Looking at the impact of PTSD on individuals with heroin use disorder 11 years after treatment
Disproportionately high rates of post-traumatic stress disorder have been documented among people with heroin use disorder. This co-occurrence has been associated with a worse clinical profile compared to those with heroin use disorder alone. This unique longitudinal study examined 11 year outcomes following treatment for heroin use disorder focusing on whether individuals initially diagnosed with post-traumatic stress disorder fared worse over time.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
More than 2 million people in the US have an opioid use disorder, and millions more misuse opioids. Among people in treatment for heroin use disorder, the prevalence of post-traumatic stress disorder (PTSD) has been estimated to be as high as 66%. Some studies have found the harms associated with co-occurring PTSD and heroin use disorder include earlier age of addiction onset, longer durations of addiction, poorer educational and occupational functioning, more polydrug use, poorer physical and mental health. At the same time, other studies have found no outcome differences between individuals with, or without, PTSD. Further, almost no studies have investigated the association between PTSD and long-term recovery, knowledge which is important to inform both treatment planning as well as ongoing health services planning.
HOW WAS THIS STUDY CONDUCTED?
The authors conducted an observational longitudinal study in 19 agencies treating heroin use disorder using medication maintenance programs (i.e., methadone/buprenorphine), “drug free” residential rehabilitation (i.e., no medications), detoxification programs, and 80 people from syringe programs in the greater Sydney region of Australia.
- READ MORE ON STUDY METHODS
-
The baseline phase was conducted in 2001.Results showed high levels of overdose history, injection-related health problems, and mental disorder. 615 mostly treatment seeking adult participants were assessed on their heroin use, physical health, mental health, depression, PTSD, employment, trauma exposure, overdose, imprisonment, and suicide attempts at baseline, 2 years, and 11 years following intake into the study. The majority were re-interviewed 11 years later (70%).
WHAT DID THIS STUDY FIND?
Individuals with current PTSD (i.e., met diagnostic criteria in the past 12 months) or former PTSD (met diagnostic criteria in the past but showed no symptoms in the past 12 months) had a poorer clinical profile at baseline. Despite showing similar levels of improvement compared to those without a history of PTSD in all outcome domains across the 11 year follow-up, those gains were not large enough to close the gap observed at baseline for certain outcomes. Specifically, PTSD was associated with consistently higher levels of major depression, attempted suicide, subsequent trauma exposure, and poorer occupational functioning (i.e., employment) across the 11 year follow-up.
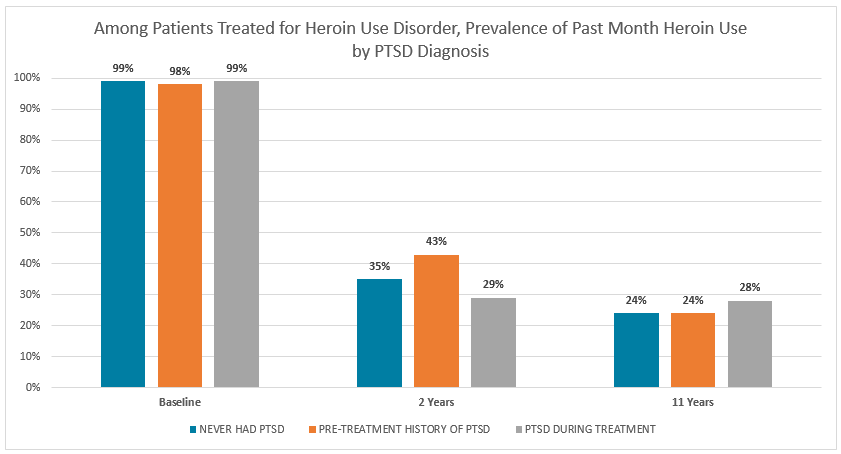
Notably, the proportion of participants who used heroin in the past month, had a heroin use disorder, or the longest reported period of abstinence did not differ according to baseline PTSD status nor were there any significant between group differences at the 11 year follow-up. A significant reduction in the proportion reporting heroin use and meeting criteria for a heroin use disorder occurred for the entire cohort between baseline and the 2 year follow-up, and between the 2 and 11 year follow-up. Although other past month drug use decreased between baseline and the 2 year follow-up, increases were observed between the 2 year and 11 year follow-up.
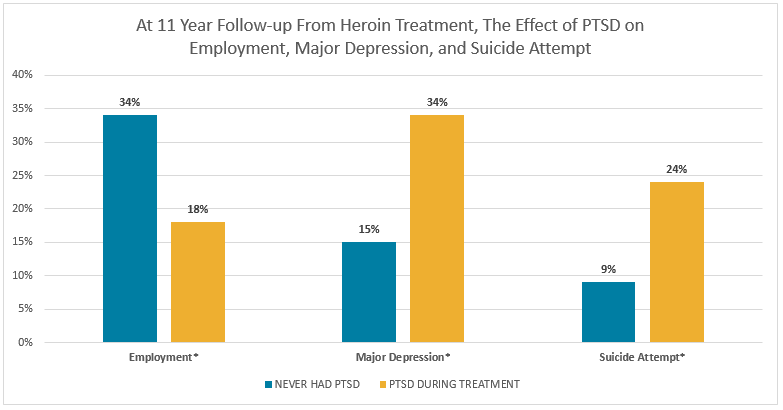
*Significant difference
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study is important because it may be the first to examine the association between PTSD and long-term recovery from heroin use disorder, although US studies have shown other similarities among those with, and without, PTSD. Findings from this research suggest that for individuals with PTSD, reductions in heroin use and heroin use disorder following treatment can be sustained over the long-term at rates equivalent to those without PTSD.
The psychological and occupational impairments associated with co-occurring heroin use disorder and PTSD (compared to PTSD alone) including major depression, attempted suicide, subsequent trauma exposure, and poor occupational functioning were more severe at baseline and persisted over the 11 years despite making gains. This finding indicates that policies and interventions targeted towards individuals recovering from heroin use disorder and PTSD should utilize approaches that will increase employment, reduce depression and suicidal thoughts, and prevent future exposure to traumatic events. PTSD impacts major areas of functioning and is difficult to treat. More effective interventions are needed for this challenging group of patients to address psychosocial functioning and quality of life independent of heroin use.
- LIMITATIONS
-
- Treatment modality (medication maintenance, residential rehabilitation, or medical detoxification) was statistically controlled for but not tested for interactions. Therefore it is unknown if heroin use outcomes varied (i.e., were more or less successful) according to treatment modality. Given the macro level of data collection and the many different treatment options participants may have used over the 11 years, questions regarding the best treatment modality for heroin use disorder should not be inferred from this data.
- This study relied on self-report measures so heroin use was not verified with biological specimens. While a body of literature has found self-reported drug use to be mostly reliable, this reliability in self-report is obtained when individuals are informed that they may have to submit a biological specimen.
BOTTOM LINE
- For individuals & families seeking recovery: This 11 year follow-up study found that treatment seeking individuals recovering from co-occurring heroin use disorder and PTSD, compared to heroin use disorder alone, reported similar reductions in past month heroin use and had similar proportions of individuals meeting criteria for an ongoing heroin use disorder. Individuals recovering from co-occurring heroin use disorder and PTSD (compared to heroin use disorder alone), however, had more severe functional impairments which persisted over the 11 years despite making many gains. If you or someone you know suffers from co-occurring heroin use disorder and PTSD, over time they may be able to reduce their heroin use to levels comparable to those without PTSD, but may need to seek additional resources or knowledge for issues related to employment, suicidal thoughts, depression, and coping with or avoiding subsequent trauma exposure.
- For scientists: This study shows the impact of PTSD on long term recovery from treated heroin use disorder. Remarkably, after 11 years the heroin use outcomes were equivalent between those with and without PTSD. There is a need to identify how to increase occupational functionality associated with co-occurring heroin use disorder and PTSD. Further, research to address suicide attempts, depression, and subsequent trauma exposure could help these individuals make a fuller recovery over and above heroin use alone that may help improve quality of life and functioning more generally.
- For policy makers: This study has shown that reductions in heroin use and heroin use disorder achieved through treatment can be sustained over the long-term, even in the presence of co-occurring PTSD. Yet occupational impairments (i.e., employment) and psychological impairments (i.e., depression, suicide attempts, and subsequent trauma exposure) were persistent among those with PTSD compared to those without. Given the high rates of PTSD among people recovering from heroin use disorder, policies and research dedicated to improving the quality of recovery is a worthy investment for individuals and the communities they support.
- For treatment professionals and treatment systems: Over the long term (i.e., 11 years) individuals recovering from heroin use disorder can reduce heroin use and heroin use disorder at a rate similar rate to those with and without PTSD. Impairments such as depression, suicide attempts, employment as a major source of income, and subsequent trauma exposure are persistent compared to those compared to those without PTSD and should be screened for, monitored, and when necessary, addressed as part of a comprehensive treatment and recovery plan.
CITATIONS
Mills, K.L., Marel, C., Darke, S., Ross, J., Slade, T., & Teesson, M. (2018). The long-term impact of post traumatic stress disorder on recovery from heroin dependence. Journal of Substance Abuse Treatment, 89, 60-66.

