Addiction Consultations in the Hospital Save Big!
In a hospital, consultation/liaison services are specialty services provided bedside directly to the patient.
While many hospitals have begun to integrate addiction-related consultations into regular inpatient care, its real-world benefits have rarely been investigated scientifically.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Addiction consultation/liaison (CL) services are interventions that are provided for individuals admitted to a hospital for another health condition. For example, the addiction CL service may be called to meet with an individual hospitalized for liver dysfunction if he/she has a suspected drinking problem.
While consultation/liaison (CL) services are intuitively part of quality clinical care, & may facilitate referrals, linkages, and entry into specialty treatment, little is known about the actual benefit provided by these services.
To help shed light on this issue, Reeve and colleagues conducted this naturalistic study of addiction consultation/liaison (CL) services on future health care utilization and cost-benefit for individuals with suspected alcohol or other drug problems to help shed light on this issue.
HOW WAS THIS STUDY CONDUCTED?
The study was conducted at eight hospitals in New South Wales, Australia for 1615 patients, all of whom were 17 years or older (41 years old, on average) and could provide consent to participate. Of these, 1101 gave permission for study authors to obtain follow-up health care data to analyze benefits of addiction consultation/liaison (CL) services. Patient data were obtained across a 2.5-year period: 1.5 years before they were assessed in the hospital, and 1 year after they were assessed.
The analyses focused on the change in trends from the time before the hospital admission to the time after the hospital admission. This “interrupted time-series” study design is a common method for trying to determine whether a naturalistic intervention not implemented or controlled by the research team was likely responsible for any observed changes in the patient after receiving the intervention – addiction consultation/liaison (CL) in this case.
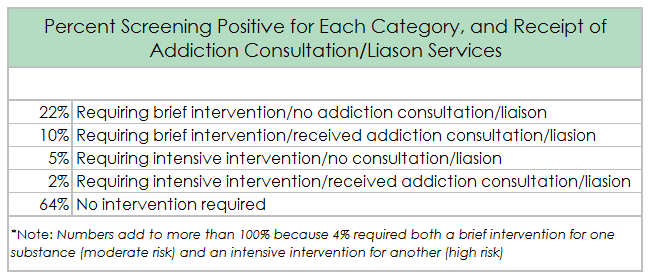
Based on the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) a substance use problem screening instrument created by the World Health Organization, given while they were in the hospital, authors created four groups of patients:
- No or lower risk for alcohol or other drug problem not requiring intervention
- Moderate risk for problem requiring brief intervention, but no Addiction consultation/liaison (CL) received
- High risk for problem requiring intensive intervention, but no Addiction consultation/liaison (CL) received
- Addiction consultation/liaison (CL) received
Specific attention was paid to the comparison between groups 3 and 4 in this study because those at high risk for having an alcohol and other drug problem have the greatest potential to benefit from a bedside intervention intended to facilitate engagement in specialty addiction treatment.
WHAT DID THIS STUDY FIND?
Controlling for a host of demographic factors, and the hospital to which the individual was admitted, for those who screened positive for high risk of having an alcohol or other drug problem requiring intensive treatment, receiving consultation/liaison (CL) was related to greater likelihood that the patient later would be admitted to the hospital within common hospital benchmarks of 4 hours and 8 hours after a decision was made to admit the patient – these benchmarks are measures of hospital efficiency and safety.
Receiving consultation/liaison (CL) was also related to more prescription drug use for medications associated with the treatment of alcohol and other drug use disorder.
However, there is no discernible impact of consultation/liaison (CL) on subsequent medical service utilization. While those who received CL services may spend fewer hours in the emergency room and an overall decrease in overall hospital admissions, these differences were not statistically significant (i.e., were not large enough to be considered statistically reliable).
Importantly, from the perspective of the hospital, providing addiction consultation/liaison (CL) services was related with a cost-savings in terms of subsequent health care service utilization.
For each patient receiving consultation/liaison (CL) for the first time in a given year, the hospital saves an average of $203 dollars per year. For the hospitals examined in this study, based on the number of patients receiving CL, this results in savings of more than $100,000 Australian dollars ($73,000 U.S. dollars) even after accounting for the cost of implementing the CL service.
WHY IS THIS STUDY IMPORTANT?
This study is important as an initial step in determining the benefits of providing addiction consultation/liaison (CL) services in a medical hospital.
While based only on this study consultation/liaison (CL) services may not provide much health care utilization benefit from the perspective of the individual, there were noteworthy cost-savings from the perspective of the hospital, over $200 per patient per year.
Almost 40% of the patients in this study screened positive for an alcohol or other drug problem requiring treatment. In other words, addiction related problems are common in general medical settings.
- LIMITATIONS
-
- Individuals were not randomly assigned to receive addiction consultation/liaison (CL) or not. Thus, while the authors designed a rigorous study to investigate the benefits provided by addiction CL services, it is not certain that any benefits described, such as cost savings, were entirely attributable to the addiction CL services themselves.
NEXT STEPS
One seemingly logical next step is to test a semi-structured addiction consultation/liaison (CL) intervention in a randomized controlled trial against, for example, usual medical care.
BOTTOM LINE
- For individuals & families seeking recovery: Addiction-related consultation/liaison (CL) services in the hospital are designed to help address alcohol and other drug problems for people admitted for another, potentially related, medical problem. Whether CL services offer you benefits in the long-run is not yet clear at this point. It is possible that receiving this service could save you health care dollars overall in the long run, but more research is needed to say this with confidence. Models of care are being developed that add case managers or “recovery coaches” in addition to CL services, to help patients after hospital discharge to link with other services and become involved with community resources that can support recovery but these also need further evaluation.
- For Scientists: In this well-designed study, authors conducted a naturalistic investigation of addiction consultation/liaison services in the hospital. Given the potential cost-benefit of providing these services, future randomized controlled trials could help determine whether these services promote better patient outcomes.
- For Policy makers: In this well-designed study, authors conducted a naturalistic investigation of addiction consultation/liaison services in the hospital. Given the potential cost-benefit of providing these services, future randomized controlled trials could help determine whether these services promote better patient outcomes.
- For Treatment professionals and treatment systems: In this well-designed study, authors conducted a naturalistic investigation of addiction consultation/liaison (CL) services in the hospital. Addiction CL services appear to provide cost-benefit in terms of reduced health care costs over a 1-year period following the intervention. Given this potential cost-benefit, future randomized controlled trials could help determine whether these services also promote better patient outcomes.
CITATIONS
Reeve, R., Arora, S., Butler, K., Viney, R., Burns, L., Goodall, S., & van Gool, K. (2016). Evaluating the impact of hospital based drug and alcohol consultation liaison services. Journal of Substance Abuse Treatment.

