Characterizing Intentional & Accidental Drug Overdose Deaths
In the past decade drug overdose deaths have more than doubled in the US, with prescription opioids contributing substantially to this dramatic increase. This article explores the characteristics of self-inflicted and unintentional drug overdose deaths.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
In the US from 2000–2014, the rate of drug overdose death increased from 6.2 to 14.7 deaths per 100,0000 population. Concurrently, from 1999–2012, the rate of prescription opioid-related deaths more than tripled; in 2012 39% of drug overdose deaths involved a prescription opioid. Because the majority of these deaths are classified as accidental, public health efforts have largely focused on understanding the characteristics of unintentional drug overdose deaths.
However, 12% of drug overdose deaths in 2014 were intentionally self-inflicted (i.e., suicide by drug overdose), with this proportion remaining relatively stable from 2005–2014. Moreover, from 1999–2014, the rate of opioid-related suicide deaths doubled. This study therefore provides critical information about the characteristics of intentional overdose deaths in the US.
HOW WAS THIS STUDY CONDUCTED?
DESIGN: The authors utilized state death records, prescription data (from the North Carolina Controlled Substance Reporting System), and toxicology reports (from the North Carolina Office of the Chief Medical Examiner) to provide a more comprehensive understanding of self-inflicted drug overdose deaths.
- MORE ON STUDY METHODS
-
SETTING: North Carolina, USA
PARTICIPANTS: Individuals dying as a result of drug overdose in North Carolina in 2012.
MEASUREMENT: Each self-inflicted and unintentional drug overdose identified through the death certificate data was queried in the North Carolina Controlled Substance Reporting System to capture prescriptions for controlled substances dispensed to the deceased within 365 days prior to death.
WHAT DID THIS STUDY FIND?
Controlled substance prescription history leading up to drug overdose deaths
- The majority of individuals dying from self-inflicted (79.2%) and unintentional (75.6%) drug overdoses had a prescription for a controlled substance within the year leading up to their death.
- The average number of days between the last dispensed prescription for a controlled substance was 31 days for self-inflicted drug overdose deaths and 45 days for unintentional drug overdose deaths, indicating people dying of overdoses often had contact with healthcare providers shortly before their death.
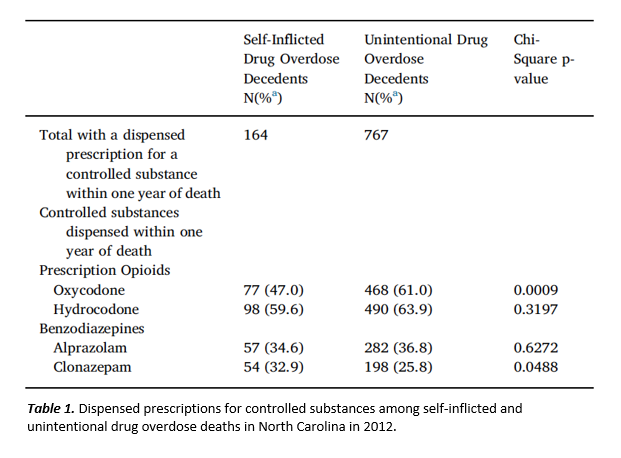
- Also, as shown in the Table 1 below, among self-inflicted drug overdose deaths involving a prescription for a controlled substance within the year leading up to death, approximately half had a dispensed prescription for opiates including hydrocodone (59.6%; e.g. Vicodin), or oxycodone (47.0%; e.g., Oxycontin), and approximately one-third had dispensed prescriptions for benzodiazepines such as alprazolam (34.8%; e.g., Xanax) and clonazepam (32.9%; e.g., Klonopin).
- Comparatively, a significantly higher percent of unintentional drug overdose deaths had a dispensed prescription for oxycodone (61.0%), and a significantly lower percent had a dispensed prescription for clonazepam (25.8%) within one year of death.
Toxicology results in drug overdose deaths
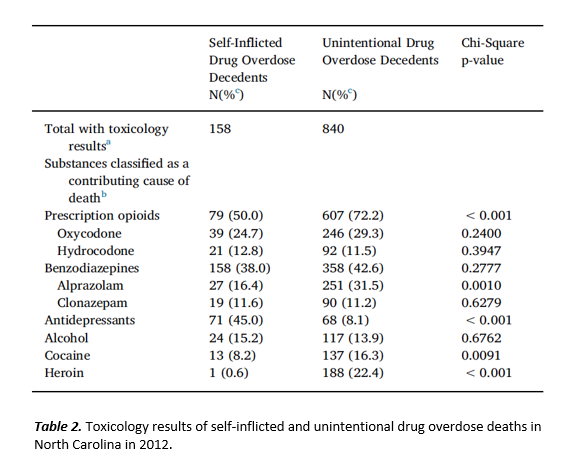
- As shown in Table 2 below, multiple substances were classified as contributing in a primary or additive manner for most self-inflicted (73.4%) and unintentional (70.4%) drug overdose deaths.
- Substances contributing to highest percent of self-inflicted drug overdose deaths were prescription opioids (50.0%), antidepressants (45.0%), and benzodiazepines (38.0%).
- Substances contributing to the highest percent of unintentional drug overdose deaths were prescription opioids (72.3%), benzodiazepines (42.5%), and heroin (22.4%).
- Antidepressants contributed to a significantly higher percent of self-inflicted compared to unintentional drug overdose deaths (45.0% vs. 8.1%).
- Prescription opioids (72.3% vs. 50.0%), heroin (22.4% vs. 0.6%), and cocaine (16.3% vs. 8.2%) contributed to a significantly higher percent of unintentional compared to self-inflicted drug overdose deaths. Benzodiazepines contributed to a similar percent of self-inflicted (38.0%) and unintentional (42.6%) drug overdose deaths.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
While there were some similarities between self-inflicted and unintentional drug overdose deaths, self-inflicted drug overdose deaths differed from unintentional drug overdose deaths in many respects. Most notably, results showed that self-inflicted drug overdose deaths were more likely to involve antidepressants as a contributing cause of death and more likely to involve a controlled substance prescription dispensed in the weeks prior to death, suggesting potential contact with the health care system in the weeks/months leading up to death. Such contacts offer a critical opportunity for health care professionals to identify and intervene on risk factors or signs of distress and potential for self-harm among those receiving prescriptions for controlled substances.
Overall, results from the present study give a more comprehensive understanding of the characteristics of self-inflicted drug overdose deaths, providing valuable information for the development of targeted prevention and intervention strategies, such as prescription monitoring and evidence-based mental health screening. The results also underscore the importance of addressing shared risk factors for mental health disorders, opioid and benzodiazepine use, and self-harm.
- LIMITATIONS
-
- It is possible that deaths recorded in the present study may have been in part a result of prescriptions for controlled substances obtained in states other than North Carolina.
- Toxicology data was not available for North Carolina residents who died out-of-state meaning data were not complete; toxicology reports were available for 76.3% of self-inflicted and 82.8% of unintentional drug overdose deaths.
- Some drug overdose deaths classified by the medical examiner as unintentional may have in reality been self-inflicted.
- It is also possible that there were substances that contributed to overdose deaths reported here that were not screened for by the North Carolina Office of the Chief Medical Examiner, and thus were not reported in the present findings.
BOTTOM LINE
- For individuals & families seeking recovery: Opiates (e.g., oxycodone, hydrocodone) and benzodiazepines (e.g., alprazolam, clonazepam) are heavily implicated in both intentional and accidental drug overdose deaths. Because opiates and benzodiazepines are both sedative hypnotic drugs, they have additive effects when taken together, and thus can dramatically increases the risk of overdose when combined. Naloxone can reverse an opiate overdose, however, when multiple medications/drugs are implicated in an overdose Naloxone is less effective. Immediate medical care is essential in the event of any drug overdose, but especially when a drug combination is suspected.
- For scientists: Results highlight risks associated with prescription medications, and also identify gaps in pharmacotherapy treatment wherein possible risk factors for drug overdose death are being missed. Research is needed on how prescribing practices and access to non-pharmacological psychological care potentially interact to affect overdose risk.
- For policy makers: The problems associated with opiate over prescription are widely appreciated. The present findings provide additional evidence of the impact of prescription opiates in the current opioid overdose crisis, and also highlight risks associated with non-opiate prescription drugs such as benzodiazepines. Prescription monitoring programs can help reduce the quantity and availability of high-risk medications and help reduce the massive public health burden of drug overdose. The fact many individuals died shortly after contact with prescribers suggests a need for better access to counseling and psychosocial support to compliment medical/psychopharmacological treatment, which may be able to provide more comprehensive risk monitoring and psychological support.
- For treatment professionals and treatment systems: Results showed that self-inflicted drug overdose decedents often involved antidepressant medication and controlled substances prescribed in the weeks/months prior to death, indicating contact with the health care system. Such contact offers an opportunity for health care professionals to identify and intervene on risk factors or signs of distress and potential for self-harm among those receiving prescriptions for controlled substances. Results also underscore the importance of addressing shared risk factors for mental health disorders, opioid and benzodiazepine use, and self-harm.
CITATIONS
Austin, A. E., Proescholdbell, S. K., Creppage, K. E., & Asbun, A. (2017). Characteristics of self-inflicted drug overdose deaths in North Carolina. Drug & Alcohol Dependence, 181, 44-49. doi:10.1016/j.drugalcdep.2017.09.014