Buprenorphine Treatment Dissemination Disparities Persist
In New York City, access to buprenorphine and methadone were previously found to be disproportionally distributed based on income and race-ethnicity. This study took an updated look to determine if this trend persisted over time from 2004-2013 and identify who may have restricted access to this evidence based treatment.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
In the U.S. there was sharp rise in the non-medical use of prescription opioids and heroin over the past decade. Buprenorphine is a partial opioid agonist that emerged as an office-based treatment that has comparable effectiveness to methadone in treating opioid use disorder. A previous study in New York City found that buprenorphine patients were significantly more likely to live in high income, predominantly White areas, however, methadone patients were more likely to live in low-income, predominantly Black or Hispanic areas. Buprenorphine has been shown to improve treatment retention and health outcomes among low-income, socially marginalized populations and differential access to buprenorphine may fail to protect the health of these populations. This study investigated whether these treatment patterns persist over time. The hypotheses tested were: 1) usage of methadone has declined and usage of buprenorphine has increased 2) the variation among neighborhoods defined by income, race-ethnicity in buprenorphine and methadone usage persists over time.
HOW WAS THIS STUDY CONDUCTED?
The buprenorphine treatment rate from 2004 to 2013 was supplied by the New York State Bureau of Narcotics Enforcement by residential postal ZIP code of the patient. Methadone maintenance treatment rates were based on data from the New York State Office of Alcoholism and Substance Abuse Services that accounted for all patients receiving methadone maintenance treatment in New York City clinics in 2004–2013 by patients’ ZIP code. Social area analysis of residential zip codes of methadone and buprenorphine patients in New York City, which aggregated zip codes into five social areas with similar percentages of residents below poverty, and identifying as Black non-Hispanic and as Hispanic, were used examine whether treatment rates differed significantly among areas over time. Usage rates of buprenorphine and of methadone were the dependent variables.
WHAT DID THIS STUDY FIND?
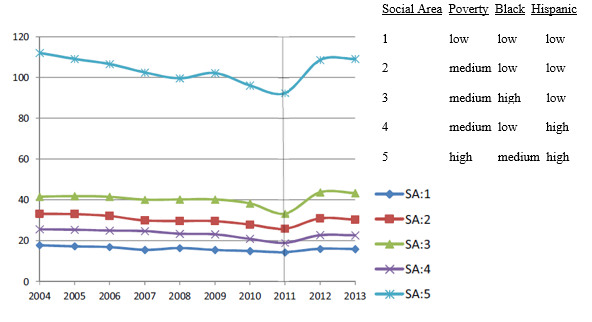
The first hypothesis was partially supported when the results showed that overall usage of methadone maintenance treatment in New York City decreased until 2011 and increased there-after returning to 2004 levels of usage. In addition, overall buprenorphine maintenance treatment rates increased over time.
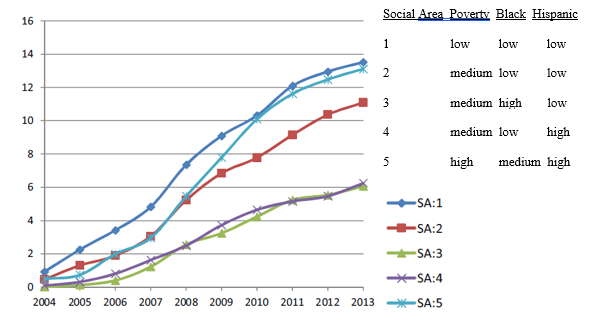
The second hypothesis was partially supported by data that showed variation in usage among neighborhoods defined by income and race-ethnicity. Specifically, buprenorphine maintenance treatment had the slowest rates of growth in two social areas (3 and 4 on Figure 1) with moderate incomes and predominantly black and predominately Hispanic residents. Rapid increases in buprenorphine maintenance treatment were found in areas with relatively low poverty and low proportions of Black and Hispanics (areas 1 and 2) as well one area that had higher poverty and proportions of Black and Hispanic residents (area 5). Although methadone maintenance treatment decreased for all areas from 2004 to 2011, the area with the greatest decrease was composed of high poverty and predominantly Black and Hispanic residents (area 5 in Figure 2). From 2011-2013 significant increases in methadone maintenance treatment were seen in areas with moderate incomes and predominantly Black and Hispanic residents (areas 2 and 3) with the biggest increase in an area (5) with high poverty and many black and Hispanic residents.
Means of Buprenorphine Maintenance Treatment Rates Over Years for Each Social Area in New York City
Means of Methadone Maintenance Treatment Rates Over Years for Each Social Area in New York City
WHY IS THIS STUDY IMPORTANT?
This study is important because unequal access to life saving medications can cause health disparities in remission and recovery from opioid use disorder. Methadone maintenance treatment rates were mostly sustained over time which may reflect that methadone is still a widely used treatment. A decade after the introduction of buprenorphine treatment access is still unevenly distributed across residential areas of New York City.
Two of the three social areas (2 and 3) with the fastest rate of increase in buprenorphine treatment were the highest income areas with the highest percentage of White residents. The rapid increase in buprenorphine treatment in predominantly White well-off areas (1 and 2) could reflect the uptake by private physicians or that the opioid crisis has affected more Whites than non-Whites.The increase in buprenorphine treatment in the high poverty area (5) might reflect the adoption of buprenorphine by public health clinicians and programs.
Authors suggest the exception in area 5 may be explained by the efforts of South Bronx addiction treatment advocates, to integrate buprenorphine into both primary care and outpatient clinics that served primarily low-income and Medicaid insured patients.
- LIMITATIONS
-
- It is unknown if observed patterns in the data are due to lower levels of physician uptake of these treatments, to lower levels of health insurance coverage, or to other variables disproportionately affecting certain areas of New York City.
- This study was based off the most densely populated city in the country so it is unknown the degree to which the results generalize to smaller or more rural cities.
NEXT STEPS
Future research should identify the reasons for slower adoption of buprenorphine in neighborhoods that are characterized by poverty and racial-ethnic minorities, including the rates of opioid misuse/opioid use disorder, availability of prescribers, and the quality of buprenorphine treatment as opposed to methadone treatment in those neighborhoods.
BOTTOM LINE
- For individuals & families seeking recovery: This study found that neighborhood poverty and racial-ethnic composition remain correlated with buprenorphine and methadone usage over time, and there are geographic differences in buprenorphine maintenance treatment compared to methadone maintenance treatment. These medications used to treat opioid use disorder reduce mortality rates, withdrawal symptoms, and increase the likelihood of remission and recovery. Be persistent in learning about all your treatment options for you or someone you know who may be dealing with an opioid use disorder.
- For scientists: Additional research should identify factors associated with the adoption of buprenorphine in neighborhoods with predominantly ethnic minority residents and poverty, including rates of opioid misuse/use disorder, the availability of physicians who prescribe, and health insurance coverage. More work is also needed to understand what distinguishes patients being treated with buprenorphine maintenance treatment who would not otherwise seek treatment with methadone.
- For policy makers: This study found geographic disparities in buprenorphine treatment usage compared to methadone maintenance treatment persist over time and these differences are related to neighborhood poverty and racial-ethnic minority composition. Assuming equal levels of misuse/use disorder, consider prioritizing policy and intervention practices that promote equity in the distribution of maintenance treatments for opioid use disorder to eliminate health disparities in remission and recovery.
- For treatment professionals and treatment systems: In New York City, methadone maintenance treatment rates have remained stable over time and buprenorphine maintenance treatment rates increased in all areas with slower uptake in moderate income mixed ethnicity areas. Consider what practices your treatment system can implement to help ensure an equitable distribution of access to evidence based treatments such as obtaining physician waivers to prescribe buprenorphine.
CITATIONS
Hansen, H., Siegel, C., Wanderling, J., DiRocco, D. (2016). Buprenorphine and methadone treatment for opioid dependence by income, ethnicity, and race of neighborhoods in New York City. Drug and Alcohol Dependence, 164, 14-21.

