The Therapeutic Paradox of Crisis: Reducing barriers to medications for opioid use disorder by starting patients on buprenorphine during emergency department visits
Buprenorphine, often prescribed in combination with naloxone known under the brand name Suboxone, is an empirically-supported medicine that reduces opioid use and risk for overdose in people with opioid use disorder (OUD). At the same time, getting this medication to the people who need it is an ongoing challenge, with many barriers existing in the United States that limit its use. This study assessed a novel intervention that aims to improve the accessibility of this life saving medication by enabling emergency department physicians, with the help of peer recovery coaches, to start patients on buprenorphine when they come to the emergency room for acute medical care.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Hospital emergency departments see hundreds of thousands of patients with OUD per year. Until recently, the standard of care for treating patients with OUD in the emergency department has been with a referral to outpatient addiction treatment. For various reasons, the vast majority of patients don’t follow up on these referrals and get connected with care. In 2015, however, an important study demonstrated that starting patients on buprenorphine when they present to emergency departments for acute medical care was associated with significant improvements in OUD outcomes, including decreased opioid use and heightened treatment engagement rates. Despite evidence demonstrating benefits of emergency department-buprenorphine initiation for OUD, many barriers still exist in implementing such programs, including issues around funding, staffing, training, treatment philosophy, culture change, limited referral sites for continued care of patients, and the federal regulations surrounding buprenorphine prescribing. The authors of this paper examined how feasible it is to implement this emergency-room intervention. In doing so, they provided an overview of a pilot implementation program, aimed at,1) identifying patients with OUD in the emergency department, 2) initiating buprenorphine for these patients, and 3) ensuring appropriate and timely follow-up care takes place with the help of peer recovery coaches.
HOW WAS THIS STUDY CONDUCTED?
This was an implementation and observational study that assessed 241 patients receiving buprenorphine through a novel program aimed at starting patients on buprenorphine when presenting to the emergency room for acute medical care at the Medical University of South Carolina from December 2017–March 2019, and Tidelands Waccamaw Community Hospital and Grand Strand Medical Center from March 2018–March 2019. Outcomes assessed at 30 days after the emergency department visit included rate of participant follow-up appointments attended, rate of continuation of buprenorphine medication, and lessons learned implementing this intervention.
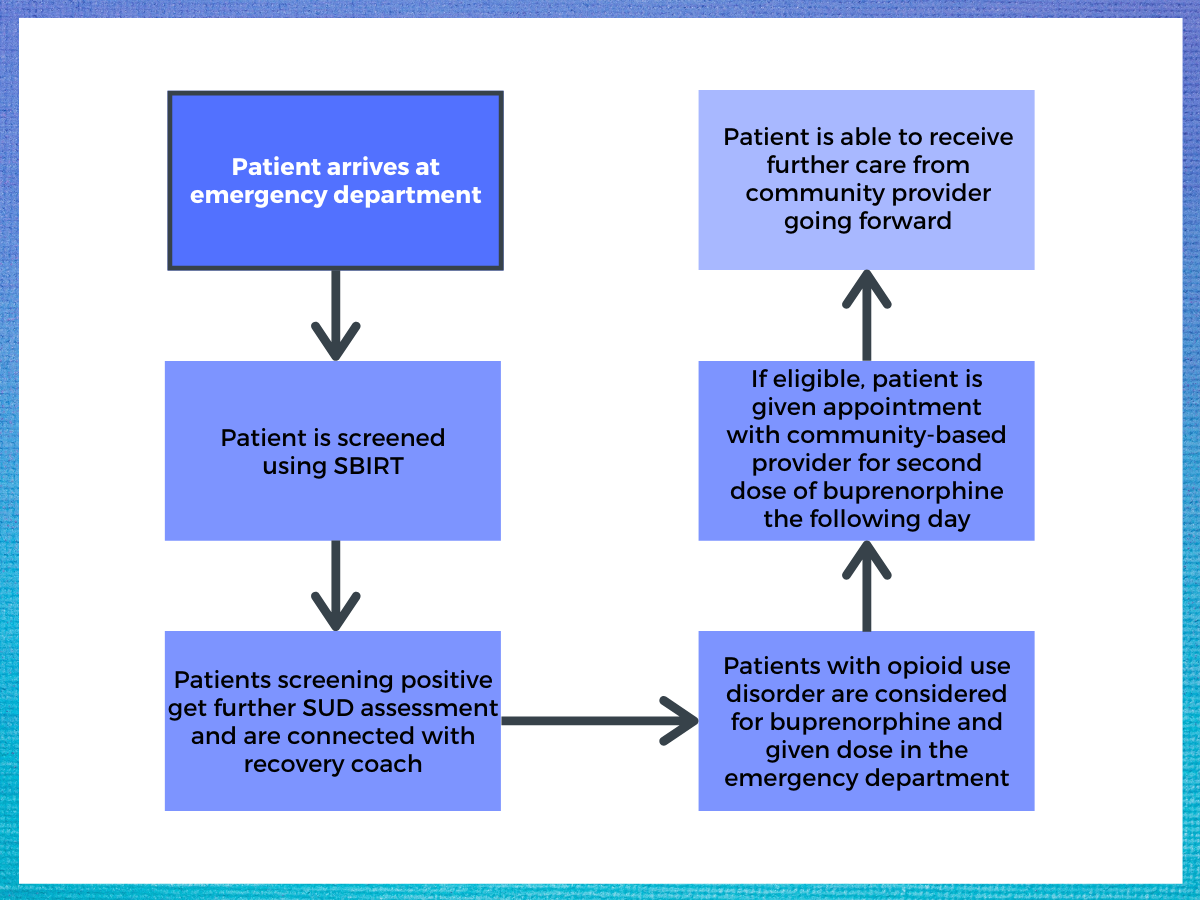
Figure 1. Flowchart detailing the intervention process.
At all three sites, peer recovery coaches (referred to in this study as patient navigators) worked directly with patients and clinical staff to complete Screening, Brief Intervention And Referral To Treatment (SBIRT) for each patient coming through the emergency department. This is a brief screener developed by the Substance Abuse and Mental Health Services Administration (SAMHSA) designed to identify patients with problematic substance use in medical settings. Additionally, universal screening for substance use disorders (SUD), including alcohol, opioids, and other illicit drugs, was added into the workflow for all patients presenting to the emergency department. Preferred screening tools included the two National Institute of Drug Abuse quick screen questions related to prescription and non-prescription drug use, and the Alcohol Use Disorders Identification Test – Concise (AUDIT-C). Peer recovery coaches were given access to electronic health records to help them identify candidates for buprenorphine initiation. Additionally, emergency department clinical staff were encouraged to alert peer recovery coaches if they felt a patient was appropriate for buprenorphine.
Individuals identified as having OUD were further screened to assess eligibility for buprenorphine initiation during their emergency department visit. If a patient was identified as an interested candidate for buprenorphine, the peer recovery coach discussed the patient’s candidacy with the emergency department provider and nurse. Exclusion criteria for receiving buprenorphine included admission to the hospital, residence outside of the local ‘tri-county’ area, and/or a Clinical Opiate Withdrawal Scale score <8, suggesting the patient was not experience opioid withdrawal symptoms. Patients with a Clinical Opiate Withdrawal Scale score >8 were further assessed for OUD by clinical staff. If OUD was confirmed, the patient was given a single dose of 8mg of sublingual buprenorphine. Peer recovery coaches arranged for follow up within 24 hours for an additional buprenorphine dose. Additionally, any patient identified with OUD, regardless of buprenorphine eligibility/dosing, was offered an intranasal naloxone kit and education prior to discharge (naloxone is a medication that helps to reverse opioid overdose). Hospital pharmacies were involved throughout the process to minimize any delays in getting buprenorphine when ordered from the emergency department and naloxone kits could be distributed directly to emergency department patients prior to discharge.
The protocol for connecting patients to ongoing buprenorphine prescriptions subsequent to emergency department medication initiation was not described, though in this study’s 2015 predecessor, D’Onofrio and colleagues provided patients with sufficient take-home daily doses to ensure they had adequate medication to last until a scheduled appointment in the hospital’s primary care center within 72 hours. Then, office-based buprenorphine treatment was provided for 10 weeks by physicians and nurses using established procedures, with visits ranging from weekly to twice monthly based on patient stability. After 10 weeks, patients were transferred for ongoing OUD medication treatment to either a community program or a clinician, or were offered medically supervised withdrawal from opioids over a 2-week period, based on their stability, preference, and insurance.
During the study period, 535 patients were deemed eligible to start buprenorphine across the three study sites. Participant demographic characteristics were not provided by the authors.
WHAT DID THIS STUDY FIND?
Starting patients on buprenorphine in the emergency department led to strong treatment retention at 30 days.
Of the 535 patients were deemed eligible to start buprenorphine across the three study sites, 241 were started on buprenorphine. Data were not provided indicating why 294 eligible patients were not initiated on buprenorphine, though it is possible many of these individuals declined the medication or left the emergency department before they could be prescribed for.
Of the 241 patients started on buprenorphine, the majority of patients were uninsured (71%), followed by being covered by Medicaid (21%), private health insurance (6%), or Medicare (2%).
Follow-up appointment attendance rates were excellent, and the majority of participants were still taking buprenorphine 30 days later.
Once receiving buprenorphine, 78% (187) of patients arrived at the follow-up appointment the next day and 59% (111) of these patients remained in treatment 30 days later. Additionally, 209 naloxone kits were distributed.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Though buprenorphine has shown to be an empirically supported treatment for OUD, accessing this medication remains a serious challenge for many individuals because of the limited availability of prescribers with the special X-license required to prescribe this medication, and because many people with OUD are under-insured, or not insured, they are less likely to have access to healthcare providers who could prescribe buprenorphine. Many have argued that by connecting people to this medication in medical settings in which individuals with OUD commonly present for medical care, this barrier could be significantly reduced. In 2015, an important study provided preliminary evidence suggesting such approaches could work. D’Onofrio and colleagues showed that initiating individuals with OUD on buprenorphine when they present to the emergency department for medical care was associated with significant improvements in 1-month OUD outcomes, including decreased opioid use (an average of 5.4 days per week of opioid use was reduced to 0.9 days per week in the medication group compared to a reduction to only 2.4 days per week of use in the comparison group’s referral to outpatient treatment) and heightened treatment engagement rates (78% of individuals receiving buprenorphine remained in treatment at 30-day follow-up versus 37% of those simply referred to outpatient treatment). Groups were however not different at 2-, 6-, and 12-month follow-up, indicating a fairly rapid decay of these beneficial effects.
Though not a randomized controlled trial like the 2015 D’Onofrio study, researchers’ findings showing 78% pf patients receiving buprenorphine in the emergency department came back the following day for additional medication, and 59% remained in treatment 30 days later are consistent with D’Onofrio and colleagues’ findings, and provide further support for the potential of this kind of OUD intervention. Though this study did not have a control group making it hard to contextualize these findings, their 59% 30-day treatment retention result looks promising compared the 37% 30-day treatment retention in the control group in the D’Onofrio study who received referral to outpatient treatment but no buprenorphine.
While the medication linkage interventions in these two studies had many similarities, the researchers intervention was distinct in that they utilized peer recovery coaches. Though the researchers’ observational study design did not allow them to draw any conclusions about the possible benefits or costs associated with utilizing peer recovery supports in this setting, previous work has shown peer recovery supports can be important contributors to engaging and retaining patients in care, and can be utilized to bridge individuals from one level of care to the next.
This paper highlights the therapeutic paradox inherent in a medical crisis: meeting patients literally ‘where they’re at’ and taking advantage of opportunities presented by a ‘reachable moment’ in the emergency department to connect them quickly to effective treatments. Individuals with OUD are often wary of medical/clinical systems and providers given the stigma of addiction and bad experiences many have had when interacting with healthcare systems/providers. Engaging patients in conversations about life saving medication for OUD when they come through the emergency department or primary care medical settings – especially through peer recovery coaches who often have more perceived credibility to those with OUD – could have massive public health benefits. This potential of recovery coach-based linkages to OUD medications, however, needs to be tested further other in real-world settings like the one described in the current feasibility study. Importantly, given the decay of these beneficial effects over time, based on the D’Onofrio and colleagues follow-up study using a very similar protocol, there may be added long-term utility in incorporating use of recovery coaches longitudinally to enhance medication adherence and facilitate linkage to other rewarding recovery support services.
- LIMITATIONS
-
- The study outcome ‘remaining in treatment’ was not defined.
- This was an implementation and observational study without a control group, making it difficult to estimate the benefits of the interventions compared to treatment as usual.
- Because all patients received medications and peer recovery coaching it is impossible to tease apart independent therapeutic benefits of each. For instance, it’s impossible to know how much of the study outcome was a function of the medication, and how much was a function of involving peer recovery coaches, both of which in their own have been shown to be helpful.
BOTTOM LINE
- For individuals and families seeking recovery: Provision of buprenorphine along with the support of peer recovery coaches was associated with promising 30-day treatment retention rates that appear to outperform usual referral to standard outpatient care. Over three quarters of patients who received buprenorphine in the emergency department arrived at a follow-up appointment the next day, and 59% of these patients remained in treatment 30 days later. Crisis also holds within it new opportunity for therapeutic action. Taking advantage of a ‘reachable moment’ in the emergency department, paradoxically may save your life.
- For treatment professionals and treatment systems: This paper highlights the importance of literally ‘meeting patients where they’re at’ and taking advantage of opportunities to connect them to safe and effective treatments when they present in crisis for medical attention. Individuals with OUD may be wary of medical/clinical systems and providers given the stigma of addiction and bad experiences many have had when interacting with healthcare systems/providers. Engaging patients in conversations about life saving medications for OUD when they come through emergency department or primary care medical settings – especially through peer recovery coaches who often have more credibility to those with OUD – could potentially have major impact on the problem of OUD. Opportunities also exist to connect people with these medications in recovery community centers. Excellent tools and resources exist to help treatment providers and systems reduce barriers to OUD medications.
- For scientists: This paper highlights the importance of literally “meeting patients where they’re at” and taking advantage of opportunities to connect patients to safe and effective treatments when they present in crisis for medical attention. Much more work is needed, however, to demonstrate the efficacy of emergency department-based buprenorphine interventions, to tease out the unique contributions medications of and peer recovery support services in such interventions, and how to extend these initial benefits over time. Further research is needed to understand how best to scale best practices learned from this research to emergency departments across the country.
- For policy makers: This paper highlights the importance of meeting patients literally ‘where they’re at’ and taking advantage of opportunities to connect patients to safe and effective treatments when they present in crisis for medical attention. Individuals with OUD are often wary of medical/clinical systems and providers given the stigma of addiction and bad experiences many have had when interacting with healthcare systems/providers. Engaging patients in conversations about life saving medication for OUD when they come through emergency department or primary care medical settings, especially through peer recovery coaches who often have more credibility to those with OUD, could potentially have massive public health benefits. Legislative changes could remove barriers, making it easier for providers to initiate buprenorphine medication in emergency and primary care medical settings.
CITATIONS
Bogan, C., Jennings, L., Haynes, L., Barth, K., Moreland, A., Oros, M., . . . Brady, K. (2020). Implementation of emergency department-initiated buprenorphine for opioid use disorder in a rural southern state. Journal of Substance Abuse Treatment, 112s, 73-78. doi: 10.1016/j.jsat.2020.02.007

