Evolving approaches to opioid use disorder treatment: A novel, community-based model for expanding treatment access
Opioid use disorder continues to be a major public health problem in the United States. Recent efforts to address treatment barriers have led to the development of innovative and effective approaches. In line with ongoing efforts to improve treatment access, engagement, and retention, this article proposes a new and comprehensive model for addressing opioid use disorder that combines and builds upon these newly emerging approaches by combining recovery community support with access to prescribed buprenorphine/naloxone (i.e., Suboxone) or long-acting injectable naltrexone (i.e., Vivitrol).
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Opioid misuse, overdose, and related disorders continue to be a major public health problem in the United States. Approximately 11.4 million Americans misused opioids in the past year, over 130 opioid-related overdose deaths occur daily, and 2.1 million Americans meet criteria for opioid use disorder. While there are effective treatments (e.g., medication, harm-reduction, residential treatment), less than 30% of the population needing opioid use disorder treatment receives it. There are several barriers to treatment access, including funding,treatment capacity, patient motivation, and patient access. In recognition of these barriers, government agencies, researchers, clinicians, and the general community have begun to address them by developing and testing new treatment approaches. These approaches include, for example, emergency department referrals to treatment, buprenorphine/naloxone (i.e., Suboxone) treatment initiation in the emergency department, the incorporation of recovery support services and harm reduction services in community organizations, and low-threshold programs that encourage treatment engagement and retention by implementing a more flexible treatment model (e.g., not requiring counseling or routine drug testing). Many of these new treatment approaches have shown to be effective for treatment engagement and retention, even among high-risk and treatment resistant populations. Despite the success of these programs, more work is needed to further improve opioid use disorder treatment and limit barriers to its access. Combining elements of and building upon some of these promising treatment approaches, this article proposes a new comprehensive model for opioid use disorder treatment to engage individuals outside of traditional healthcare systems – the Recovery Community Center Office-Based Opioid Treatment model.
HOW WAS THIS STUDY CONDUCTED?
The current manuscript outlines a treatment design proposal based on two general models of care, including a community-based model and a medical/professional model. The proposed treatment design was developed by a diverse group of academic and federal-agency researchers, and peer-based community partners, including individuals participating in peer-led recovery community organizations.
The Recovery Community Center Office-Based Opioid Treatment model is based on several promising community-based and professional treatment approaches including: 1) Hybrid recovery community organizations: A combination of recovery support services and harm reduction services tailored to a community’s particular needs; 2) Office-based pharmacotherapy programs: Medication treatment (i.e., Suboxone) for opioid use disorder, provided by a primary care physician in an office-based setting rather than a treatment-specific setting; 3) Emergency department pharmacotherapy programs: Providing emergency department patients with a 3–day prescription of Suboxone and linkage to community-based pharmacotherapy providers; 4) Low-threshold treatment programs: Opioid use disorder treatment programs that are less strict and more flexible than traditional treatment programs (e.g., less emphasis on drug testing, abstinence, and psychosocial support, more flexible medication treatment plans, shorter waitlists and lower cost) in an effort to minimize barriers to treatment. The Recovery Community Center Office-Based Opioid Treatment model is proposed as a way to expand the availability and accessibility to treatment, and to keep opioid use disorder patients engaged once they start treatment.
The authors propose two situations in which an individual is linked to this model of care: 1) Overdose event scenario: When an individual arrives at the emergency department after an opioid–related overdose; 2) Non-overdose event scenario: When individuals are referred by a hybrid recovery community organization without an overdose event.
WHAT DID THIS STUDY FIND?
Linkage to Care – Overdose Event Scenario
If an individual overdoses and arrives at the emergency department, a peer recovery support specialist would offer medication treatment for opioid use disorder.
- If individuals decide to engage in Suboxone treatment, the emergency department would provide the patient with:
- The first dose of Suboxone.
- A 3-day Suboxone prescription.
- Linkage to a hybrid recovery community organization.
- If Suboxone treatment is not available in the emergency department, the patient would:
- Be stabilized at the emergency department.
- Initiate Suboxone at the recovery community center as soon as possible (under the supervision of on-call medical staff).
All patients would also have the option to be treated with long-acting injectable naltrexone (i.e. Vivitrol), instead of Suboxone.
- If Vivitrol is preferred over Suboxone, the patient would:
- Be provided with referrals to medical withdrawal management programs, since detoxification from opioids is necessary before taking Vivitrol.
- Start Vivitrol treatment at the recovery community center after detoxification.
- Receive the Recovery Community Center Office-Based Opioid Treatment model of care at the recovery community center.
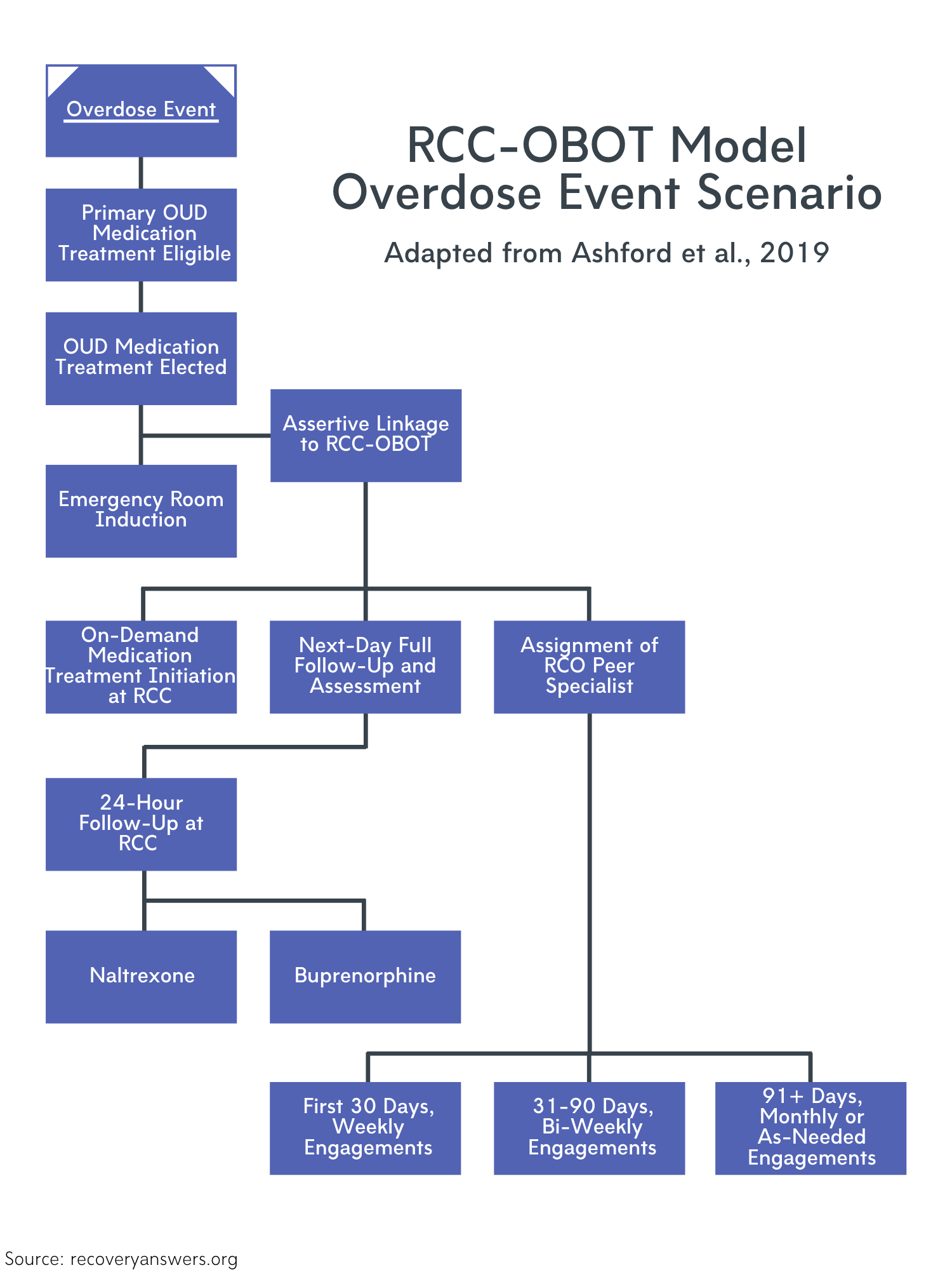
Figure 1.
Linkage to Care – Non-Overdose Event Scenario
In non-overdose scenarios, individuals would be linked to the hybrid recovery community organization through referrals (e.g., from the criminal justice system, social and health services, recovery community organization peers, walk-ins). The individual would be screened for opioid use disorder and whether pharmacotherapy is right for them. Once deemed eligible for the program, the patient would discuss treatment options with a peer recovery support specialist.
- If individuals decide to engage in Suboxone treatment:
- Patients would immediately start Suboxone treatment under the Recovery Community Center Office-Based Opioid Treatment model of care.
- If Vivitrol is preferred over Suboxone:
- Vivitrol treatment would be started at the hybrid recovery community center under the Recovery Community Center Office-Based Opioid Treatment model of care.
Model of Care After Initial Medication Exposure
- Suboxone patients would:
- Receive their daily Suboxone dose in-person at the recovery community center for the first 30 days.
- Attend bi-weekly follow-ups and receive 14-day Suboxone prescriptions for the next 30 days.
- Attend monthly follow-ups and receive 30-day Suboxone prescriptions after day 60 of treatment.
- Vivitrol patients would:
- Attend monthly follow-ups.
- Receive monthly injections of Vivitrol.
- All patients would:
- Be assigned a peer recovery support specialist, who provides peer-based recovery support and recovery management.
- Engage with their peer support specialist at least weekly for the first 30 days, bi-weekly for the next 30 days, and monthly or as-needed after 60 days of treatment.
- Develop a goal-oriented plan for recovery (housing, education, health, and employment) with their peer specialist.
- Receive direct links to outside addiction and mental/physical health services from their peer specialist.
- Receive naloxone (overdose reversal medication) and education in harm-reduction techniques within the first 14 days of the program.
- Participate in the program for as long as they choose to.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
The author’s proposed model of care is a response to the opioid and overdose crisis. The Recovery Community Center Office-Based Opioid Treatment model is a comprehensive approach to opioid use disorder treatment that has the potential to enhance treatment access, engagement, and retention. Combining proactive referral services, medication treatment, harm-reduction education, peer-based support, and the flexibility of a low-threshold program might open treatment up to individuals who do not otherwise have access to it.
Harm-reduction education and low-threshold programs may be particularly useful for enhancing treatment engagement among individuals who are clinically high-risk (e.g., individuals who engage in injection drug use) and/or experiencing several psychosocial challenges (e.g., housing insecure or experiencing homelessness). This model’s use of proactive referrals means that more people will be aware of and offered resources that may not otherwise be accessible to them. In addition, providing naloxone and educating patients about ways to reduce their risk of harm could ultimately help reduce high rates of opioid-related overdoses. Though traditional treatment programs aid the recovery of many individuals, not all individuals have the resources or recovery capital to access and engage in traditional services. This low-threshold model proposes one way to engage and support the broader population of individuals suffering from opioid use disorder.
Offering both Suboxone and Vivitrol, the proposed treatment model ensures that individuals have treatment options regardless of their preference for an opioid agonist (Suboxone) or opioid blocking (Vivitrol) medication. Moreover, regular check-ins and no pre-defined treatment ‘end-date’ promotes treatment engagement and retention, as well as individualized care that can adapt to disorder severity. A peer-based model of support also presents a cost-effective approach to providing recovery services. Studies show that peer recovery support improves relationships, treatment satisfaction, and retention, and reduces risk of relapse. Peer-based support outside of mutual help organizations like Narcotics Anonymous may also help patients avoid stigma and judgement around their medication treatment.
A similar model of addiction care (medication, counseling, and recovery coaching) implemented in primary care settings has shown to yield benefits that go beyond patient outcomes, by reducing the costs associated with providing more intensive care (inpatient, emergency department). Whereas a primary care model fails to reach many individuals, the current model would help expand treatment access to a broad array of individuals with opioid use disorder. Although this model has not been tested, it is an important step toward thinking about various pathways to help support individuals with substance use disorders outside of traditional healthcare settings.
- LIMITATIONS
-
- This model is not accompanied by a plan for payment and reimbursement for facility services. It is necessary to determine the most cost-effective operational methods for reimbursing medical services and managing costs associated with hiring/maintaining medical staff.
- This treatment approach has not yet been tested clinically and research is needed to determine its effectiveness and public health impact relative to other established models.
- Related to the need to test this overall model empirically, while there is a large body of research supporting medications for opioid use disorder, there is very little research on recovery community organizations. Given that only three data-driven reports have been published to-date, the research conducted thus far does not yet allow us to make conclusions about its utility.
- This model proposes many programmatic details that are in contrast to standard treatment guidelines (ASAM and SAMHSA). Differences in follow-up frequency, drug testing, and concurrent psychosocial support require testing and validating these treatment methods to ultimately gain broad public support for this treatment approach.
BOTTOM LINE
- For individuals and families seeking recovery: This article proposes a new approach to opioid use disorder treatment that has the potential to improve treatment access, engagement, and retention, particularly among high risk and treatment resistant individuals. Given that a high percentage of individuals that need opioid use disorder treatment do not receive it, it is important to think about alternative ways that we can provide treatment to everyone that needs it. Although additional research is needed to test the effectiveness of this model and develop plans for its funding and programming, it offers a new way to expand treatment access and engage people in treatment who may not seek out traditional services.
- For treatment professionals and treatment systems: This article proposes an integrative opioid use disorder treatment model that combines proactive referral services, pharmacotherapy, harm-reduction education, peer-based support, and low-threshold programs. Specifically designed to expand treatment outside of traditional healthcare settings, this model has the potential to enhance treatment access, engagement, and retention among high-risk and treatment-resistant individuals. Less than 30% of the population needing opioid use disorder treatment receives it. Although additional research is needed to test this low-threshold treatment model, it offers a novel way to enhance engagement among individuals who would not otherwise use traditional services.
- For scientists: The authors of this manuscript proposed a new model of opioid addiction treatment that aims to expand treatment access outside of traditional healthcare settings. Combining the elements of proactive referral services, pharmacotherapy, harm-reduction education, peer-based support, and low-threshold programs, this treatment model has the potential to enhance treatment access, engagement, and retention among high-risk and treatment-resistant individuals. Given the disparate rates of opioid use disorder and treatment-seeking, additional research is needed to test the feasibility and effectiveness of this treatment approach, to develop the financial components of this model, and measure its impact on society. Further investigation of treatment models that address barriers to treatment could ultimately help address the opioid epidemic.
- For policy makers: This article proposes a new comprehensive approach to opioid use disorder treatment that has significant potential to enhance treatment access, engagement, and retention, particularly among high-risk and treatment-resistant individuals. Given that less than 30% of the population needing opioid use disorder treatment actually receives it, it is critical to develop new ways of providing treatment to the broader substance use disorder population. Additional funding is needed to study this model’s effectiveness. Importantly, this clinical service delivery model does not speak to the financial components of the policy and it will be important to develop a plan for funding and maintaining this model. Nonetheless, proposing a low-threshold treatment model is the first step toward expanding treatment access to individuals who may not otherwise engage in traditional services.
CITATIONS
Ashford, R. D., Brown, A. M., McDaniel, J., Neasbitt, J., Sobora, C., Riley, R., … & Curtis, B. (2019). Responding to the opioid and overdose crisis with innovative services: The recovery community center office-based opioid treatment (RCC-OBOT) model. Addictive Behaviors, 98(106031), (Epub). doi: 10.1016/j.addbeh.2019.106031

