Office-based Opioid Treatment with Buprenorphine: Insights from the Massachusetts Model
Despite the availability of effective pharmacological interventions for opioid use disorder, less than 24% of individuals receive any medication for their opioid addiction.
One main barrier to access is lack of trained physicians who can prescribe medications such as buprenorphine
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Under the Drug Addiction Treatment Act of 2000, a physician who has received the requisite training, and is consequently waivered, can prescribe buprenorphine to a limited number of patients, with the opportunity to increase that number.
However, uptake of this model has been slow, with less than 5% of physicians becoming waivered by 2014.
As a solution, Boston Medical Center created the Collaborative Care Model of Office-based Buprenorphine Treatment, also known as the Massachusetts Model. This study describes the expansion of this model into community health centers (CHCs) in Massachusetts.
HOW WAS THIS STUDY CONDUCTED?
This study assessed enrollment of community health centers (CHCs) in the Office-based Buprenorphine Opioid Treatment Collaborative Care Model (STATE OBOT-B) program beginning in 2007.
The goal of this program was to increase access to treatment among the communities of the community health centers (CHCs).
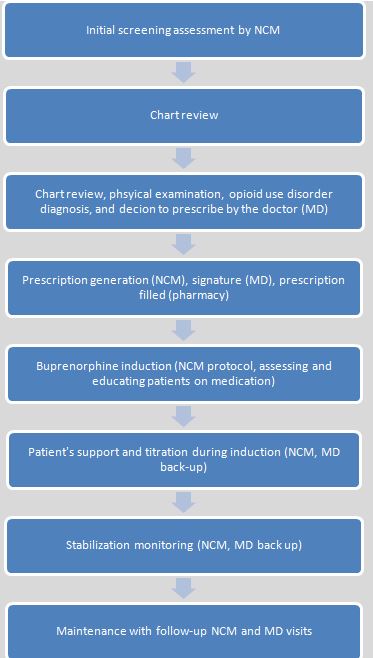
Buprenorphine “induction” refers to the medically-monitored initiation of treatment and “titration” refers to adjustment of medication to provide a therapeutic effect while minimizing adverse reactions.
Community health centers (CHCs) were required to complete patient reporting forms at three time points: enrollment, quarterly during enrollment in the program, and at disenrollment (i.e., discharge). CHCs also provided weekly reports with program-related data. This descriptive study includes information on the number of CHCs enrolled, number of physicians participating at CHCs, annual active admissions, and duration of treatment between August 2007 and December 2013.
WHAT DID THIS STUDY FIND?
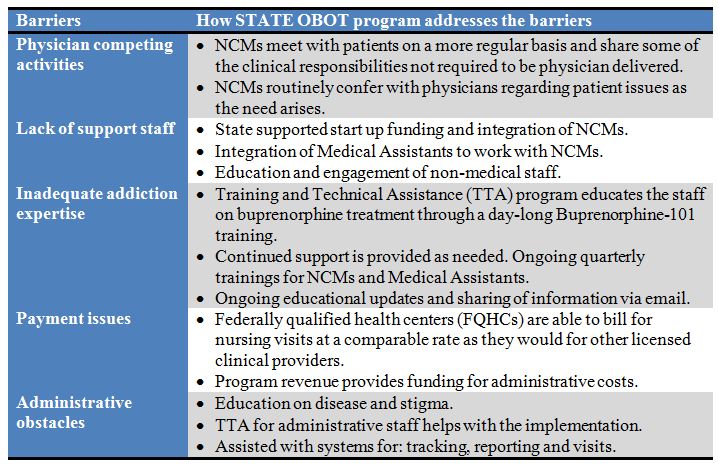
Nineteen Community health centers (CHCs) enrolled in the STATE OBOT-B program between 2007 and 2013. Of the 19 enrollees, five returned the grant contract within the first 3-16 months because they were unable to use funds sufficiently and meet caseload requirements for reasons such as lack of administrative support and difficulty recruiting NCMs. Among the 14 remaining CHCs, annual admissions increased from 178 to 1210 over this timeframe. Half of these sites hired additional NCMs (the grant only required and funded one full-time NCM) to increase their capacity to treat more patients.
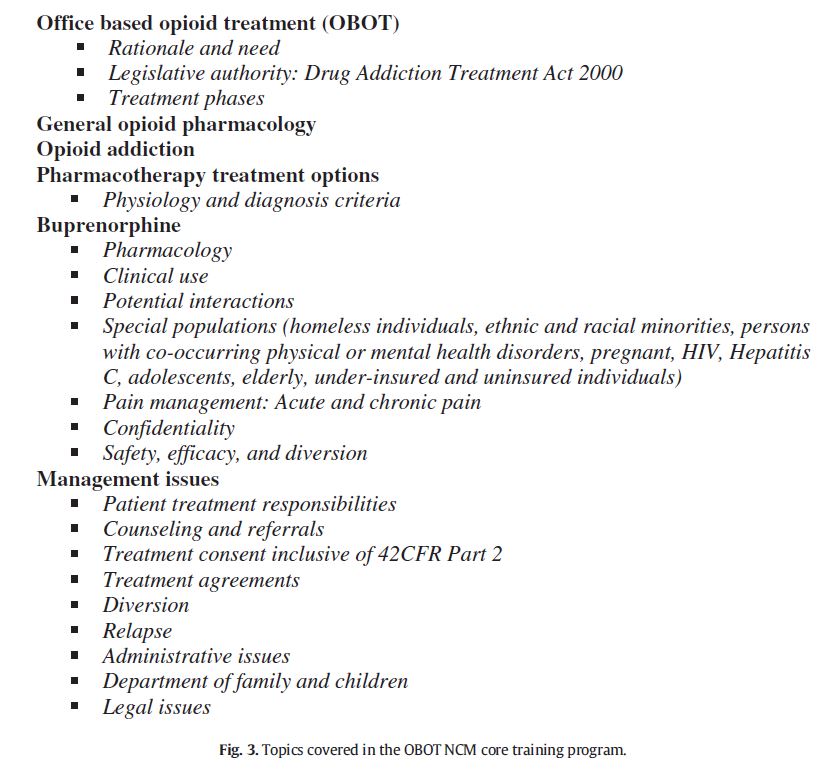
Before the initiation of the STATE OBOT-B program, 24 physicians were waivered. This number increased to 114 by 2010. By 2013, two thirds of enrolled patients remained in treatment for more than 12 months. Patients were largely white (73%), male (63%), between ages 21 to 39, and unemployed (66%). Almost 90% of NCMs “strongly agreed” on a 5-point Likert scale that the training sessions were helpful.
This study provides information on implementation and utilization of an office-based buprenorphine care delivery model. The authors used the ADAPTS implementation science model which included defining steps for assessment, deliverables, and sustainability to explain the implementation of the STATE OBOT-B program.
This descriptive study highlights the need to think critically about barriers to adopting effective interventions, addressing those barriers, measuring and evaluating programs to do so, and considering how to maintain/sustain programs over time given limitations (e.g., reimbursement and funding). The promising initial results from this study suggest that this model may be worth evaluating further and potentially implementing elsewhere.
WHY IS THIS STUDY IMPORTANT
Medication-assisted treatment exists in several forms, but is of no use to a patient who cannot access it.
The development and scaling up of models to enhance the delivery of treatment is important for addressing this issue.
By incorporating this model into Community health centers (CHCs), marginalized individuals such as the homeless and uninsured can initiate treatments they otherwise would be unable to access.
Of note: This model also relies on Nurse Care Managers to act as the primary point of contact for patients and liaison between the patient and their physician. Since Nurse Care Managers carry out multiple steps in the care cascade, more patients can access treatment since they do not need to meet with physicians at every visit.
This model for office-based buprenorphine delivery relies heavily on Nurse Care Managers for many components of care. This study shows that it is feasible to hire Nurse Care Managers to handle high patient caseloads so access to treatment is not limited by the number of prescribing physicians on staff. With the aid of a medical assistant, Nurse Care Managers in this program were managing 125+ patients.
- LIMITATIONS
-
- This study describes a program implemented in Massachusetts so there may be other unknown factors such as funding and acceptance of medication-assisted treatment that influence its adoptability in other states.
- Additionally, this study did not assess the effectiveness of this office-based buprenorphine program, so despite increasing enrollment, it is unknown how patients responded to and benefited from treatment.
NEXT STEPS
More research is needed to evaluate the effectiveness of this model in Massachusetts and to determine if this approach can be implemented in other states.
BOTTOM LINE
- For individuals & families seeking recovery: If you feel buprenorphine may be helpful, seek out a treatment facility that can determine your eligibility and determine the best course of action. If your current physician is unable to prescribe buprenrophine, this treatment locator by SAMHSA (Substance Abuse and Mental Health Administration) allows users to filter results by providers who use buprenorphine in treatment.
- For scientists: Research is needed to evaluate the effectiveness of this model across several settings including but not limited to community health centers in Massachusetts to determine how it impacts the trajectory of patient opioid use.
- For policy makers: The Massachusetts Model is a feasible method for implementing buprenorphine treatment in the office-based setting. If future evidence suggests that it is effective, more funding could help scale up this program among other providers in Massachusetts and other states.
- For treatment professionals and treatment systems: A delivery model such as the one described in this study may be a potential option for community health centers to follow. While it may require hiring NCMs and completing training for physicians to become waivered, it can help address a growing public health issue that affects many individuals.
CITATIONS
LaBelle, C. T., Han, S. C., Bergeron, A., & Samet, J. H. (2015). Office-Based Opioid Treatment with Buprenorphine (OBOT-B): Statewide Implementation of the Massachusetts Collaborative Care Model in Community Health Centers. J Subst Abuse Treat. doi:10.1016/j.jsat.2015.06.010

