of utilization among American Indians/Alaska Natives, but not other racial groups.
Unlike other racial groups, more education was not associated with increased odds of utilizing medication for opioid use disorder among American Indians/Alaska Natives.
Unlike other racial groups, unemployment, later age of first use, more frequent use, and comorbid cocaine use were not associated with lower odds of medication receipt among American Indians/Alaska Natives.
There were significant geographic differences in medication use. Among American Indians/Alaska Natives seeking treatment for opioid use disorder, compared to the Midwest, medication use was lower in the Northeast, West, and especially the South. Among other racial groups, medication use was lower in the South and higher in the West compared to the Midwest.
Lastly, only 40% of American Indian/Alaska Natives in specialty care for opioid use disorder receive medication treatment. 22% of specialty treatment facilities serving American Indian/Alaska Natives offer opioid agonist medication.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
American Indians/Alaska Natives had slightly lower rates of using medication for opioid use disorder in non-detoxification settings than other races (44.4 % vs. 46.7 %). This may reflect differences in the facilities where they seek treatment given that 22.4% offered ongoing medication compared to 27.6% that service individuals of other races. Opioid use disorder is a treatable disorder, and when approached using a continuum of care framework that includes medications as opposed to brief episodic medical intervention alone, it can facilitate and increase the chances of treatment engagement and, potentially, ongoing recovery management to address the disorder over time.
A number of factors were investigated for their disproportionate effect on medication use among American Indians/Alaska Natives. Unlike other racial groups, markers of education, unemployment, later age of first use, more frequent use, and comorbid cocaine use were not associated with the receipt of medication for opioid use disorder.
This means that other factors, not all identified here, are more influential on the likelihood of American Indians/Alaska Natives using medication. Hispanic identity was a protective factor among American Indians/Alaska Natives associated with an increased likelihood of medication receipt, unlike other racial groups that also identified as Hispanic ethnicity. The intersectionality of race-ethnicity and the sociocultural benefits it provides appears to be relevant for medication use for opioid use disorder and the lived experience this identity reflects is worth exploring.
The facilities least likely to offer ongoing agonist treatment were ones operated by tribal governments and facilities with staff that spoke Native languages. Research is needed to understand motivations for medication use as ongoing vs. detoxification among patients and providers, cultural values around medication, and how these trends compare among American Indians/Alaska Natives relative to other racial-ethnic groups. Additionally, more research is needed to understand why access to medication for opioid use disorder appears to be reduced in the South for all racial groups and how best to increase access. The importance of tribal affiliation and reservation status will need to be elucidated.
- LIMITATIONS
-
- The datasets used in this study specifically cover treatment that occurs in specialty programs. Treatment that is offered in other settings is not represented.
- The tribal affiliation or reservation status of the American Indians in this study is unknown and may influence the likelihood of access and use of medication for opioid use disorder.
BOTTOM LINE
- For individuals and families seeking recovery: People who identify as American Indians/Alaska Natives and have an opioid use disorder are at high risk for overdose compared to other racial groups. Seeking medication early is likely to yield improved functioning and reduced opioid use, but only about 40% of American Indians/Alaska Natives who seek care will use medication, and only 22% will use ongoing medication. This may be explained in part because the facilities that serve American Indians/Alaska Natives are less likely to offer this type of treatment. Ongoing medication for the treatment of opioid use disorder is considered a safe front-line treatment, and so seeking facilities that offer medications for opioid use disorder will likely facilitate better treatment outcomes.
- For treatment professionals and treatment systems: Many Native Americans and Alaska natives are receiving medications for opioid use disorder for tapering or withdrawal purposes rather than on-going treatment. This may be explained in part because the facilities that serve American Indians/Alaska Natives are less likely to offer this type of support. Medications for opioid use disorder are considered to be the most effective treatments available. Only 22% of American Indians/Alaska Natives who seek care will use ongoing medication. Ongoing medication is a tool to reduce the high per capita overdose rates experienced by this group.
- For scientists: The facilities least likely to offer ongoing agonist treatment were ones operated by tribal governments and facilities with staff that spoke Native languages. Research is needed to understand motivations for medication use as ongoing vs. detoxification among patients and providers, cultural values around medication, and how these trends compare among American Indians/Alaska Natives relative to other racial-ethnic groups. Additionally, more research is needed to understand why access to medication for opioid use disorder appears to be reduced in the South for all racial groups and how best to increase access. The importance of tribal affiliation and reservation status will need to be elucidated.
- For policy makers: Racial equity is high on drug policy agendas. American Indians/Alaska Natives have a high rate of per capita overdose, and this study may have uncovered a path to reduce disparities. The lower utilization of ongoing medication for opioid use disorder may reflect differences in the facilities where they seek treatment, given 22.4% offered ongoing medication compared to 27.6% that service individuals of other races. Evidence-based services delivered equitably go hand in hand.
CITATIONS
Krawczyk, N., Garrett, B., Ahmad, N.J., Patel, E., Solomon, K., Stuart, E.A., & Saloner, B. (2021). Medications for opioid use disorder among American Indians and Alaska natives: Availability and use across a national sample. Drug and Alcohol Dependence, 220, 108512. DOI: 10.1016/j.drugalcdep.2021.108512

