Can a brief intervention in an emergency room reduce healthcare costs 10 years later?
Despite efforts to effectively intervene with youth who show up to emergency departments with alcohol or other drug problems, a systematic review concluded that there was no clear benefit for this type of intervention in terms of substance use outcomes in the short term. But, what about how these hospital-based interventions help reduce health care utilization over the long term?
Using 10 year follow-ups, this study investigated whether healthcare costs were reduced among youth who received an intervention during a visit to the emergency department to help link them to outside alcohol and other drug services.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Hospital emergency departments provide services to a high proportion of people with risky alcohol and other drug use; therefore, they are a useful setting to evaluate the effectiveness of brief interventions. Brief interventions delivered in hospital emergency departments have often yielded positive results for adults; however, a review of brief interventions delivered in emergency departments for youth aged 21 or under provided no clear advantage for this intervention, yet follow-ups beyond 12-months are rare.
This study examined a group of participants 10 years post intervention to determine the costs and potential savings in terms of reduced emergency department costs and overall hospital costs. Another goal was to identify predictors of costs to help in directing future interventions.
HOW WAS THIS STUDY CONDUCTED?
Between 1999-2002, this study conducted a randomized trial in four Australian hospital emergency departments targeting youth aged 12-19 who presented with an alcohol or other drug related condition. Brief advice and referral to off-site treatment was tested against usual care with 127 adolescents.
Data for the 10 year follow up was collected by submitting identifying information to the Data Linkage Unit which produced participant information on mortality, hospital admissions, emergency department attendance, outpatient mental health, and use of opiate pharmacotherapies.
A total of 116 participants were successfully linked and included in the follow-up analysis (9 of the 11 people not linked were from the usual care group). For the economic analysis (i.e., healthcare costs), cost weights were obtained and applied to the variables in order compare the usual care group with the intervention group.
WHAT DID THIS STUDY FIND?
The intervention significantly reduced rates of presentation for mental health, alcohol, and other drug use in the emergency department at 10 year follow-ups.
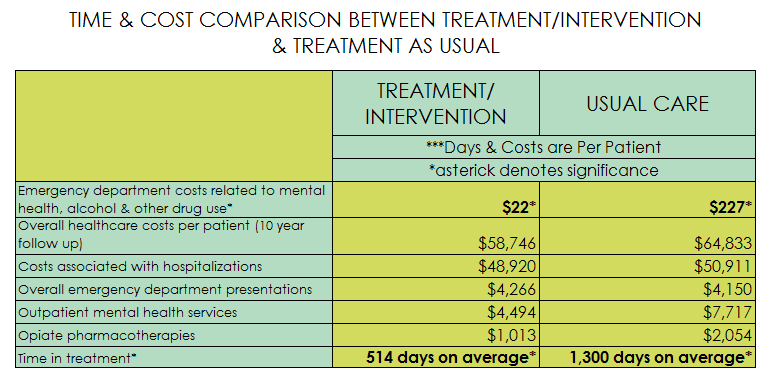
By extension, emergency department costs related to mental health, alcohol, and other drug use were lower in the treatment group ($22 per patient) compared to the usual care group ($227 per patient). However, the intervention did not significantly reduce overall healthcare costs per patient (intervention $58,746 versus usual care $64,833), costs associated with hospitalizations (intervention $48,920 versus $50,911), overall emergency department presentations (intervention $4,266 versus $4,150), outpatient mental health services (intervention $4,494 versus $7,717), or opiate pharmacotherapies (intervention $1,013 versus $2,054) yet still showed a pattern of trends towards significance.
Notably, participants in the intervention group spent significantly shorter time in treatment for substance use disorders (514 days on average) compared to the control group (1,300 days on average).
Five deaths were observed during the 10-year follow-up; however, rates of mortality were not significantly different between groups.
A number of baseline variables were predictive of costs. Primary alcohol use was associated with lower costs, whereas injecting drug use was associated with increased costs over the 10 year study.
Further analysis was conducted on the intervention group only (n = 60) because just under half (n = 28; 46.7%) received follow-up contact from a linkage worker after the intervention (which was largely referral focused).
The half that also received follow-up contact from a linkage worker has lower costs on average than the half that received the intervention alone ($36,108 versus $78,511).
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study cohort had high healthcare costs ($6,200 per person/year) compared to Australian national averages ($1,532 per person/year) which identifies this group as a high priority for intervention for both healthcare and financial reasons.
At 10 year follow-ups, this referral-focused intervention was successful at reducing mental health, alcohol, or other drug presentations by young people in emergency departments.
Other healthcare costs appeared to be reduced but not significantly. The cost of the intervention was estimated at $55 per patient and takes approximately 1 hour.
There were several non-significant findings regarding overall costs comparisons. The authors suggest that although these results were non-significant they still showed the potential to have economic impacts.
- LIMITATIONS
-
- The intervention was not shown to reduce costs associated with overall healthcare services. However, given that slightly less than half of the participants in the intervention group actually received follow-up contact from the linkage worker, and by 12 months only 12 participants accessed an external treatment service (compared to 4 in the control group), the study was potentially underpowered to detect this effect.
- Despite the small sample sizes, which was an obvious major limitation of the study, the intervention still showed noticeable and stable trends towards financial reductions in many domains.
NEXT STEPS
The authors suggested that if a new component was developed from this intervention, it should be an attempt to gain the young person’s consent to contact significant others to increase engagement.
BOTTOM LINE
- For Individuals and families seeking recovery: This referral-focused intervention was helpful in reducing mental health, alcohol, and other drug use related conditions among youth who show up in an emergency department. However, overall healthcare costs unrelated to mental health, alcohol, or other drug use were not reduced. This shows the value that even a brief intervention can have on long-term mental health, alcohol, and other drug-related conditions when delivered in an emergency department setting.
- For scientists: After 10 years, this intervention was able to reduce rates of emergency department utilization and costs associated with mental health, alcohol, and other drug use among youth. Other healthcare costs were not significantly reduced; however, the financial impact may still be noticeable. More research needs to be done on the long-term financial impact of emergency department based interventions for youth using larger sample sizes in areas in addition to Australia.
- For policy makers: The findings provide information on where limited resources could be directed to potentially reduce future costs and morbidity. In Australia, the average per person/year healthcare costs for 15–24 year olds in hospital inpatient, outpatient, and prescriptions in 2015 was $1,532. In this study, the average healthcare cost per person was $6,200 per person/year. Additionally, injecting drug use was a robust predictor of increased future healthcare costs. This intervention was associated with reduced emergency department costs associated mental health, alcohol, and other drug use among youth. Thus a greater focus on intervening with youth in EDs could be highly cost-effective.
- For treatment professionals and treatment systems: This brief intervention was referral-focused and yielded reductions in subsequent mental health, alcohol, and other drug-related costs in emergency department settings among youth. There was no group difference in costs related to pharmacotherapy (e.g., methadone or buprenorphine); however, the pharmacotherapy treatment time was significantly shorter among the treatment group (514 days versus 1,300 days). This was a rigorous and well designed study that suggests a brief intervention could yield considerable reductions in healthcare costs related to emergency department mental health, alcohol, and other drug related costs.
CITATIONS
Tait, R. J., Teoh, L., Kelty, E., Geelhoed, E., Mountain, D., & Hulse, G. K. (2016). Emergency department based intervention with adolescent substance users: 10 year economic and health outcomes. Drug and Alcohol Dependence, 165, 168-174. doi: 10.1016/j.drugalcdep.2016.06.005.

