Compared to methadone, Suboxone is associated with lower mortality but also less time in treatment
Overdose death risk related to opioid use disorder is well documented. Taking opioid agonist medications like buprenorphine, the active ingredient in Suboxone, or methadone is associated with overdose reductions of 50% or more. In this study which compared death rates of those prescribed buprenorphine versus methadone in United Kingdom primary care practices, buprenorphine patients had lower death rates than methadone patients both while receiving and not receiving the medication.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Opioid use disorder increases the risk of premature death (i.e., mortality) 10-fold compared to the general population. Agonist pharmacotherapies for opioid use disorder, which activate opioid receptors in controlled ways, are associated with improved survival rates, decreasing mortality by at least 50%. However, some studies highlight increased mortality risk both in the first month of treatment and in the first month after treatment cessation. High doses of methadone can lead to respiratory depression (similar to that seen in other opioid overdoses). On the other hand buprenorphine (often prescribed in combination with naloxone and referred to by its brand name Suboxone) is a partial agonist that also has greater affinity for opioid receptors than other opioids (apart from fentanyl) which in theory limits the risk of respiratory depression. Thus the mortality risk shortly after starting or stopping agonist pharmacotherapies may vary depending on whether the treatment is buprenorphine versus methadone. By analyzing a large medical database linked to a mortality registry, this study by Hickman and colleagues examines mortality rates within a year of starting either buprenorphine or methadone treatment among primary care patients in the UK.
HOW WAS THIS STUDY CONDUCTED?
This cohort study linked primary care medical records to a national mortality registry over the time period 1998-2014. Participants were more than 11,000 patients aged 15-64 with opioid use disorder who were prescribed either buprenorphine or methadone (those receiving opioids for pain were excluded). Prescription of methadone was more common with 61% receiving this full opioid agonist compared to 39% receiving the partial agonist, buprenorphine. Of note, the popular buprenorphine formulation, Suboxone, was not approved for use in the European Union until 2006. All-cause mortality and drug-related poisoning for the participants were collected from the Office for National Statistics. Patients with buprenorphine or methadone prescription were analyzed at four treatment milestones (first four weeks in treatment, subsequent weeks in treatment, first four weeks after treatment discontinuation, and subsequent weeks after treatment discontinuation). The analyses statistically controlled for medical comorbidity score (based on 17 chronic illnesses), geographical region, benzodiazepine or gabapentin co-prescription (two medications that activate the GABA, leading to relaxing, anti-anxiety or anti-convulsive effects), history of self-harm, alcohol problems, imprisonment or homelessness.
WHAT DID THIS STUDY FIND?
In all participants mortality risk is increased during the weeks after treatment initiation and after treatment cessation.
Compared to methadone or buprenorphine prescriptions after the first four weeks, mortality rates are 3 times higher during the first 4 weeks with such a prescription, but 9 times higher during the first four weeks after no longer receiving such prescriptions. They are 2 times higher after the first four weeks without a prescription.
Across all treatment periods, patients with a buprenorphine prescription had lower mortality rates compared with methadone.
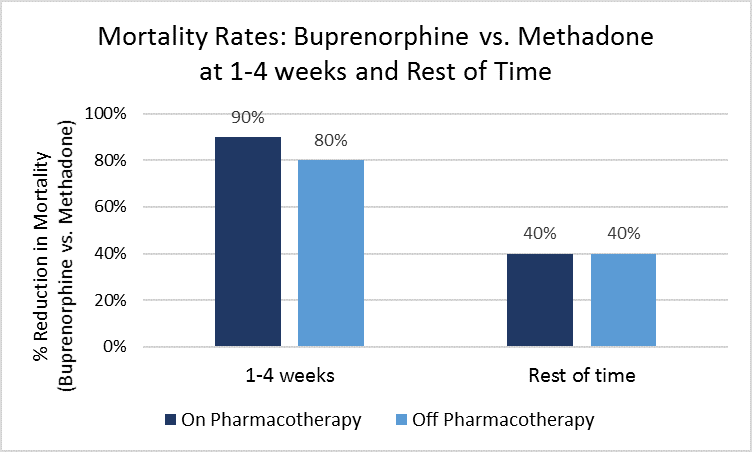
An overall benefit associated with buprenorphine relative to methadone is increased even more during the two periods of highest mortality. During the first 4 weeks of treatment, buprenorphine prescription is associated with 90% lower mortality rates than methadone, and 40% lower after the first 4 weeks. These reduced morality rates associated with buprenorphine hold up when individuals stop receiving pharmacotherapy prescription, too. This may be due to methadone patients having more severe opioid use disorder at the time they started the medication, since they had greater death rates than buprenorphine patients when neither was prescribed the medication. Authors controlled statistically for many factors related to receiving a buprenorphine vs. methadone prescription (e.g., prior overdose, homeless, co-occurring drinking problems, etc.) to try and isolate the difference between buprenorphine and methadone prescription, though these reduced mortality rates for buprenorphine remained even after such statistical control.
Individuals with a buprenorphine prescription had lower mortality rates than those with a methadone prescription. They also had lower mortality rates when no longer prescribed the medication. This suggests methadone patients may have been more severe, placing them at greater risk for death irrespective of whether they received methadone or buprenorphine.
Patients remained on methadone for longer continuous periods of time than on buprenorphine.
The mean duration of a single treatment episode was 363 days for methadone as compared with 173 days for buprenorphine. These durations of treatment were not sufficient to reduce mortality rates relative to no agonist pharmacotherapy prescription.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Despite prescriptions for opioid use disorder agonist pharmacotherapies, patients continue to be vulnerable to premature death, particularly during the first month of treatment and especially during the first month after discontinuing treatment. When comparing the two most common medications to treat opioid disorders, patients taking buprenorphine show significantly lower mortality rates compared with methadone at all time points analyzed, but especially during the two time periods when patients are most vulnerable (transitioning on or off the medication). Though treatment courses on methadone are approximately twice as long as buprenorphine courses, buprenorphine may be more protective in terms of all-cause mortality. It is possible, also, that buprenorphine patients were simply less severe than methadone patients, and this accounted for buprenorphine patients’ lower death rates, despite authors efforts to control for factors which may reflect patient severity to varying degrees (e.g., prior overdose, co-occurring alcohol problems, homelessness, etc.).
One issue also raised here is that, based on the lengths of treatment observed in this sample of UK primary care patients, agonist pharmacotherapy prescription is not associated with reductions in drug overdose and death. Authors suggest that, for example, individuals would require buprenorphine prescription for more than 6 months (202 days) to observe a 25% in drug overdose. Such a finding highlights the importance of treatment, policy, and scientific efforts to enhance pharmacotherapy adherence. Innovative approaches like those that integrate combinations of psychosocial intervention, monitoring, and mobile technologies with agonist prescriptions (see here for example) may help improve the public health benefit of these potentially life-saving medications.
- LIMITATIONS
-
- The subjects in this study were selected based on receiving a methadone or buprenorphine prescription. Then subsequent groups were eliminated (those receiving opioids for pain, doses too low of either medication, outside the age range, etc.). This means that the resulting subject population is presumed to have opioid use disorder although those criteria were not used to directly select the patient population.
- As mentioned above, one confounder not directly analyzed was severity and chronicity of opioid use disorder. However, the finding that patients with a history of prior overdoses, alcohol problems, imprisonment or homelessness were more likely to receive methadone suggests that methadone was used more frequently for more severe opioid use disorder, which could have been associated with their higher death rates, as mentioned above.
BOTTOM LINE
- For individuals and families seeking recovery: Methadone and buprenorphine, the active ingredient in Suboxone, are both shown to help reduce opioid use and opioid-involved overdose deaths. In this study, researchers found buprenorphine patients had lower death rates than methadone patients when prescribed each respective medication, death rates were also lower for buprenorphine patients when they stopped receiving prescriptions. Given this study was not randomized, it is possible that buprenorphine patients were less severely addicted at the time they were started on the medication, which might account to at least some degree for the lower mortality rate in this group. More research is needed to understand pros and cons of buprenorphine versus methadone. In the U.S., for example, individuals must receive methadone from a licensed opioid treatment program whereas they may receive buprenorphine from any physician licensed to prescribe the medication.
- For treatment professionals and treatment systems: Methadone and buprenorphine, the active ingredient in Suboxone, are both shown to help reduce opioid use and opioid-involved overdose deaths. In this study, researchers found buprenorphine patients had lower death rates than methadone patients when prescribed each respective medication, death rates were also lower for buprenorphine patients when they stopped receiving prescriptions. Given this study was not randomized, it is possible that buprenorphine patients were less severely addicted at the time they were started on the medication, which might account to at least some degree for the lower mortality rate in this group. More research is needed to understand pros and cons of buprenorphine versus methadone. Authors also found that in their UK primary care sample, pharmacotherapy durations were insufficient to make a public health difference in opioid-involved overdose and death rates. As there are few empirically supported interventions specifically to target agonist medication adherence (though some are being developed and tested), providers may wish to develop and evaluate their own strategies (e.g., via motivational interviewing or recovery management check-ups) to help maintain pharmacotherapy adherence and treatment engagement more generally.
- For scientists: Methadone and buprenorphine, the active ingredient in Suboxone, are both shown to help reduce opioid use and opioid-involved overdose deaths. In this study, authors found buprenorphine patients had lower death rates than methadone patients when prescribed each respective medication. Death rates were also lower for buprenorphine patients when they stopped receiving prescriptions. Despite authors’ best efforts to isolate the effects of buprenorphine versus methadone, by controlling for propensity score weights, for example, findings suggest that buprenorphine patients’ lower severity may have accounted for their lower overdose and death rates in this study. Studies in other cohorts (this was a UK primary care- based cohort) may help shed light on whether lower death rates in buprenorphine patients are accounted for by partial agonist effects, case mix (i.e., patient characteristics), or some combination of the two. Also, given that pharmacotherapy durations were insufficient to make a public health difference in opioid-involved overdose and death rates, studies that develop, test, and disseminate innovative strategies to enhance agonist pharmacotherapy adherence are areas ripe for future investigation.
- For policy makers: Methadone and buprenorphine, the active ingredient in Suboxone, are both shown to help reduce opioid use and opioid-involved overdose deaths. In this study, authors found buprenorphine patients had lower death rates than methadone patients when prescribed each respective medication, death rates were also lower for buprenorphine patients when they stopped receiving prescriptions. Given this study was not randomized, it is possible that buprenorphine patients were less severely addicted at the time they were started on the medication, which might account to at least some degree for the lower mortality rate in this group. More research is needed to understand pros and cons of buprenorphine versus methadone. Authors also found that in their UK primary care sample, pharmacotherapy durations were insufficient to make a public health difference in opioid-involved overdose and death rates. As there are few empirically supported interventions specifically to target agonist medication adherence (though some are being developed and tested), the field would greatly benefit from financial and legislative support to aid in the development, testing, and dissemination of such strategies.
CITATIONS
Hickman, M., Steer, C., Tilling, K., Lim, A. G., Marsden, J., Millar, T., . . . Macleod, J. (2018). The impact of buprenorphine and methadone on mortality: a primary care cohort study in the United Kingdom. Addiction, 113(8), 1461-1476. doi:10.1111/add.14188

