Weighing the evidence for spiritual and religious interventions for substance use problems
Spiritual and religious interventions are commonly used to treat substance use disorder, and findings from a number of randomized controlled trials suggest such interventions are effective. And yet it has been over a decade since this evidence has been weighed in a meta-analysis – a statistical approach that can assess findings from multiple studies to determine whether, taken together, they suggest a treatment works. This study brings us up to date with a meta-analysis of spiritual and religious interventions for substance use disorder that includes all randomized controlled trials on this subject from 1990-2018.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
During the first half of the 20th century and through the 1970s, the treatment of substance use disorder was largely separate from traditional health care systems, including both medicine and psychological treatments. In part due to this siloing of substance use from the rest of health care, during this same time period, spiritual and religious based approaches gained in popularity at the community level, and anecdotally many individuals who engaged with these approaches found them helpful. Interventions that leveraged spiritual and religious principles, like those that facilitated engaging with 12-step mutual-help group principles, predominated available treatments, particularly in residential programs (e.g., the 28-day “Minnesota Model”). Even though there are now, of course, many empirically-supported interventions that leverage biological, psychological, and social models of substance use disorder recovery, spiritual and religious based interventions continue to be widely used. Criticisms of these approaches have been levelled in the lay and scientific media, though evidence supports the utility of participation in 12-step mutual-help organizations, which is one ostensibly spiritually-based approach.
Reviews and meta-analyses of the literature can help weigh and synthesize findings from a body of work such as this to get a sense of whether, on the whole, a treatment or approach is effective. However, of the five related reviews on spiritual and religious interventions done before this study, none included evidence generated after 2006, and all had significant methodological limitations. The authors of this study sought to redress this by conducting a meta-analysis incorporating all randomized controlled trials on spiritual and religious interventions for substance use disorder conducted from 1990-2018 to examine spiritual and religious interventions’ capacity for reducing substance use and enhancing participants’ wellbeing from psychological, social, and spiritual perspectives.
HOW WAS THIS STUDY CONDUCTED?
This was a meta-analysis of the literature on spiritual and religious interventions for substance use disorder conducted from 1990-2018. To identify relevant papers on this topic, the authors used gold-standard, Cochrane recommendations for identifying randomized controlled trials. As is typical in meta-analytic studies, major electronic research publication databases were searched. These included: PsycINFO, SocINDEX, Religion and Philosophy Collection, MEDLINE, CINAHL Plus with Full Text, PsycARTICLES, Psychology and Behavioral Sciences Collection, Dissertations and Theses Global, National Registry of Evidence-based Programs and Practices, and Specialized Register of Trials of the Cochrane Group on Drugs and Alcohol.
To be included in the final meta-analysis, studies needed to meet the following requirements: 1) They must have employed a randomized controlled trial design. 2) Studies needed to include participants with substance use problems, though a formal SUD diagnosis was not required. 3) Studies must have examined spiritual and religious interventions’ effectiveness and/or efficacy for treating or preventing substance use problems. The authors defined spirituality as the “universal and fundamental human quality of searching for meaning, well-being, and profundity through connections with oneself, others, and the universe,” and religion as an “institutionalized system of beliefs, values, and practices oriented towards spiritual concerns and transmitted over time by a community.” Thus, religiosity in this study refers to “membership and participation in an organized religion.” Since interventions had to be themselves spiritual or religious, studies of interventions designed to simply increase 12-step fellowship attendance through referral were excluded. Of note, mindfulness-based interventions were also excluded. 4) Studies needed to include a control condition defined as inactive controls (no treatment, waiting list control, standard care) or active controls (bona fide non-spiritual/religious interventions, such as cognitive-behavioral approaches). 5) Studies had to focus on substance use outcomes (e.g., use frequency, abstinence rate), spiritual and religious outcomes (e.g., spiritual wellbeing, daily spiritual experience, religious practice, spiritual coping), psychological outcomes (e.g., depression, anxiety, self-efficacy), and/or social outcomes (e.g., employment, relationship status). Studies that measured psychosocial-spiritual outcomes but not substance use outcomes were included because psychological, social, and spiritual and religious outcomes are important contributors to addiction recovery, based on several existing definitions like that of the Substance Abuse and Mental Health Services Administration. Studies analyzing only treatment retention or 12-step mutual-help organization attendance outcomes were excluded. After removing duplicates, 2306 articles remained for screening; 2100 articles were excluded based on titles and abstracts; and 186 articles were excluded in full-text review. In total, 20 studies from 20 articles met inclusion criteria and were included in the final review. Four studies used inactive controls (i.e., control participants were not provided with any active treatment), 14 used active controls (i.e., control participants received some kind of SUD intervention), and two used both inactive and active controls.
Sixteen of the 20 studies included in the meta-analysis (80%) tested 12-step-related interventions like 12-Step Facilitation. Four studies (20%) investigated the efficacy of non-12-step-oriented spiritual and religious interventions. Seven spiritual and religious intervention studies (35%) were implemented in group format, six (30%) in individual format, four (20%) in group and individual format, and three (15%) did not report format. Treatment length ranged from six to 60 sessions, and intensity ranged from one to three sessions per week. The spiritual and religious interventions in nine studies (45%) were manualized, and two (10%) were partially manualized.
The combined studies had a total of 3700 participants. Individual study samples sizes ranged from 30 to 952. Sixteen studies (80%) were conducted in the United States, one in Nigeria, two in Iran, and one in Canada. Four studies (20%) used inactive controls, 14 (70%) used active controls, and two (10%) used both. Comparison interventions included Cognitive Behavioral Therapy, integrated Cognitive Behavioral Therapy, Acceptance and Commitment Therapy, methadone maintenance treatment, family-of-origin therapy, clinical management, group drug counseling, minimal treatment approach, guided imagery, Motivational Enhancement Therapy, and the Community Reinforcement Approach. Of the 15 studies that measured substance use outcomes, four relied solely on self-reports, while 11 used methods considered more reliable (e.g., laboratory tests, collateral- plus self- reports). All 12 studies that measured psycho-social-spiritual outcomes used standardized self-report measures.
The authors calculated average effect sizes reflected by Cohen’s d statistic. Cohen’s d around 0.20 is considered a small effect, while 0.50 is considered a medium effect, and 0.80 is considered a large effect. In addition to overall effect sizes of the overall efficacy of spiritual/religious interventions, effect sizes for substance use outcomes (e.g., days of use in previous 90 days, days to relapse) and for psychosocial-spiritual outcomes (e.g., religious practice, spiritual coping, depression, anxiety, self-efficacy, self-esteem, employment, relationship status) were also calculated separately.
WHAT DID THIS STUDY FIND?
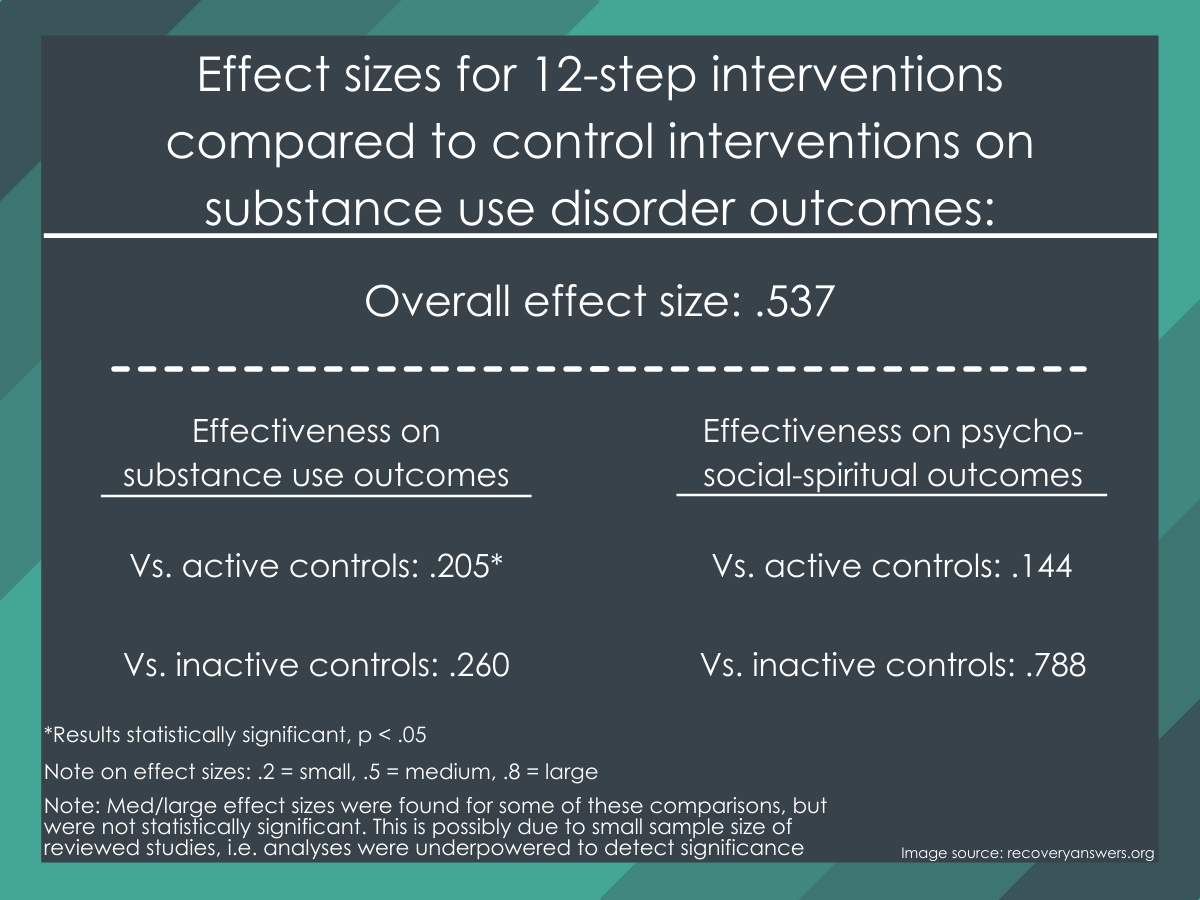
Figure 1.
Studies with inactive controls.
The average overall effect size representing the absolute efficacy of spiritual and religious interventions when compared with inactive controls (calculated using 37 effect sizes derived from six studies) was medium (d= .537), but not statistically significant. It is unusual that a medium effect size would not be statistically significant (meaning the probability of this finding being a result of randomness or chance is less than 5%). In this case, the non-significant effect is most likely related to the small number of studies included in this aspect of the meta-analysis, because smaller samples reduce statistical ability to detect significance.
Studies with active controls.
Notably, the bulk of studies with active control groups included in this meta-analysis used in their calculation were 12-Step Facilitation randomized controlled trials. The average overall effect size representing the relative efficacy of spiritual and religious interventions when compared with active controls (with 92 effect sizes from 16 studies) was small (d= .176) but statistically significant. As an example of one such study included in the meta-analysis, Carroll and colleagues compared 12 sessions of 12-Step Facilitation + disulfiram (a medication commonly used to treat alcohol use disorder, better known by its trade name Antabuse) to standard counseling + disulfiram for 112 adults with cocaine dependence. They found that assignment to 12-Step Facilitation was associated with small to medium effect size reductions in cocaine use throughout treatment and a higher number of cocaine-negative urine samples compared to standard counseling.
The authors of this meta-analysis also checked numerous characteristics that may differ between studies to determine if they may have influenced findings (e.g., sample differences in race/ethnicity, ratios of women to men). Only countries in which studies were conducted were shown to significantly influence results. However, because of the very low number of studies conducted in countries other than the United States, confidence in this finding is very low.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
The study authors found evidence of the capacity for spiritual and religious interventions to aid substance use problem recovery. It is important to note, however, that all trials comparing spiritual and religious interventions to an active control group included in their meta-analysis (16 of 20) were on 12-step based interventions (primarily 12-Step Facilitation), and as such these results don’t necessarily speak to the breadth of spiritual and religious interventions for substance use disorder.
Results of this meta-analysis show benefits to patients from 12-step based interventions in terms of substance use outcomes, although the aggregated effect size was small.
In terms of effects on psychosocial and spiritual outcomes, taken together, spiritual and religious interventions’ did better when compared to a no-treatment (inactive) control group, but no better than active control groups, who mostly received Cognitive Behavioral Therapy.
It is important to note that these findings do not speak directly to the efficacy of 12-step fellowships per se (e.g., AA, NA), because most active studies included in the meta-analysis tested either professionally delivered 12-Step Facilitation or 12-step-oriented treatments in the context of formal recovery programs. That said, in studies where AA participation has been examined, the theoretically-consistent mediator of the benefit from professionally-delivered 12-Step Facilitation supports AA being the main reason why people are doing better (see Walitzer et al., 2009; Litt et al., 2009; Longabaugh et al., 1998).
It is also important to note that 12-Step Facilitation does not necessarily aid addiction recovery because it has a “spiritual” orientation. Rather, it is thought to work by connecting patients to AA and NA. In turn, AA and NA are thought to support recovery through multiple mechanisms, particularly through their ability to effect changes in individuals’ social networks. Notably, spiritual mechanisms in 12-step programs are thought only explain a small amount of their effect, and may only be important for those with more severe addiction.
Given that the 12-step based interventions included in this meta-analysis were all compared to active controls (i.e., control participants were receiving some other kind of active substance use disorder treatment), we would expect differences between groups to be fairly small because both study groups were receiving active treatments. The authors’ findings suggest 12-step based interventions slightly outperform other well-established treatments like Cognitive Behavioral Therapy, Motivational Enhancement Therapy, and Community Reinforcement Approach. Conversely, the non-12-step based spiritual/religious interventions in this meta-analysis, which were compared to control groups in which participants were not receiving an active treatment, showed a larger effect size improvement in substance use outcomes, but because these interventions were compared against no active treatment, we would expect them to fare better. This kind of comparison, however, is less helpful, as it tells us little about the relative effectiveness of this class of interventions.
The health care cost savings of 12-step interventions also bears consideration. For instance, substantial health care costs savings have been found for patients treated in 12-step compared to cognitive-behavioral treatments with 12-step treatment simultaneously producing substantially better abstinence outcomes. Greater use of community AA/NA services among those receiving 12-step-based treatments and greater use of professional health care services among those receiving cognitive-behavioral based treatments explains these lower costs for 12-step treatments.
- LIMITATIONS
-
- Ultimately, because of the available religious/spirituality intervention literature, this meta-analysis focused largely on studies of 12-step related interventions as “spiritual” interventions. This limits the generalizability of these findings to less commonly used spiritual and religious based substance use disorder treatments.
- Excluding non-randomized controlled trial studies and studies that failed to report sufficient effect size data limited the evidence gathered for this review and neglected potentially valuable information that studies with other research designs may provide.
- This review examined only the efficacy of spiritual and religious interventions and not the mechanisms through which spiritual and religious interventions exert their effects due to limited information provided in the primary studies. Findings supporting certain spiritual and religious interventions’ efficacy do not imply that the spiritual and religious mechanism is the only mechanism operating or that it is operating at all.
BOTTOM LINE
- For individuals and families seeking recovery: Findings from this meta-analysis of spiritual and religious interventions for substance use problems suggest 12-Step Facilitation is slightly more effective than other well-established treatments, such as cognitive-behavioral interventions, but more research is needed to properly determine the effectiveness of other less commonly utilized spiritual and religious interventions. Because 12-Step Facilitation works by connecting individuals to 12-step programs, if 12-Step Facilitation is not available in a particular clinical program, a viable alternative is to simply attend and participate in community-based 12-step programs as other studies have shown this to also confer recovery benefits.
- For treatment professionals and treatment systems: Findings from this meta-analysis of spiritual and religious interventions for substance use problems suggest 12-Step Facilitation is slightly more effective than other well-established treatments, such as cognitive-behavioral interventions, but more research is needed to properly determine the effectiveness of other less commonly utilized spiritual and religious interventions. Because 12-Step Facilitation is more cost-effective than Cognitive Behavioral Therapy and produces slightly better short-term and better long-term outcomes, it should be considered as a treatment option in clinical settings.
- For scientists: Findings from this meta-analysis of spiritual and religious interventions for substance use problems suggest 12-Step Facilitation is slightly more effective than other well-established treatments, such as cognitive-behavioral interventions, but more research is needed to properly determine the effectiveness of other less commonly utilized spiritual and religious interventions, which have largely been tested with less rigorous, inactive control groups. Randomized controlled trials of non-12-step based spiritual and religious substance use disorder interventions are needed.
- For policy makers: Findings from this meta-analysis of spiritual and religious interventions for substance use problems suggest 12-Step Facilitation is slightly more effective than other well-established treatments, such as cognitive-behavioral interventions, but more research is needed to properly determine the effectiveness of other less commonly utilized spiritual and religious interventions. Providing access to empirically supported treatments like 12-Step Facilitation has the potential to improve substance use disorder recovery rates and reduce healthcare costs as these interventions are typically brief, low cost, and produce better long-term recovery outcomes by connecting patients to 12-step community groups that other research has shown mobilizes the same kinds of recovery-related therapeutic mechanisms that are mobilized by professionally-delivered addiction care but is able to do this for free over the long-term in the communities in which people live.
CITATIONS
Hai, A. H., Franklin, C., Park, S., DiNitto, D. M., & Aurelio, N. (2019). The efficacy of spiritual/religious interventions for substance use problems: A systematic review and meta-analysis of randomized controlled trials. Drug and Alcohol Dependence, 202, 134-148. doi: 10.1016/j.drugalcdep.2019.04.045

