Buprenorphine and methadone treatment among Medicaid members: Reducing relapse and health care costs
Despite evidence supporting the effectiveness of medications for opioid use disorder, state funded insurance programs often lack adequate coverage of this treatment option.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
For example, state Medicaid programs may impose control measures for receiving a prescription (e.g., quantity limits and lifetime treatment limits) which can make it difficult for patients to obtain these medications.
Since Medicaid programs fund over 1/3 of all substance use disorder (SUD) treatment in the U.S.,, it is important to determine the potential benefit of medications for opioid use among Medicaid beneficiaries.
HOW WAS THIS STUDY CONDUCTED?
With less restrictive access to these medications relative to other programs, MassHealth offers an opportunity to determine how access to, and use of, these medications may improve treatment outcomes for Medicaid beneficiaries in the long term.
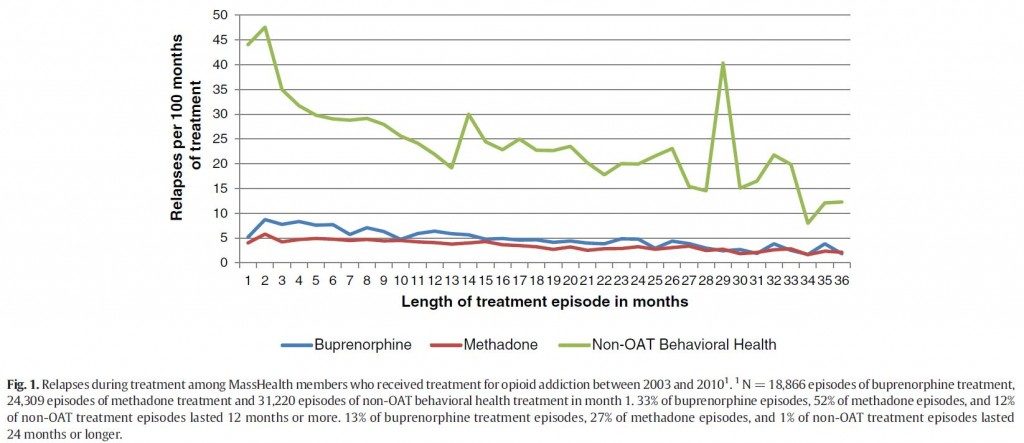
This study by Clark and colleagues used MassHealth data of members age 16 and older with a primary diagnosis of opioid abuse or dependence between 2004 and 2010 to examine the association between type of treatment episode (whether it was buprenorphine/naloxone, methadone, or behavioral health treatment) and relapse rates and total healthcare costs during treatment episodes. Relapse was considered to have occurred if a patient had claims data for detoxification, inpatient admission with a primary diagnosis of substance use disorder (SUD), or an emergency department visit with a primary diagnosis of SUD at some point after the index episode of care.
WHAT DID THIS STUDY FIND?
Between 2004 and 2010, 56,278 individuals received a total of 104,840 episodes of treatment. Members who did not receive medication assisted treatment (MAT) were more likely to have co-occurring mental illness and alcohol use disorders, higher average costs, and more frequent relapses. Episodes of buprenorphine or methadone maintenance treatment were less than half as likely to result in relapse compared to behavioral health treatment (i.e., non-MAT. Individuals with co-occurring alcohol abuse or dependence experienced relapse at four times the rate of those without alcohol abuse or dependence.
Each year of current treatment was associated with a decreased relapse rate of about 30%.
Having an addiction to drugs in addition to opioids doubled the risk of relapse. After controlling for factors including treatment history and length of treatment episode, methadone and buprenorphine treatment episodes were associated with lower total health care expenditures compared to behavioral health treatment; this ranged from savings of $153 to $223 per month.
The average per person cost of treatment was $786 higher per month when factoring in co-occurring severe mental illness, alcohol use disorders, and other drug use disorders.
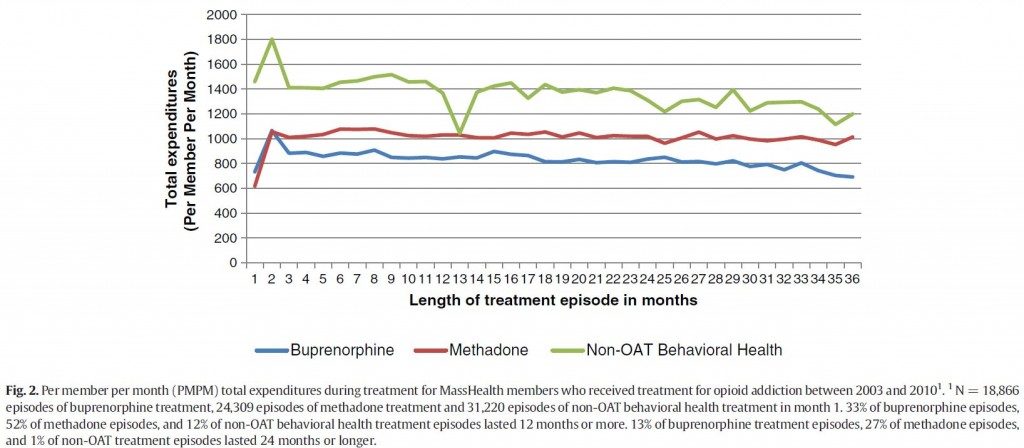
This study adds support for medication assisted treatment's (MATs) ability to reduce relapse—and at a lower cost—than behavioral health treatment alone. Additionally, the data suggests that longer treatment may result in an increasingly lower rate of relapse over time.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study provides evidence about the use of medications among Medicaid beneficiaries.
If the data from Massachusetts’ Medicaid program, known as MassHealth, support its use, other state Medicaid programs may choose to reimburse for this treatment modality consistent with the evidence base (e.g., like other chronic health conditions, such as diabetes) and potentially to improve access to care with fewer barriers to accessing it.
Comorbidity or co-occurring conditions increased risk of relapse and total healthcare expenditures. Medication assisted treatment (MAT) alone may not be suitable for patients with more severe mental health problems.
- LIMITATIONS
-
- Since this study relied on data available through Medicaid claims, it is possible that the number of relapses was underestimated since not all relapses may be captured by insurance claims (i.e., a person may relapse without requiring detoxification, admission to a hospital, or an emergency room visit).
- Additionally, if non-MAT behavioral health treatment episodes overlapped with a methadone or buprenorphine treatment episode, it was classified as medication assisted treatment (MAT) treatment. It is unclear how many of the MAT treatment episodes may have included some combination of MAT and behavioral treatment. While the data used was observational and results cannot be interpreted as causal, this study was able to assess MAT in a real-world setting.
NEXT STEPS
Next steps should address how to increase access to these medications in other state Medicaid programs. A qualitative study of policy makers in Ohio identified some barriers to implementing buprenoprhine/naloxone treatment (e.g., limited availability of prescribers), but more quantitative research including cost-effectiveness analyses are needed to bolster support for medications for the treatment of opioid use disorder.
BOTTOM LINE
- For individuals and families seeking recovery: Opioid agonist therapy may help reduce your risk of relapse if you suffer from opioid use disorder. Consult with an addiction specialist for more information on medications for opioid use disorder.
- For scientists: It is established that medications such as buprenoprhine and methadone are effective for the treatment of opioid use disorder. The next steps include research examining for whom these medications work best, and determining how to implement programs to provide widespread access to the people who need these medications.
- For policy makers: With Medicaid programs expanding under the Affordable Care Act, it is important that members have access to effective and less costly addiction treatment options.
- For treatment professionals and treatment systems: Not all medications are effective for all individuals so it is important that patients are aware of their options. Work with your patients to determine the best treatment plan for them.
CITATIONS
Clark, R. E., Baxter, J. D., Aweh, G., O’Connell, E., Fisher, W. H., & Barton, B. A. (2015). Risk Factors for Relapse and Higher Costs Among Medicaid Members with Opioid Dependence or Abuse: Opioid Agonists, Comorbidities, and Treatment History. J Subst Abuse Treat, 57, 75-80. doi:10.1016/j.jsat.2015.05.001

