Linking Hospital Patients to Medication for Opioid Use Disorder: Not One Size Fits All
Buprenorphine (often prescribed in a formulation with naloxone, known by brand name Suboxone) is a helpful medication for many people with opioid use disorder. Yet, relatively few opioid-addicted individuals seek it out.
Linking people to services that can prescribe and monitor use of this medication if they happen to end up in the hospital for an opioid-related, or other, reason, might provide an innovative pathway to access and begin treatment. Does this kind of active linkage work, and do the challenges of injection use make a difference in terms of outcomes?
WHAT PROBLEM DOES THIS STUDY ADDRESS?
The sharp increase in opioid use disorder and opioid overdoses has been well documented, and much is being done to address this public health epidemic. Medications like buprenorphine – often prescribed in combination with naloxone as “Suboxone” – are among the most helpful treatments for opioid use disorder, in terms of decreasing illicit opioid use, and reducing the likelihood of overdose and death. Because only 10% of individuals requiring specialized substance use disorder treatment actually seek it, innovative ways to engage and target these individuals are being developed and evaluated.
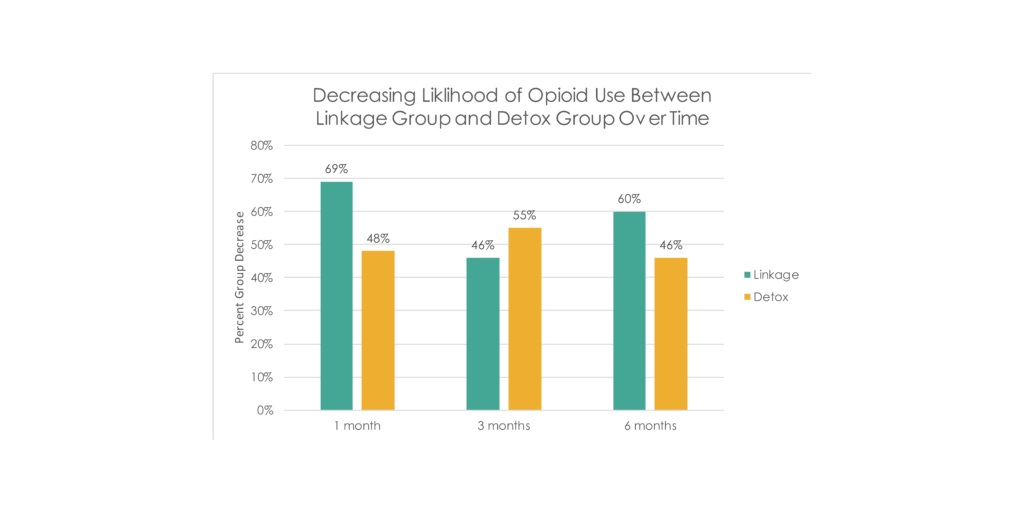
In one study called the “Suboxone Transition to Opiate Program” or “STOP”, hospitalized individuals that also had a possible opioid use problem, were given an intervention to systematically start them on buprenorphine then link them to outpatient buprenorphine treatment. When this was compared to providing medical opioid detoxification if needed and a treatment referral (“detox”), 72% of the buprenorphine linkage patients versus 12% of the detox patients showed up to subsequent buprenorphine treatment, and they had a 40% lower likelihood of illicit opioid use up to 6 months after the hospitalization.
Because injection opioid users are often more severe and present unique health care challenges compared to non-injection users, Cushman and colleagues re-analyzed these STOP data but this time investigating only the subsample of study participants who were injection opioid users.
HOW WAS THIS STUDY CONDUCTED?
Authors compared 51 individuals in the linkage group to 62 in the detox group, all of whom were injection heroin users. For the linkage, patients were started on buprenorphine (called “induction”) while in the hospital, then were scheduled an appointment at an outpatient primary care clinic affiliated with the hospital and given enough medication to last them until that appointment. The clinic used a “collaborative care model” which provided monitoring in addition to buprenorphine prescription, as well as nurse care managers who were responsible for the bulk of patient care.
Patients, on average, were 40 years old; 69% were male and the ethnic/racial composition was diverse with 49% White, 23% Black, 20% Latino, and 8% of another racial/ethnic background. The groups were similar on many measured characteristics when they started treatment in the hospital, including how often they used opioids, though the detox patients were more likely to have used cannabis and cocaine in the 30 days before treatment (28 vs. 45% and 53 vs. 69%, respectively), though these differences were not statistically significant.
WHAT DID THIS STUDY FIND?
Interestingly, this effect of greater engagement with buprenorphine but similar opioid use was evident early in the trial.
By 1 month, linkage patients took buprenorphine, on average 22 days out of 30 (standard deviation = 10) versus 7 out of 30 in the detox group (standard deviation = 8).
Their opioid use, however, was similar during this time period, with 12 days of illicit opioid use in the linkage group (standard deviation = 8) versus 13 in the detox group (standard deviation = 8).
WHY IS THIS STUDY IMPORTANT?
Finding innovative ways to engage people with opioid use disorder in evidence-based treatments like buprenorphine is critical.
The initial STOP study based in hospital settings, and another study reviewed in a prior Bulletin which was based in emergency rooms both demonstrated innovative ways to engage individuals with opioid problems with helpful buprenorphine medication treatment.
In this latest analysis of the STOP study, in contrast with the positive linkage findings in the whole sample of individuals with opioid use disorder, injection users did not benefit from the active linkage to buprenorphine compared with detox and referral. As such, this study highlights the importance of examining subgroups of patients for whom the typical current standard of care may not be adequate
While the buprenorphine linkage patients were more likely to be in buprenorphine treatment 6 months later, only 14% were in treatment, which is also a low percentage, albeit better than the 3% of the detox group.
Suggestion in terms of what might be needed for this group of injection users, given that they were more likely to engage with buprenorphine treatment, but had similar outcomes:
- Increasing their dose or perhaps adding psychosocial treatment (though other studies have shown adding psychosocial treatment to buprenorphine is no more helpful than buprenorphine alone)
- The benefits of recovery-specific social support as an addition to medication. In another prior RRI Bulletin, for example, we highlighted a study from Baltimore, Maryland, showing 12-step mutual-help participation (e.g., Narcotics Anonymous involvement) and buprenorphine treatment produced additive beneficial effects when used together.
- LIMITATIONS
-
- The sample was small (51 in the linkage group and 61 in the detox group). It is possible that a study targeting just individuals with injection opioid use would have produced different results, rather than this analysis that analyzed a subgroup in existing data. That said, the detox patients were actually slightly more severe when entering treatment in terms of additional other drug use, and they may have had greater challenges that were not accounted for in the results. This, however, would actually favor the buprenorphine linkage group. Given that they did not perform any differently, that makes it less likely a larger sample would have made a difference.
- Finally, the results were based entirely on self-reported use, with no validation of these reports by urine toxicology screens as is often done in studies testing interventions for opioid use.
NEXT STEPS
More research is needed specifically on how to improve outcomes of hospitalized individuals with injection opioid use. It is possible that different combinations and intensities of medical, psychological, and community-based approaches might be needed.
BOTTOM LINE
- For individuals & families seeking recovery: Injection opioid users in the hospital may not find efforts to start and actively link them with buprenorphine treatment any more helpful than receiving detox and referral to treatment. More research is needed to determine the best ways to help injection opioid users who are resistant or otherwise have difficulty seeking treatment on their own.
- For Scientists: This secondary analysis of an active linkage to medication-assisted treatment with buprenorphine (in combination with naloxone, as Suboxone) for injection users in the hospital yielded null findings. The sample was small and the study may not have been adequately powered to detect benefits over time. Research that specifically targets this group of patients in a study that is adequately powered to detect benefit could offer different results, however.
- For Policy makers: Injection opioid users in the hospital may not find efforts to start and actively link them with buprenorphine any more helpful than receiving detox and referral to treatment. More research is needed to determine the best ways to help injection opioid users who are resistant to, or otherwise have difficulty seeking treatment on their own.
- For Treatment professionals and treatment systems: Injection opioid users in the hospital may not find efforts to start and actively link them with buprenorphine treatment any more helpful than receiving detox and referral to treatment. More research is needed to determine the best ways to help injection opioid users who are resistant to, or otherwise have difficulty seeking treatment on their own.
CITATIONS
Cushman, P. A., Liebschutz, J. M., Anderson, B. J., Moreau, M., & Stein, M. D. (2016). Buprenorphine Initiation and Linkage to Outpatient Buprenorphine Do Not Reduce Frequency of Injection Opiate Use Following Hospitalization. Journal of Substance Abuse Treatment.

