Critical need at critical times: Transitions to and from methadone treatment are associated with higher risk of drug related death
Methadone treatment is a safe and evidence-based approach to treating and managing opioid use disorder, yet interruptions to care can be life-threatening. In this study based in Ireland, authors take a critical look at patterns of treatment disruption and the impact of these disruptions on risk for drug-related death and all-cause mortality using large-scale administrative databases.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
The alarming prevalence of opioid use, disorder, and overdose death has become an international public health concern. Efforts to curb this epidemic include prescription of medications for addiction treatment, like methadone, which has been shown to be safe and effective. However, risk of mortality and drug-related overdose death remains. In this study, authors combine data from multiple sources to examine trends and identify critical periods of elevated risk for mortality and drug-related death among methadone patients. By identifying these critical periods, treatment providers and policy makers can be better equipped to intervene and thereby reduce harms among methadone patients.
HOW WAS THIS STUDY CONDUCTED?
The aim of this study was to examine risk of overdose and death among patients taking methadone for opioid use disorder, following interruptions to care (e.g., transferring service providers). The authors conducted an observational study of 2,899 patients in Ireland (whose methadone treatment practices resemble those of the U.S.), between January 2010 and December 2015, who were registered on the Central Treatment List and prescribed and dispensed methadone at least once. The Central Treatment List is a large database of patients prescribed medications for opioid use disorder including methadone medication. This database includes information about patients’ treatment history, including types of treatment (including entry into prison), and dates of receipt, discharge, and (re)initiation. Pharmacy data, which includes information about dates of prescriptions, prescriber name(s), and clinic and dispensary locations, was also combined with Central Treatment List data. Additional administrative information included data from the Health Service Executive’s (HSE) Methadone Treatment Scheme (e.g., primary care treatment and prescriptions information), and the General Medical Services, which provided detailed information about all prescription medications dispensed in primary care during the observation period. Finally, these data were then combined with mortality data contained within the National Drug Related Death Index, General Mortality Register through the Central Statistics Office, HSE Hospital In-Patient Enquiry, and Central Treatment List databases.
The researchers then used these data to examine patients’ treatment status (engaging in addiction service, primary care, in prison [where they still received methadone treatment, which has been shown to be effective], or “out of treatment”) across each day of the study. They defined treatment duration as periods of uninterrupted care (i.e., daily methadone supply), with breaks not exceeding seven days. Methadone patients with treatment breaks or interruptions beyond seven days were considered to have discontinued treatment. The “out of treatment” designation began after the seventh day and continued until the patient re-engaged in treatment. Given these definitions, the authors came up with the following treatment/discontinuity designations to examine risk for mortality:
- The first four weeks following a transfer between clinics (e.g., prison to primary care).
- Continuous treatment with the same prescriber for five weeks or more.
- Continuous “out-of-treatment” status for five weeks or more.
- The first four weeks following cessation of treatment.
- The first four weeks following initiation or re-initiation into treatment following a period of being out of treatment.
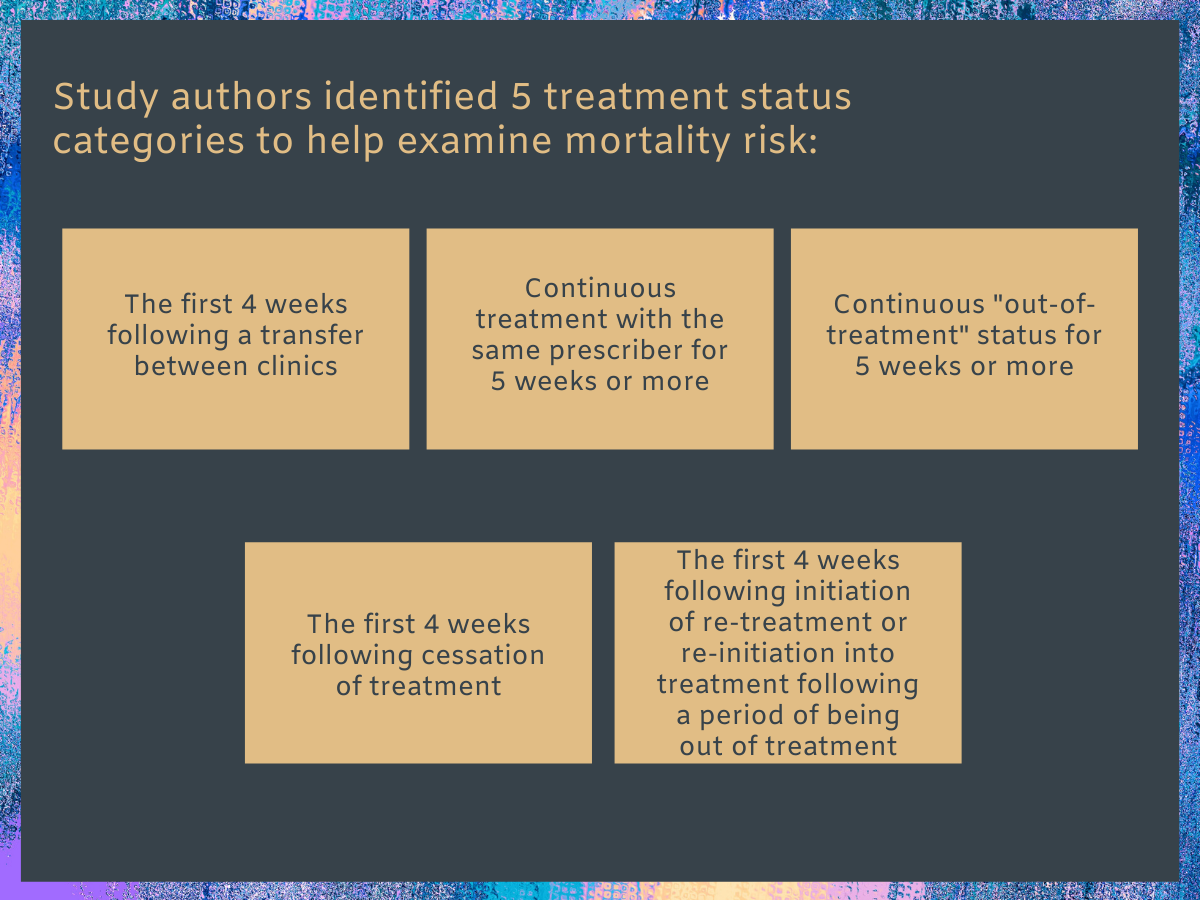
Figure 1.
Using these designations, the researchers examined whether these patterns were associated with risk of mortality (all causes) and drug-related deaths, after statistically adjusting for other patient characteristics (i.e., age, gender, history of incarceration, median methadone dose, and presence of co-occurring disorders).
All of the patients in this study were residents of Ireland. Among the 2,899 patients included, 85% entered during the first year of observation (2010). Patients were observed for a median of 5.5 years. The median age of patients was 34 (actual range not available) and about two-thirds were men (68%). The majority (66%) also had multiple co-occurring conditions, such as psychiatric disorders (66%); diseases related to digestion (34%), respiration (24%), and/or circulatory (18%) or nervous systems (13%), to name a few.
WHAT DID THIS STUDY FIND?
Death rates:
Using data from multiple sources (e.g., public data bases, hospital databases, prescription medication, and mortality registries), the researchers found that 154 (5.3%) died during the 2010-2015 observation period; 36.2% (55) of these deaths were drug related.
Critical periods:
Compared to patients in continuous methadone treatment, drug-related death rates were highest among patients during the first four weeks after initiating, re-initiating, or discontinuing treatment. These periods of time were also linked to overall mortality risk; however, remaining out of treatment (between four and 52 weeks) was also associated with higher general mortality rates.
Patients who transferred care to another provider or setting (e.g., primary care to specialty addiction clinic, prison to primary care) during methadone treatment were no likely to die than patients who remained in continuous treatment.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study utilized data from numerous sources to document patterns of treatment receipt and discontinuity associated with drug-related and general mortality among methadone patients in Ireland. Among 2,899 patients monitored between 2010 and 2015, 5.3% died and 1.9% died for drug-related reasons (e.g., overdose). Importantly, researchers found that the first 4 weeks following methadone treatment (re)initiation and cessation were associated with the highest risk of drug-related death and all-cause mortality. Remaining out of treatment (four weeks to one year) was also associated with higher risk of all-cause mortality.
The finding that patients were more likely to die in the 4 weeks following methadone initiation may be accounted for by the continued opioid use in addition to prescribed methadone (i.e., accumulation of opioids in the system that exceeds the patients’ tolerance).
Concurrent use of other substances, like alcohol or benzodiazepines, might also explain elevated mortality risk following treatment (re)initiation. On the other hand, elevated mortality risk following treatment discontinuation may be explained by patients’ return to opioid or other drug use, and/or psychosocial or psychiatric stressors that might also be more difficult to manage during these transitions.
Methadone discontinuation, particularly among those receiving it from primary care physicians, might also be related to disengagement with medical care generally. As such, providing continuing care in the form of counseling might help reduce risk, facilitate healthcare transitions, and/or reduce risk of disengagement with opioid use disorder treatment. This might extend beyond methadone treatment, as negative outcomes have also been documented following disruption to buprenorphine treatment.
Unlike previous research, patients who transferred to another clinic or provider during active methadone treatment were no more likely to die than patients who remained in continuous, uninterrupted treatment. However, it is important to note that 67% of these transfers were from primary care clinics to prison, which may offset mortality risk.
- LIMITATIONS
-
- The researchers were unable to account for key variables related to mortality risk, such as rates of relapse vs. abstinence following discontinuation of methadone treatment; use of other substances; routes of administration for any drug use (e.g., oral vs. intravenous); demographic characteristics; other relevant health factors (e.g., Hepatitis C or HIV status); or other types of treatment received, its quality, or intensity.
- The researchers were unable to account for hospital admissions where methadone may have been unavailable, which would have appeared as methadone treatment discontinuation in their study.
- The researchers excluded patients who were taking other medications for opioid use disorder, such as buprenorphine (e.g., Suboxone, Subutex), limiting generalizability to individuals with opioid use disorder more broadly.
- Reliance on administrative data but also aggregation of administrative data from multiple sources may introduce bias to the extent that researchers cannot account for differences in data collection or reporting practices across data sources.
- The data used in the current study is not exhaustive. Ongoing research and replication are needed to increase generalizability. Incorporating data from additional sources would help.
BOTTOM LINE
- For individuals and families seeking recovery: The results of this study suggest that the first four weeks following methadone treatment initiation, re-initiation, and discontinuation are associated with greater risk drug-related and all-cause mortality among methadone patients. Remaining out of treatment is also associated with increases in all-cause mortality. This is important for individuals and families to consider so they can monitor potential risks, such as continued use of substances following treatment initiation, or relapse following methadone discontinuation. At the same time, 5.3% and 1.9% of patients died for any vs. drug-related reasons between 2010 and 2015, respectively, and not all during treatment initiation or discontinuation. Further, these mortality rates are considerably lower than the mortality rates associated with continued use of opioids. Methadone has been shown repeatedly to be a safe and effective treatment and remains a front-line medication for opioid use disorder. Other drugs, like buprenorphine (e.g., Suboxone, Subutex), are also evidence-based and may be associated with lower mortality rates. For family members of deceased drug users, individual and group-based grief counseling may help.
- For treatment professionals and treatment systems: This study suggests that methadone patients are at greater risk of dying during the first four weeks following initiation or discontinuation of methadone treatment. As providers, assessing and monitoring risks following initiation of methadone treatment, and helping patients pre-emptively to manage such risks whenever possible, may help reduce their risk for harm. Risks to consider during treatment initiation include methadone diversion, concurrent use of other respiratory suppressants (e.g., opioids, alcohol, benzodiazepines), and underlying medical and psychiatric conditions that might elevate mortality risk. Preparation for discontinuation of methadone should include education and relapse prevention, contingency planning (e.g., identifying signs it might be good idea to resume methadone treatment), and facilitation of healthcare transitions to ensure patients are connected with necessary medical and mental health services following discontinuation of methadone treatment.
- For scientists: Mortality risk was shown to be highest among methadone patients treated in Ireland during the first 4 weeks following treatment initiation and discontinuation. Though notable, these findings require follow up research to take into account mechanisms and moderators of risk. Unmeasured variables in the current study, such as continued or return to substance use, specific underlying mental health and medical conditions, and other high-risk behaviors (e.g., suicide) may help explain this elevated risk in follow up research. Previous research found that patients were also at risk of death following transfer to other clinics or providers; however, the authors of this study did not and attributed this largely to the fact that most transferred from primary care to prison. Replication is needed to test this hypothesis. In addition, incorporating data from patients, their medical charts, and prescribers could improve efforts to model mortality outcomes among methadone patients. In addition to assessing unmeasured confounds in the current study, intensive longitudinal data collection methods, including daily diary and ecological momentary assessment, could produce meaningful insights into the precise mechanisms of risk during the critical 4-week periods post treatment initiation and discontinuation.
- For policy makers: Death rates in the current study were highest among methadone patients in the 4 weeks following treatment initiation and discontinuation. Policy makers can assist with overcoming this service gap by helping to ensure sufficient allocation of resources to support patients and facilitate these critical healthcare transitions. This might come in the form of funding allocation to (1) research these critical periods more thoroughly so researchers and providers can understand better why drop-out is occurring and develop effective prevention and intervention strategies, or (2) support facilities and clinics to address this unmet need (e.g., staff trainings, higher provider to patient ratio, creation of step-down or after care services).
CITATIONS
Durand, L., O’Driscoll, D., Boland, F., Keenan, E., Ryan, B., Barry, J., Bennett, K., Fahey, T., & Cousins, G. (2020). Do interruptions to the continuity of methadone maintenance treatment in specialist addiction settings increase the risk of drug‐related poisoning deaths? A retrospective‐cohort study. Addiction, [Epub ahead of print]. doi:10.1111/add.15004.

