Benefits of Buprenorphine (Suboxone) Vary by Type of Opioid Addiction
As the use of opioids, including both prescription opioids and heroin, continues to increase in the U.S., so do rates of overdose and healthcare costs attributed to the epidemic.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Buprenorphine is an effective treatment for opioid use disorder, but most research has been conducted in populations of heroin users. While recent research by Weiss et al., 2015 showed improvement for prescription drug users on buprenorphine at 42 months, the knowledge base remains limited on outcomes specifically for this group.
Additionally, there is a lack of research comparing treatment outcomes among three distinct groups of opioid users: those who exclusively use prescription opioids, those who exclusively use heroin, and those who use both.
HOW WAS THIS STUDY CONDUCTED?
This study is based on data from 179 participants enrolled in a clinical trial of heroin and prescription opioid users receiving buprenorphine and medical management (MM) and one of four behavioral interventions: cognitive behavioral therapy (CBT), contingency management (CM), both CBT and CM, and MM alone. Participants started taking buprenorphine and adjusting their dose to a stable level over the course of two weeks. They then received combined behavioral treatment and buprenorphine for 16 weeks, followed by another 16 weeks of buprenorphine-only treatment. Participants were tapered off the medication between weeks 34 and 40.

Individuals aged 15 or older meeting DSM-IV criteria for opioid dependence without a comorbid psychiatric condition were eligible for the study. Since there was no difference between behavioral treatment conditions in the main trial, these groups were collapsed and participants were classified by opioid use status based on the 30 days before entering the study: prescription opioid only (PO; n = 54), prescription opioid and heroin (POH; n = 71), and heroin only (H; n = 54).
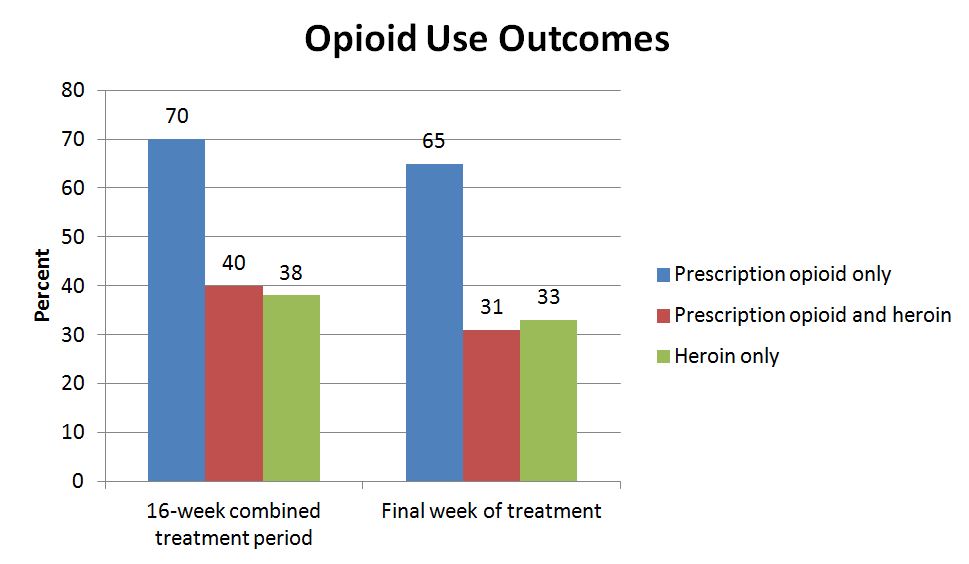
he primary outcomes were use of opioids other than the prescribed buprenorphine over the combined treatment phase and during the final week of this phase (as determined by urine drug screen) and treatment retention (i.e., remaining on medication) at the end of the combined treatment phase.
WHAT DID THIS STUDY FIND?
PO participants were more likely to be White or Hispanic and regularly employed than POH and H, while H participants had the longest average history of opioid use (21 years vs. 16 for both PO and POH). The main outcome of opioid use was determined by Treatment Effectiveness Score (TES) calculated as number of opioid negative urine drug screens over the number of possible drug screens.
The PO group had significantly better outcomes as measured by more opioid negative drug screens than the other two groups over the combined treatment period and during the final week of treatment. The differences in percentages remained significant after controlling for differences in baseline characteristics including race, marital status, employment status, and length of opioid use.
In the final week of treatment, after controlling for these factors, PO participants were over 5 times more likely to have two opioid negative urine drug screens than both POH and H. PO participants also provided significantly more opioid negative drug screens than POH and H at the end of the buprenorphine-only phase (week 34) and at the end of the taper phase (week 40), though these differences were no longer significant by the final assessment (week 52).
At the end of the combined treatment phase, participants had positive urine drug screens for other substances including benzodiazepines, cocaine, amphetamines, and marijuana though cocaine was the only substance for which there were significant differences in use with 29% of H participants screening positive compared to 12% of POH and 6% of PO.
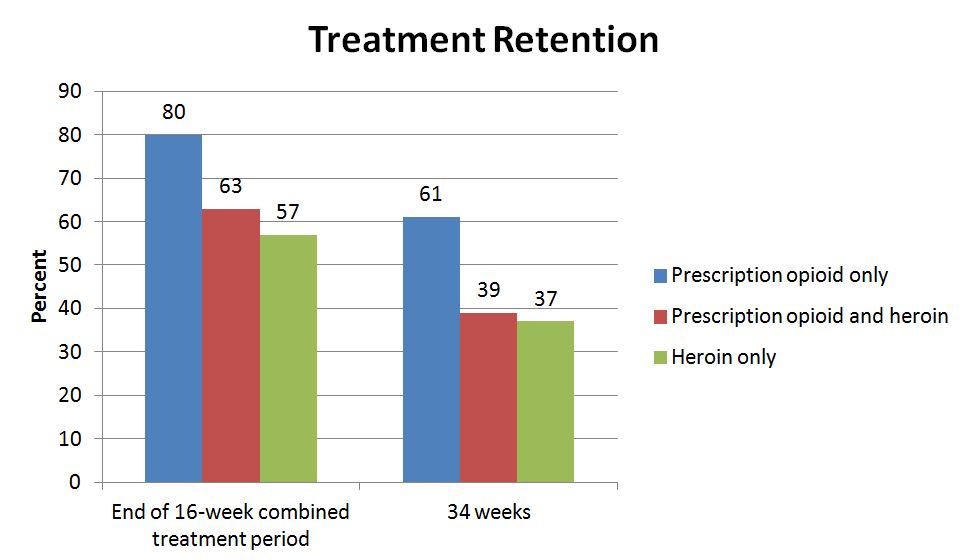
Treatment retention was significantly different by group with highest rates in the PO group. In a controlled model, those in the PO group were over 2.5 times more likely to be retained in treatment than those in the H group. At week 34, the PO group continued to have higher rates of retention.
In this study, prescription opioid users had better outcomes compared to participants who used heroin in combination with prescription opioids or alone. The differences between these groups in characteristics such as history of use, marital status, and employment status suggest that prescription opioid users may have more sources of social support. Having a spouse for emotional support or a job with reliable income are examples of recovery capital, or resources that are necessary to begin and maintain recovery.
Overall, the prescription opioid users in this study may have had more recovery supportive environments than participants who used heroin, which may partially account for their improved results. Heroin users may also be more entrenched in their addiction pattern as they their history of use was longer on average, making it more difficult to stop use. Other interventions and recovery support services need to be explored to ensure that heroin users can experience similar levels of success.
WHY IS THIS STUDY IMPORTANT
Prior research has shown that prescription opioid users may differ from heroin users in several ways that could have implications for treatment. For example, prescription opioid users tend to have shorter histories of use and fewer prior treatment episodes than heroin users. Studies also suggest that prescription opioid use may lead to heroin use and possibly injection drug use, so treating people who use prescription opioids earlier may prevent this progression.
With a majority of buprenorphine treatment research focusing on heroin users, this study adds to the evidence regarding its effectiveness for other opioid using populations.
Since a majority of prior research on the effectiveness of buprenorphine was conducted in heroin-using populations, this study provides support for its use among people who solely use prescription opioids.
It is possible that treating prescription opioid users with buprenorphine may help them cease opioid misuse before progressing to the use of heroin which has been shown to result in a worse prognosis.
Also, given that heroin users had worse outcomes, which may be due to their lower recovery capital and more severe clinical presentation, individualized treatment plans addressing stressful life circumstances may improve outcomes for these individuals.
Alternatively, they may require different dosing of buprenorphine or a full agonist such as methadone.
- LIMITATIONS
-
- This study was a secondary analysis using data from a randomized controlled trial not originally designed to compare the types of opioids used by individuals in treatment. The urine drug screen used in assessing the main outcome may not have been sensitive enough to pick up on a full range of prescription opioids such as fentanyl.
NEXT STEPS
More research is needed to understand why prescription opioid users appear to fare better in treatment than heroin users by testing the hypothesis raised by this study that POs’ greater recovery capital is accounting for their better outcomes. Interventions and support services addressing the needs of subgroups of opioid users should also be explored.
BOTTOM LINE
- For individuals & families seeking recovery: With prescription opioids, consider treatment with buprenorphine in combination with a behavioral therapy to improve your chances of recovery. If using heroin, more support may be needed, such as another type of medication (e.g., methadone) and more behavioral treatment and recovery support services. While this study found that participants who used heroin did not do as well, there are many pathways to recovery that can be used alone or in conjunction with buprenorphine.
- For scientists: This study showed differences in outcomes by type of opioid used. Research is needed to determine the cause of these differences and identify strategies to improve outcomes for subgroups of opioid users who do not respond as well to treatment.
- For policy makers: Buprenorphine works similarly, if not better, for patients who solely misuse prescription opioids before entering treatment. In light of the prescription opioid epidemic in the U.S., it is important that this is a widely available treatment option for those who may benefit from its use. It is also important that recovery support services, including ones that can assist with obtaining employment and housing, are available for people who may be lacking in social supports.
- For treatment professionals and treatment systems: Based on a patient’s individual situation and needs, it may be beneficial to prescribe buprenorphine regardless of the type of opioid used.
CITATIONS
Nielsen, S., Hillhouse, M., Mooney, L., Ang, A., & Ling, W. (2015). Buprenorphine pharmacotherapy and behavioral treatment: comparison of outcomes among prescription opioid users, heroin users and combination users. J Subst Abuse Treat, 48(1), 70-76. doi:10.1016/j.jsat.2014.06.00

