Using Opioid Use Disorder Medication Without a Prescription: How common is it and what are the reasons behind it?
Buprenorphine is a lifesaving treatment for opioid use disorder, but its use by individuals without a prescription (diverted use) and motivations for this type of use are not fully understood. The current study examines buprenorphine use among treatment seekers with opioid use disorder. Among those who used diverted buprenorphine, 80% said they would obtain a legitimate prescription if they had easier access, but 50% had, at some point, used it to get high.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Buprenorphine is a federally approved medication to treat opioid use disorder in the United States. Diversion (the transfer of a prescribed controlled substance from the prescription holder to an individual for whom it was not intended) of buprenorphine is a concern among treatment seekers, but reasons for diversion of buprenorphine are not entirely clear. To address this gap in the literature, the current study assessed prevalence of diverted and prescribed buprenorphine use among opioid use disorder treatment seekers, their motivations for buprenorphine use patterns, and the role that barriers to treatment play in diverted use.
HOW WAS THIS STUDY CONDUCTED?
The authors analyzed survey-based data from adults who had participated in a larger investigation. Individuals initially participated in the Survey of Key Informants’ Patients (SKIP), an anonymous nationwide survey of adults entering treatment for opioid use disorder that is part of a large scale program collecting data on opioid misuse and diversion (i.e. Researched Abuse, Diversion, and Addiction-Related Surveillance (RADARS) System).
- READ MORE ON STUDY METHODS
-
A portion of the individuals who completed the SKIP and were willing to give up their anonymity also completed a series of 5 online surveys (the Researchers and Participants Interacting Directly (RAPID) Program). Of the 21,087 participants who completed the SKIP survey, 303 participated in the online surveys. All participants were diagnosed with substance abuse or dependence (determined with the Diagnostic and Statistical Manual of Mental Disorders (DSM, 4th edition)), reported opioids (prescription opioids or heroin) as their primary drug, and were seeking opioid agonist treatment. Online surveys addressed prescribed buprenorphine use, diverted buprenorphine use, barriers to accessing buprenorphine, and participant demographics. The authors were interested in characterizing buprenorphine use, reasons for and sources of diverted buprenorphine, routes of administration, and barriers to treatment. The majority of participants were 25-44 years of age (72%), female (55%), Caucasian (90%), and employed (71%), from rural/suburban locations (57%), and covered by private health insurance or Medicaid/Medicare (64%).
WHAT DID THIS STUDY FIND?
Lifetime History of Buprenorphine Use
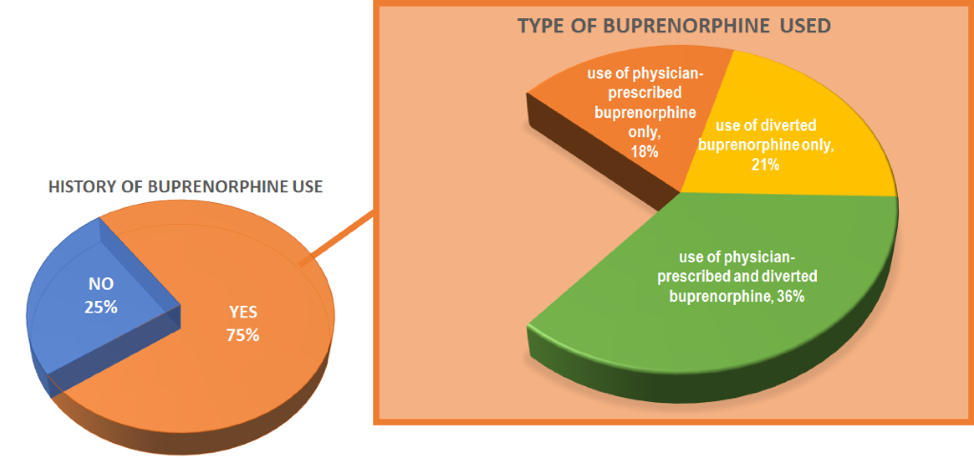
- 75% of all participants had a history of buprenorphine use
Prescribed Buprenorphine Use
- 54% of all participants had a history of using prescribed buprenorphine. Among them:
- 38% were not abstinent while taking their prescribed buprenorphine
- 32% had used their prescribed buprenorphine in a non-prescribed way
- 33% had given away, sold, or traded at least some of their prescribed buprenorphine
- 63% stopped taking their prescribed buprenorphine
- Common reasons for stopping buprenorphine included 1) choosing to stop seeing their doctor (33%), 2) losing the ability to visit or pay for their doctor’s appointments or prescriptions (25%), and 3) other (28%, e.g., going to treatment, switching to methadone, viewing buprenorphine as a crutch).
Diverted Buprenorphine Use
- 58% of all participants had a history of using diverted buprenorphine. Among them:
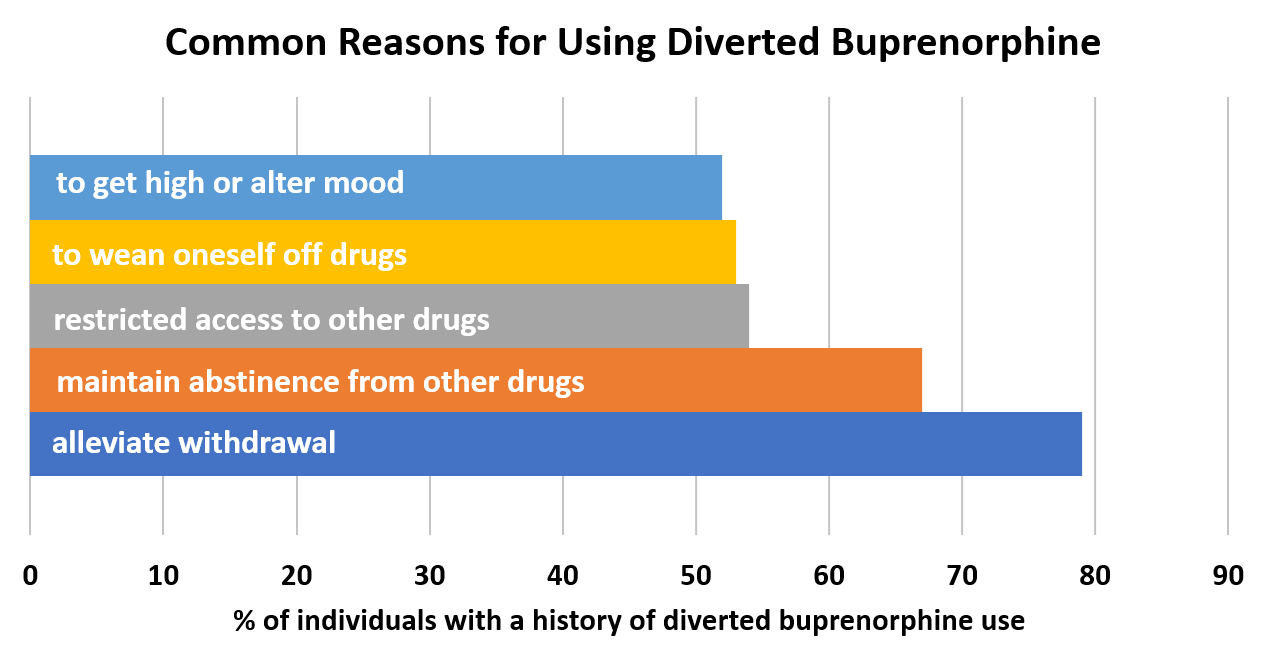
- Less than 5% said buprenorphine was their drug of choice or thought it gave a better high than other drugs
- Diverted buprenorphine was most commonly obtained through a dealer or on the street (84%), or from a friend/relative (71%).
- The majority of participants reported taking buprenorphine at least once per day (63%) by dissolving it under the tongue (90%).
- About one-quarter of participants had a history of snorting, swallowing, and injecting it.
- Reasons for using these means commonly involved achieving a ‘high’
Barriers to Buprenorphine Access
- Problems finding a doctor who can prescribe buprenorphine and the high costs associated with obtaining a prescription were common barriers to access among those who had used diverted buprenorphine (33%) and prescribed buprenorphine (38%).
- 81% of participants who used diverted buprenorphine said they would be encouraged to get a prescription and stop seeking diverted buprenorphine if it were easier to access a buprenorphine-prescribing doctor.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study suggests that use of diverted buprenorphine is prevalent among individuals seeking treatment for opioid use disorder. Importantly, diverted buprenorphine was commonly used for therapeutic purposes, and about 4 out of 5 of those who had used diverted buprenorphine reported that increased access to this medication would encourage them to obtain a legal prescription. Restricted access to buprenorphine-prescribing doctors and the high cost of obtaining a prescription remain commonly perceived barriers to getting buprenorphine.
Cost was indicated as a barrier, despite the fact that the majority of participants reported having health insurance. A recent study suggested that physicians prefer cash-paying patients to Medicaid paying patients, with method of payment being the second largest factor in deciding whether to start buprenorphine treatment in a patient. Providing additional clinical resources and streamlining the Medicaid reimbursement process may help to reduce clerical burdens on prescribers. Still, cost also appears to play a role in prescription users’ ability to continue treatment and further study is needed to determine the needs of physicians and patients to limit cost as a barrier. Regarding access to prescribers, physicians must obtain waivers to prescribe buprenorphine and can treat a limited number of patients at a given time, with certifications having a 30-, 100-, or 275- patient limit. A limited number of doctors have waivers and, the majority (73%) of those who do, have a 30-patient limit with many prescribing below their maximum patient allowance. As such, opioid use disorder prevalence far exceeds buprenorphine treatment capacity. Physicians may be reluctant to obtain waivers and prescribe buprenorphine due to concerns about diversion, Medicaid reimbursement, the legal risks of prescribing, or limited knowledge of opioid use disorder treatment. To enhance physician willingness to prescribe buprenorphine and treat opioid use disorder, providing additional training and educational resources may be warranted.
Although reducing these barriers to buprenorphine access may encourage therapeutic use through legal means, it also has the potential to increase diverted use for non-therapeutic reasons. About half of the individuals who had used diverted buprenorphine said they had at one time or another used it to get high or alter their mood. Therefore, increasing access to this medication could make it more available for individuals to misuse. However, non-therapeutic use seems to be an issue regardless of whether or not an individual has a prescription; non-therapeutic use of prescribed buprenorphine was reported by over a quarter of legal prescription users. Moreover, few individuals reported buprenorphine as their drug of choice.
Given the limitations inherent in this study’s self-reported, online survey design, it is unclear exactly how much confidence can be placed in the findings regarding diverted buprenorphine. However, this study provides an important foundation for future research. Furthermore, from a broader public health perspective, the consequences of increasing buprenorphine access are likely to be generally positive. Buprenorphine’s risk for harm (overdose) is relatively low in individuals with opioid use disorder and increased access to this medication may help individuals who are seeking it for therapeutic purposes to achieve stable legal treatment with potentially better outcomes. So, even despite some diversion, there is likely still to be a net public health gain. Further research characterizing motivations for diverted use and perceived barriers to buprenorphine access will ultimately help physicians better understand their patients’ needs and help guide the decisions of policy makers.
- LIMITATIONS
-
- Only 303 of the 21,087 individuals who participated in the nationwide SKIP also participated in the current study’s survey. Furthermore, all participants were seeking opioid agonist treatment. Therefore, it is unclear whether these findings are representative of the broader opioid use disorder population or if they would translate to all opioid agonist treatment seeking patients.
- The survey included open-ended questions that required a written response and it is unclear how prevalent some of the example responses were. Further study is needed to gain a more detailed quantitative understanding of motivations and reasons for diverted use.
- Survey questions regarding motivations behind the use of diverted buprenorphine concerned lifetime motivation without consideration of the frequency or trajectories of those motivations in a given individual. Therefore, it is unclear how often individuals used diverted buprenorphine for therapeutic reasons or non-therapeutic reasons. Further research is needed to inform whether non-therapeutic use is a frequent occurrence among individuals using diverted and prescribed buprenorphine.
BOTTOM LINE
- For individuals & families seeking recovery: Medications that treat opioid use disorder, including buprenorphine, provide significant benefits to recovering individuals, particularly with their ability to help stop illicit opioid use. However, buprenorphine use by individuals without a prescription (diverted use) and motivations for this type of use are not fully understood. This study suggests that diversion is common and, although use of diverted buprenorphine can be for non-therapeutic reasons, it is also commonly used to self-treat withdrawal and maintain abstinence. Increased access to this medication may encourage individuals to obtain it legally. Given the limitations of this study, additional research is needed. Nonetheless, buprenorphine is a lifesaving medication and increased access to it may help individuals who are seeking it for therapeutic purposes.
- For scientists: Pharmacotherapy for opioid use disorder is a proven treatment that saves lives and increases recovery rates. However, this study suggests that diverted buprenorphine use is common among treatment seekers, both for therapeutic and non-therapeutic reasons. It also suggests that increased access to buprenorphine could encourage patients to seek it through legal means. Importantly, this study did not address the frequency with which individuals used diverted buprenorphine for therapeutic and non-therapeutic reasons. Nationally-representative studies that address the frequencies of therapeutic and non-therapeutic use, and their temporal occurrence over the course of use trajectories are needed to fully understand diverted buprenorphine use and to inform clinical practice and policy.
- For policy makers: Medications that treat opioid use disorder, including buprenorphine, provide significant benefits to recovering individuals, particularly with their ability to help stop illicit opioid use. However, the use of diverted buprenorphine among opioid use disorder treatment seekers is common. Using this diverted medication for therapeutic reasons was common and individuals indicated that they would be more likely to seek out a legal prescription if they had increased access to it. Although diverted buprenorphine was also used for non-therapeutic reasons, it is unclear how often individuals used it for this or other reasons. Despite the limitations of this preliminary study and the need for additional research, buprenorphine’s risk for harm (overdose) is relatively low in individuals with opioid use disorder and increased access to this medication may help enhance opioid and other recovery outcomes. Addressing common barriers to treatment, including restricted access to buprenorphine-prescribing doctors and the high cost of obtaining a prescription might help opioid use disorder patients get the treatment they need. This is likely to yield a high net publc health benefit.
- For treatment professionals and treatment systems: Buprenorphine provides significant benefits to individuals recovering from opioid use disorder. Despite its benefits, diversion of this medication is a concern. Although diverted buprenorphine may be used for non-therapeutic purposes, a significant proportion of individuals use it to self-treat withdrawal symptoms and other health consequences of opioid use disorder. Expanding access to buprenorphine treatment may encourage individuals to get a legal prescription and stop seeking diverted buprenorphine. Increasing the number of doctors with buprenorphine-prescribing waivers, taking on the maximum number of patients permitted by a given waiver, and helping patients to obtain treatment at lower costs could substantially aid our ability to reach a greater number of individuals who want treatment but may not have the resources to do so.
CITATIONS
Cicero, T. J., Ellis, M. S., & Chilcoat, H. D. (2018). Understanding the use of diverted buprenorphine. Drug and Alcohol Dependence, 193, 117-123.

