Lost in Translation: Does regular misuse of prescription opioids affect one’s ability to understand others’ emotions?
Opioids pose a major public health problem, but little is known about the consequences of prescription opioid misuse on cognition. This study examined classical cognitive functions, like attention and memory, as well as social cognitive functions, like the ability to read others’ emotions, in individuals with prescription opioid misuse.
Opioids pose a major public health problem, but little is known about the short-term cognitive consequences of regular non-medical prescription opioid use (referred to here as prescription opioid misuse). Classical cognitive functions (e.g., memory, attention) and social cognition abilities (e.g., reading emotions in others, empathizing with others‘ emotions) have the potential to impact daily functioning and quality of life. For example, memory is essential for the acquisition and retention of newly learned skills and social cognition is needed for healthy social interactions and relationships. Identifying whether prescription opioid misuse has long-term effects on these functions has important implications for treatment and recovery. To investigate the direct effects of prescription opioid misuse, the current study assessed classical cognitive functions and social cognitive functions in individuals with current prescription opioid misuse, relative to healthy controls without a history of opioid use (i.e. opioid-naïve).
HOW WAS THIS STUDY CONDUCTED?
Researchers from the University of Zurich and University of Munich conducted a quasi-experimental, cross-sectional study, whereby two groups of adults were recruited, including 23 individuals with current prescription opioid misuse and a comparison group of 29 opioid-naïve individuals, and assessed on cognitive functioning.
- READ MORE ON STUDY METHODS
-
Individuals with prescription opioid misuse reported non-medical use over the last 6 months, and did not have a history of heroin dependence (determined with the Diagnostic and Statistical Manual of Mental Disorders (DSM, 4th edition), intravenous opioid use, or chronic pain disorder.
Opioid-naïve controls had no history of drug/alcohol dependence or opioid misuse. The prescription opioid misuse and control participant groups were matched for sex, age, education, and smoking status (cigarette smoker vs. non-smoker). All participants provided information regarding their substance use histories, provided urine and hair samples to confirm recent drug use, and completed neuropsychological tests that examine various aspects of classical cognition and social cognition. Social Cognition was assessed with two tests: (1) The Multifaceted Empathy Test measures cognitive empathy (ability to recognize others’ emotions) and emotional empathy (ability to subjective experience others’ feelings). Participants are presented with images of people in specific negative and positive emotional states. Participants rate empathetic concern and arousal for each image, providing measures of emotional empathy. Participants are also asked to indicate how they think the person in the image is feeling(cognitive empathy). (2) The abbreviated version of the Comprehensive Affect Test System was used to assess auditory and visual emotion recognition, and requires the participant to identify which one of six basic emotions is being expressed in faces and voices. The authors also used cognitive empathy scores from each of these tasks to create a global cognitive empathy score (overall ability to recognize emotions). Trait empathy (self-ratings of emotional and cognitive empathy) was also assessed with the Interpersonal Reactivity Index, a self-report questionnaire. Classical Cognition was assessed with a series of cognitive tasks and scores from these tasks were used to create overall performance scores for 4 areas of cognitive function: (1) attention(ability to focus on incoming information to achieve goal directed behaviors), (2) working memory (ability to hold onto incoming information and manipulate it in short-term memory), (3) declarative memory (the ability to recognize or recall newly presented information after a short delay), and (4) executive function (ability to adjust tactics for handling new situations or cues in the environment and implement purposeful behaviors to achieve an ultimate goal).
The study was conducted in Germany and all tasks were administered in the German language. Substance use disorder diagnoses among individuals with prescription opioid misuse (determined with the Diagnostic and Statistical Manual of Mental Disorders (DSM, 4th edition) included 74% with opioid dependence, 13% with alcohol dependence, 3% with cannabis dependence, 9% with amphetamine dependence, and 4% with cocaine dependence. On average, the prescription opioid misuse group had 3 years of non-medical use and used opioids about 4 times per week. The prescription opioid misuse group was asked to not take opioids on the day of testing, but individuals were allowed to take a very small dose if needed, to avoid withdrawal and prevent its influence on cognitive performance. Relative to controls, the prescription opioid misuse group showed higher scores on an attention-deficit hyperactivity disorder questionnaire and reported smoking almost twice as many cigarettes per week.
WHAT DID THIS STUDY FIND?
Individuals with prescription opioid misuse showed deficits in cognitive empathy (understanding and reading others’ emotions), but not emotional empathy (subjective experience of others’ feelings). Deficits in classical cognition were also observed, but only for specific cognitive functions.
Social Cognition
The prescription opioid misuse group performed worse than controls on measures of cognitive empathy, as assessed by the Multifaceted Empathy Test and the Comprehensive Affect Test System. Global cognitive empathy scores confirmed this impairment in the prescription opioid misuse group. Whereas recognition of positive emotions (happiness & surprise) was specifically compromised, negative emotion recognition was not. Conversely, the prescription opioid misuse and control groups performed similarly on the Multifaceted Empathy Test for measures of emotional empathy and self-reported trait empathy did not differ between groups.
Classical Cognition
The prescription opioid misuse group showed deficits in attention and declarative memory (recognizing or recalling information) relative to controls, but these groups showed similar abilities in the domains of working memory and executive function.
Factors Influencing Function
In individuals with prescription opioid misuse, higher levels of drug metabolite found in hair samples, indicativeof higher opioid doses, were associated with poorer global cognitive empathy and worse declarative memory. In addition, better executive functioning was associated with better cognitive empathy, but cognitive empathy deficits persisted when controlling for executive abilities.
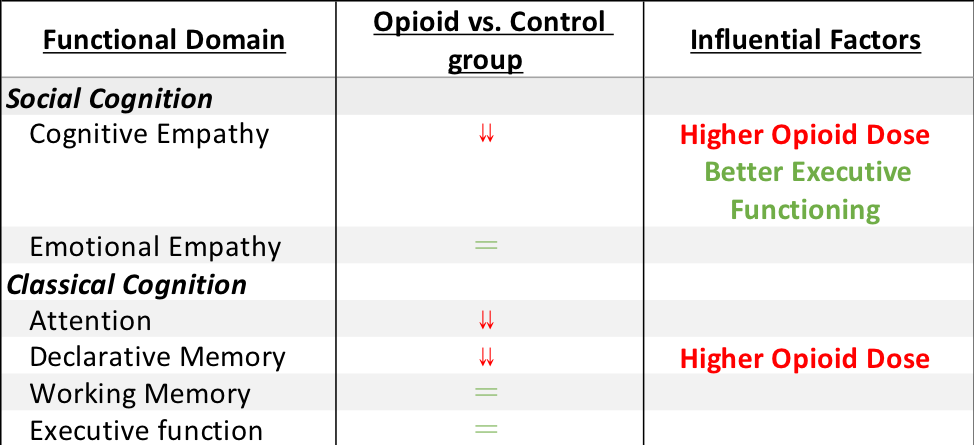
The table above shows the study outcomes, when controlling for demographic factors (e.g., age, education, IQ). The “⇊ “ symbolizes a deficit in the prescription opioid misuse group relative to the control group, and the “=” symbolizes no difference between groups. The right most column indicates the factors that influence performance in each domain among the opioid use group; Red text indicates that factor is associated with greater impairment in the given functional domain and green text indicates that factor is associated with better performance in a given functional domain.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This preliminary study demonstrates that regular prescription opioid misuse may have negative effects on cognitive function that extend to both classical (attention & declarative memory) and social (cognitive empathy)cognitive abilities. These cognitive functions are essential for everyday function and interpersonal relationships and interactions. Deficits in these domains have the potential to hinder social skills and treatment efforts, and may ultimately prolong opioid misuse, advance the disorder, and diminish the potential for recovery. Cognitive empathy (ability to recognize emotion) deficits, particularly for positive emotions, might lead to interpersonal conflict if, for example, happiness is mistaken for anger, or surprise is mistaken for fear. Interpersonal conflict is a key risk factor for relapse, suggesting this deficit’s potential for hindering treatment and recovery efforts. Additional deficits in attention and declarative memory have the potential to interfere with treatment efforts; individuals may be less able to attend to and remember incoming information important for addressing maladaptive substance use behaviors. Impairments in cognitive empathy appear to exist somewhat independent of one’s level of functioning in classical cognitive abilities, suggesting that rehabilitation efforts may need to target these functions separately. It is important to note that the individuals in this study were still engaged in opioid misuse and it is, therefore, unclear how long these deficits would last after abstinence is achieved. Still, these findings may have implications for the early stages of recovery, since opioid misuse often continues during the early stages of treatment, despite reductions in the amount or frequency of use over time. This study’s self–report measures also suggest that individuals with prescription opioid misuse may be unaware of their social cognition deficit. This lack of awareness can influence clinical intervention and treatment efforts, as individuals may not recognize the full scope of opioid-related consequences. Group interventions, and participation in community-based mutual-help organizations, may be helpful here so that individuals can help each other identify emotional states and experiences. Given that higher opioid doses appear to be associated with reduced ability in areas of classical and social cognitive functioning, misuse of opioids in greater quantities may have more serious short-term neuropsychological consequences. Although additional research is needed to replicate these findings, this is one of the first studies to investigate social cognition in individuals with prescription opioid misuse and it lends important insight to the cognitive empathy deficits that these individuals may be suffering from, without being aware of them. Studies like this are essential for gaining a better understanding of the effects of opioid misuse. Characterizing the cognitive consequences of prescription opioid misuse can ultimately help guide clinician-patient interactions and treatment plans that target areas of impairment to aid treatment and recovery efforts.
- LIMITATIONS
-
- As with all cross-sectional comparisons of affected vs. healthy groups, it is unclear whether opioid use directly caused these deficits or if these deficits predated and drove non-medical prescription opioid use. Furthermore, comorbid substance use disorders in the opioid use group may have the potential to negatively influence cognitive function. Given that this study aimed to look at the direct effects of prescription opioid misuse, the potential influence of other substance use cannot be ruled out.
- This study was conducted in Germany, and it is unclear whether these findings would translate cross-culturally. Differences between geographic regions with regard to cultural/social beliefs, emotional expression and opioid use patterns could lead to different outcomes. Additional research is needed to generalize findings cross-culturally.
- Although deficits in cognitive empathy were greater for positive emotions, the results approached statistical significance for anger and fear. The small sample size may mask a subtle but potentially broader range of impairment that spans positive and negative emotions. Therefore, further investigation with a larger sample is needed to replicate these findings.
BOTTOM LINE
- For individuals & families seeking recovery: Individuals with nonmedical prescription opioid use may have difficulty with memory and in reading certain types of emotions in other people, which they are unaware of. Difficulties paying attention and remembering important information can diminish treatment effects and impair daily functioning. A reduced ability to understand and read others’ emotions correctly can lead to difficulty in social situations and conflict in relationships at home and work. These classical and social cognitive impairments may be worse in individuals who are misusing prescription opioids in larger quantities. Understanding the effects of prescription opioid misuse on cognitive function can ultimately help guide clinicians in their treatment plans and may lead to strategies for enhancing treatment and recovery. Furthermore, recognizing these cognitive difficulties and their potential to cause interpersonal difficulties might reduce feelings of frustration and enhance patience in individuals and families seeking recovery, which can ultimately help loved ones better address their opioid use problems. Given the scope of the opioid problem and the number of individuals and families affected, more studies like this are necessary to enhance our understanding of the more subtle and potentially long-term effects of opioid misuse so that we can better help those affected.
- For scientists: Prescription opioid misuse may be accompanied by deficits in cognitive empathy, as well as attention and declarative memory. Individuals may be unaware of cognitive empathy deficits and impairment may be more pronounced in those who use higher opioid doses. The deficits observed in classical cognitive functions here are less widespread than those observed in previous opioid-focused studies, warranting further investigation as to whether inconsistent outcomes are attributable to variability in sample comorbidity (e.g., co-occurring psychiatric conditions), disorder severity, or the specific opioid under investigation (heroin vs. prescription opioid). Nonetheless, cognitive empathy impairments appear to be somewhat independent of functional ability in classical cognitive domains, with executive function playing a role in cognitive empathy but not fully accounting for cognitive empathy impairments. Given the preliminary nature of this study, additional research is needed to replicate these findings, determine their cross-cultural applicability and whether residual effects would be observed after cessation of opioid misuse. Characterizing the cognitive consequences of prescription opioid misuse can ultimately help develop scientific models for informing treatment and recovery in this population.
- For policy makers: Research studies like this one provide important information about the consequences of one of our nation’s biggest public health problems on the individuals directly suffering from it. In the context of this study, cognitive abilities that play an important role in social skills and daily functioning appear to be impaired in individuals currently engaged in prescription opioid misuse. Understanding the negative short-term consequences of prescription opioid misuse is important because it can help us to inform clinical treatment and benefit patients suffering from opioid problems. Given that this is the first study to look at social cognition in individuals with prescription opioid misuse and that it took place in Germany, additional funding is needed to conduct these kinds of studies in the U.S., which will help determine whether findings translate cross-culturally and improve our ability to more effectively address our country’s opioid epidemic.
- For treatment professionals and treatment systems: Individuals currently engaged in prescription opioid misuse may exhibit deficits in classical (attention & declarative memory) and social (cognitive empathy) cognitive abilities, which they are unaware of. Those who use opioids in larger doses may be at risk for even larger deficits in cognitive empathy skills. Understanding and recognizing emotion in others is essential for healthy interpersonal functioning and important to the clinician-patient relationship. Furthermore, classical cognitive abilities play an important role in daily functioning and difficulties with attention and memory can hinder an individual’s ability to fully process and benefit from clinician interactions and treatment efforts. Recognizing these deficits can ultimately help guide clinician-patient interactions and treatment plans to aid recovery efforts. Given that social cognition impairments can ultimately lead to interpersonal difficulties and that interpersonal conflict is a key risk factor for relapse, addressing these deficits might aid recovery efforts. Group interventions and participation in mutual-help organizations have the potential to help individuals overcome these difficulties, as participants can help each other identify emotional states and experiences. Additional investigation is needed to replicate these findings, to identify best practices for addressing social cognition deficits, and to determine if these deficits continue during abstinence and whether opioid misuse severity, psychiatric or medical comorbidities play a role in cognitive empathy difficulties.
CITATIONS
Kroll, S. L., Nikolic, E., Bieri, F., Soyka, M., Baumgartner, M. R., & Quednow, B. B. (2018). Cognitive and socio-cognitive functioning of chronic non-medical prescription opioid users. Psychopharmacology, 235(12), 3451-3464.

