Having Insurance Increases Treatment-Seeking in People Who Inject Drugs: results from a 12 year study
US health policies such as the Affordable Care Act and its related Medicaid expansion helped increase access to health insurance for low-income and other vulnerable groups. This study explored if specific types of health insurance were associated with seeking specialty treatment; buprenorphine (a medication used to treat opioid use disorder often prescribed in combination with naloxone and known by the brand name Suboxone); and consistent medical care among people who inject drugs.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Expanding access to evidence-based substance use treatment is critical to reducing opioid poisonings in the United States. Medications like buprenorphine (often prescribed in a formulation with naloxone, known better by its brand name Suboxone) and methadone are more effective at treating opioid use disorder than psychosocial treatments alone. Most people who receive specialty treatment for an opioid use disorder, however, do not receive these potentially life-saving medications. Lack of insurance coverage is a barrier to receiving treatment for opioid use disorder, particularly given that Medicaid was only recently mandated to pay for all three FDA-approved medications and expanded to reach vulnerable populations. This study sought to find if acquiring insurance coverage or a specific type of insurance was associated with the use of 1) specialty substance use treatment 2) buprenorphine treatment and 3) having a regular source of medical care.
HOW WAS THIS STUDY CONDUCTED?
The authors conducted secondary data analysis of a longitudinal single group multiple cohort study (i.e., where two or more samples are followed prospectively) collected originally from the Baltimore community to compare groups of insured participants to uninsured participants.
- READ MORE ON STUDY METHODS
-
After excluding participants with missing data, the final sample consisted of 1,724 participants who attended at least two study visits during 2006-2017 assessed biannually from 1988-2017 on receipt of specialty substance use treatment, receipt of buprenorphine, and having a usual source of medical care with additional cohorts recruited to replenish the original sample. Since many characteristics could impact service utilization, statistical adjustments were made to equate comparison groups on age, sex, race, having at least a high school education, past six-month injection drug use, heroin use, crack use, unhealthy alcohol use, and HIV status as a way of isolating the effect of having health insurance on service utilization.
The insurance companies confer eligibility on a different basis. VA insurance is only for veterans, Medicare is only for the elderly or qualified disabled. Ryan White is a health insurance payor of last resort (when other insurances do not pay) for individuals with HIV. Medicaid is for low-income individuals. Other insurance is mostly Maryland state-run insurance for the low income.
WHAT DID THIS STUDY FIND?
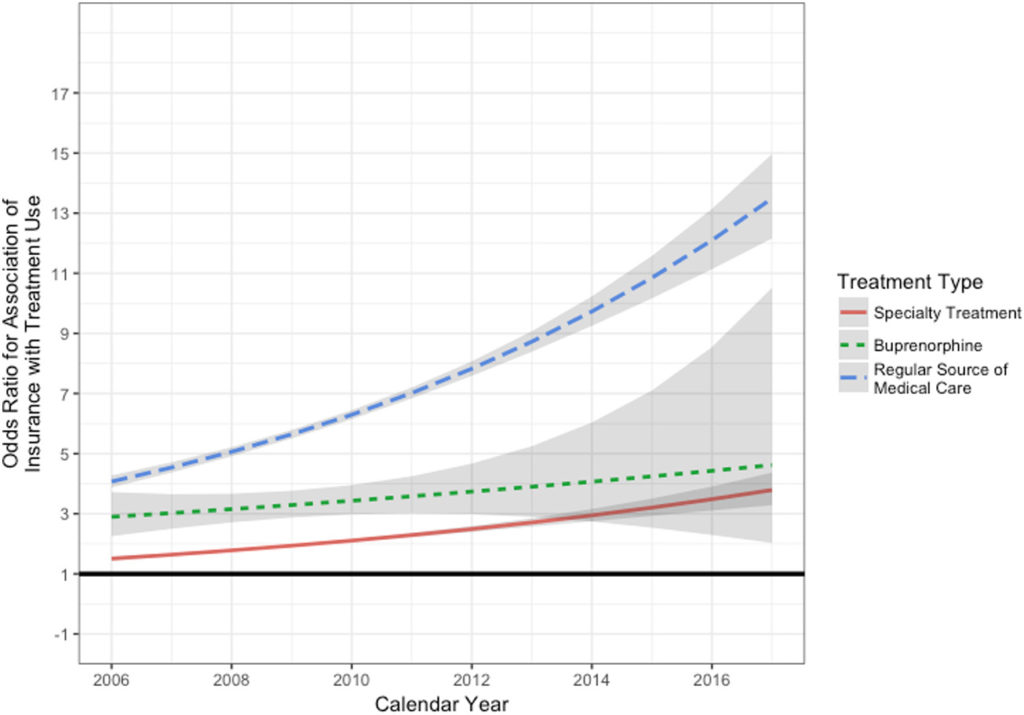
Compared with the uninsured, participants who had health insurance were twice as likely to use specialty substance use treatment, three times as likely to receive buprenorphine and six times as likely to have a regular source of medical care. The associations were observed across each of the insurance types examined (i.e., Medicaid, Private, Medicare, Veterans, Ryan White, other) with the following exceptions:
- Private insurance was not significantly associated with increased use of specialty treatment.
- Veterans (VA) insurance was not significantly associated with increased use of specialty treatment or buprenorphine. Less than 5 percent of the sample had veterans’ insurance.
- Ryan White insurance was not significantly associated with increased use of buprenorphine treatment. Less than 5 percent of the sample had Ryan White insurance.
Overall, Medicaid and Medicare had consistently stronger associations with treatment than private insurance.
When nearly all of the sample was insured by 2017, only about one-seventh of the sample reported receiving buprenorphine in the past six months.
Source: Feder et al., (2019)
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study finds that individuals with injection drug use are more likely to seek specialty substance use treatment, buprenorphine treatment, and secure a steady source of medical care when they have health insurance. This shows that when provided with the right resources, individuals who inject drugs are more likely to seek treatment for their addiction and improve their general health.
This study provides evidence that public health insurance plans like Medicaid play an important role in responding to the opioid epidemic. Parity enforcement will play a critical role in addressing the current opioid epidemic, given that access to public health insurance increases the likelihood of individuals who inject drug to seek treatment. Further, states that have not yet expanded Medicaid to certain groups of low-income adults are likely impeding citizens access to needed care for opioid use disorder.
The finding that individuals with private insurance who inject drugs were no more likely than those without insurance to receive specialty treatment for substance use disorder may be tied to the tendency to impose cost sharing, establish policies like “fail first” (when the patient must fail on a drug or take the cheapest drug before getting what the doctor prescribed) or prior authorizations. Parity enforcement will be key to address those practices. In addition, the positive association between having health insurance and a buprenorphine prescription did not grow over the course of the study, unlike the association between having health insurance and using specialty treatment or seeking regular medical care. The assessment of buprenorphine changed during the study period, which may account for the lack of growth in the association. An alternative explanation may be that insurance is not expanding access to buprenorphine in the Baltimore region.
- LIMITATIONS
-
- Due a design change in the study, researchers could not assess whether methadone was used. However, during the period from 2014 to 2017, past six-month methadone use was reported at between 29 percent and 39 percent of study visits.
- This study could not assess access to other forms of beneficial treatment such as mental health counseling or naltrexone treatment, but insurance coverage may have impacted use of those treatments as well.
BOTTOM LINE
- For individuals & families seeking recovery: This study found that individuals who inject drugs were twice as likely to use specialty substance use treatment, three times as likely to receive buprenorphine, and six times as likely to have a regular source of medical care if they had health insurance. Having health insurance may not make a person get treatment, but having it may remove an important barrier to treatment. Those with health insurance demonstrated an increased likelihood of receiving treatment and increased the duration of treatment available when a person is ready for assistance.
- For scientists: This study found that in 2017, when most of the cohort was insured, only about one-seventh reported receiving buprenorphine in the past six months (although the number of participants injecting opioids was not specified.) This highlights the need to identify other barriers to medication treatment. Barriers may include not perceiving the need for treatment, lack of medication providers or transportation, or the stigma associated with using medication treatment.
- For policy makers: This study suggests that having health insurance, including Medicaid coverage, plays an important role in facilitating access to substance use disorder treatment. Policies and insurance practices that impede access to treatment–such as limiting coverage among certain low-income groups or imposing “fail first” policies (when the patient must fail on a drug or take the cheapest drug before getting what the doctor prescribed) and prior authorizations–may be self-defeating for public health.
- For treatment professionals and treatment systems: This study found that individuals who inject drugs were twice as likely to use specialty substance use treatment, three times as likely to receive buprenorphine, and six times as likely to have a regular source of medical care if they had health insurance. Consider dedicating resources to educating clients about health insurance information and helping them enroll.
CITATIONS
Feder, K.A., Krawczyk, N., Mojtabai, R., Crum, R.M., Kirk, G., & Mehta, S.H. (2019). Health insurance coverage is associated with access to substance use treatment among individuals with injection drug use: Evidence from a 12-year prospective study. Journal of Substance Abuse Treatment, 96, 75-81.

