Medicaid Coverage of Medications to Treat Addiction
Substance use disorders are common among people who receive healthcare through Medicaid, yet less than 5% of Medicaid recipients receive treatment each year.
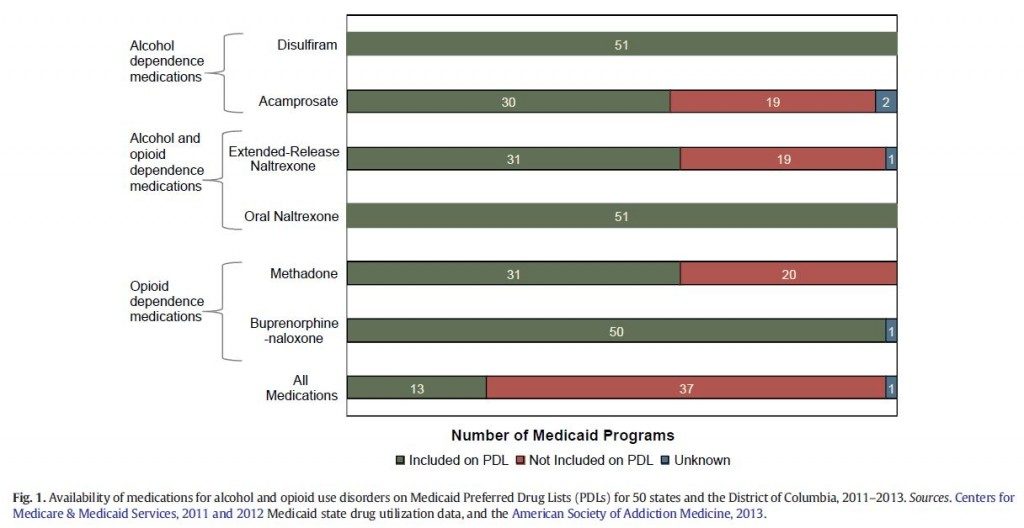
Medication-assisted treatment is an important option for these individuals. However, prescription of these medications depends on Medicaid prescription drug programs which vary by state.
With three medications approved by the Federal Drug Administration available for the treatment of opioid use disorder:
- naltrexone
- buprenorphine
- methadone
& three for the treatment of alcohol use disorder:
- disulfiram
- naltrexone
- acamprosate
it is important that individuals have access to multiple options since it is unlikely that one medication will be effective for all patients.
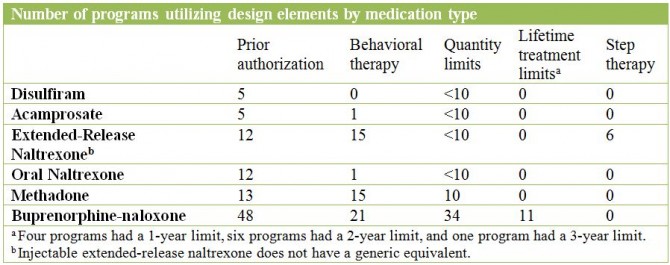
Mark and colleagues used Medicaid pharmacy documents and state drug utilization data to characterize the coverage of these medications within individual state Medicaid programs (including the District of Columbia, N = 51). The authors also examined the Medicaid benefit design elements (described below) for each medication.
The Medicaid benefit design elements for each medication:
- Prior authorization: requires a prescriber to receive permission from the benefit plan prior to prescribing a medication to a member
- Behavioral therapy: requires evidence that a patient has a referral to or has attended some form of behavioral therapy before a prescription can be filled
- Quantity limits: the maximum quantity of medications that can be reimbursed under the benefit plan per one prescription or copayment (e.g., 30 days in-person or 90 days for mail order)
- Lifetime treatment limits: a dollar limit on the amount the program will spend on the treatment during the entire time a patient is enrolled in the plan
- Step therapy: patients are required to try a first-line treatment (e.g., generic or alternative medication) before receiving a second-line treatment (e.g., brand medication)
Source: (Mark et al., 2015)
IN CONTEXT
This study showed that coverage of medications for the treatment of alcohol and opioid use disorders vary by state and are subject to multiple potential control elements.
Pharmaceutical benefits are designed in an effort to cover the best interest of different constituencies; they should be cost-saving, deter inappropriate use, and guarantee accessibility of treatments for those who need them.
It is important to reevaluate prescription drug benefits while keeping the conditions for which the medications are indicated in mind.
- For example, since opioid and alcohol use disorders are diseases which can result in disability, contraction of further disease, and premature mortality, any delay imposed by these design elements could act as a barrier to care with serious and even deadly ramifications. Innovative solutions are needed at the state level to prioritize patient care.
- For example, after experiencing long waitlists for outpatient buprenorphine-naloxone treatment, Massachusetts created a nurse management program where nurses conduct assessments, referrals, and adherence monitoring to alleviate the workload of the prescribing physicians and allow them to see more patients (see here)
Ultimately, coverage of a medication by a Medicaid program is not beneficial if the patients are unable to access the necessary care. While coverage may involve expenditure upfront, it is likely to save money in health care costs in the long run.
BOTTOM LINE
- For individuals & families seeking recovery: If you are a Medicaid patient, medication options for the treatment of alcohol or opioid use disorder may be limited by your state program’s preferred drug list. Work with a clinician to determine the best option for your needs. Also, some programs have financial and resource specialists that can support your ability to advocate and appeal to your insurance companies for medication coverage.
- For scientists: More research needs to be done to investigate the incremental clinical utility of medications that are most commonly not covered by Medicaid (i.e., injectable extended-release naltrexone vs. daily oral naltrexone).
- For policy makers: Since not all medications work for every patient, it is important that Medicaid recipients have multiple medical options for the treatment of alcohol or opioid use disorders. Policies that reduce barriers to evidence-based medication-assisted treatments can radically improve health and quality of life.
- For treatment professionals and treatment systems: If your patient cannot receive a medication that you think is appropriate due to lack of coverage by Medicaid, see if the patient may respond to a medication that is covered. To the extent that it is financially feasible, consider hiring a patient coordinator or advocate to help them effectively work with their insurance to access care. Patients may also respond to behavioral therapies.
CITATIONS
Mark, T. L., Lubran, R., McCance-Katz, E. F., Chalk, M., & Richardson, J. (2015). Medicaid coverage of medications to treat alcohol and opioid dependence. J Subst Abuse Treat. doi: 10.1016/j.jsat.2015.04.009

