Life after detox: Can medication and residential treatment for opioid use disorder reduce risk of death?
Relatively few individuals who complete medically supervised detoxification programs for opioid withdrawal go on to receive further treatment. This study highlights the risks of attending only detoxification, and showed that post-detox engagement in treatment, particularly medication treatment for opioid use disorder, can reduce the risk of mortality (e.g., opioid overdose) in the 12 months after detoxification.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Detoxification programs for opioid use disorder, also known as medically managed opioid withdrawal, are in-patient short-term programs that help individuals overcome severe withdrawal symptoms using opioid agonists like methadone/buprenorphine or non-opioid alternatives like clonidine and anti-inflammatories. These agonists or non-opioid alternatives are typically tapered down over the course of about five to ten days. Detoxification alone, however, is almost never sufficient for opioid use disorder patients, as many individuals return to opioid use after completing such programs. While relapse and recurrence of symptoms may be a common part of the recovery process, returning to opioid use after a period of sustained abstinence can increase one’s risk for overdose. This is because the acquired tolerance to an opioid’s effects is lost during a long period of abstinence as the brain readapts to opioid abstinence. Returning to opioid use in amounts similar to those used before detoxification can result in overdose due to this loss of tolerance. Medications for opioid use disorder (e.g., methadone and buprenorphine) are shown to reduce opioid overdose risk and utilization of residential treatment programs is associated with reduced mental and physical health harms (e.g., emergency department visits, return to detoxification, etc.). Despite the benefits of psychosocial and medication treatments for opioid use disorder, only about 13% to 36% of patients go on to receive treatment after detoxification. To better understand the effects of follow-up care, the current study evaluated treatment (medication and/or residential) receipt post detoxification and its relationship to opioid-related and general (i.e., all-cause) mortality.
HOW WAS THIS STUDY CONDUCTED?
The authors conducted a retrospective cohort study using a subset of data from the Massachusetts Public Health Data Warehouse (i.e., Bureau of Substance Addiction Services (BSAS) dataset), which is overseen by the Department of Public Health and includes Massachusetts residents aged 11 years and older who had health insurance (public or private) between the years 2011 and 2015, ultimately representing 98% of the state’s residents. Individuals in this dataset were included in the study if they were aged 18+, identified opioids as their primary substance, and had an opioid-related detoxification (i.e., medically managed withdrawal) episode between January of 2012 and December of 2014, allowing the researchers to examine the 12-month period before and after detoxification. Individuals without documented birthdate or sex, and those diagnosed with cancer were excluded from analysis.
Follow-up for each detox episode began during the month of detox and ended at the date of (1) a recurrent detoxification episode or (2) death. If neither of those events occurred, the follow-up ended at (3) 12 months after detox. Up to five detoxification episodes were considered per patient and those beyond their 5th detox episode were excluded from analysis. The authors evaluated four post-detoxification situations in each month after detox: (1) no treatment, (2) ≥ one month of medication treatment for opioid use disorder (buprenorphine / methadone / naltrexone) without residential treatment, (3) ≥ one month of residential treatment without medication treatment, and (4) ≥ one month of concurrent medication treatment and residential treatment. If treatment was received for at least one day in a given month, that month was counted as a treatment episode.
Figure 1.
Outcomes of interest included all-cause mortality (i.e., died for any reason; not due to any specific disease or disorder) and opioid-related mortality (i.e., opioids contributed to death, such as opioid-related overdose death), as determined by medical examiner or the department of public health. Mortality was evaluated across the full 12 months after detoxification to determine overall mortality risk relative to no treatment both 1) while receiving treatment, and 2) in the month following discontinuation of treatment (i.e., stopped or completed treatment), because this is a documented period of heightened overdose risk. When conducting their analyses, the authors statistically controlled for a number of potentially influential factors, including age, sex, diagnosis of anxiety/depression, race/ethnicity, receipt of monthly prescriptions for opioids or benzodiazepines (pre and post detox), non-fatal overdose episodes, recent incarceration, homelessness, and medication/residential treatment receipt within the 12 months prior to detox. The final dataset included 61,819 detoxification episodes among 30,681 individuals. The sample primarily consisted of white (81%) men (68%), younger than 45 years of age (86%). In the 12 months prior to detoxification, 16% had at least one medication treatment episode, 5.3% had a residential treatment episode, and only about 1% of individuals had both a medication and a residential treatment episode.
WHAT DID THIS STUDY FIND?
Within the 12 months following discharge from detoxification:
- 41% of detoxification episodes were followed by an episode of medication treatment (median duration = 3 months)
- 35% were followed by a residential treatment episode (median duration = 2 months)
- 13% were followed by an episode of combined medication and residential treatment (median duration = 5 months)
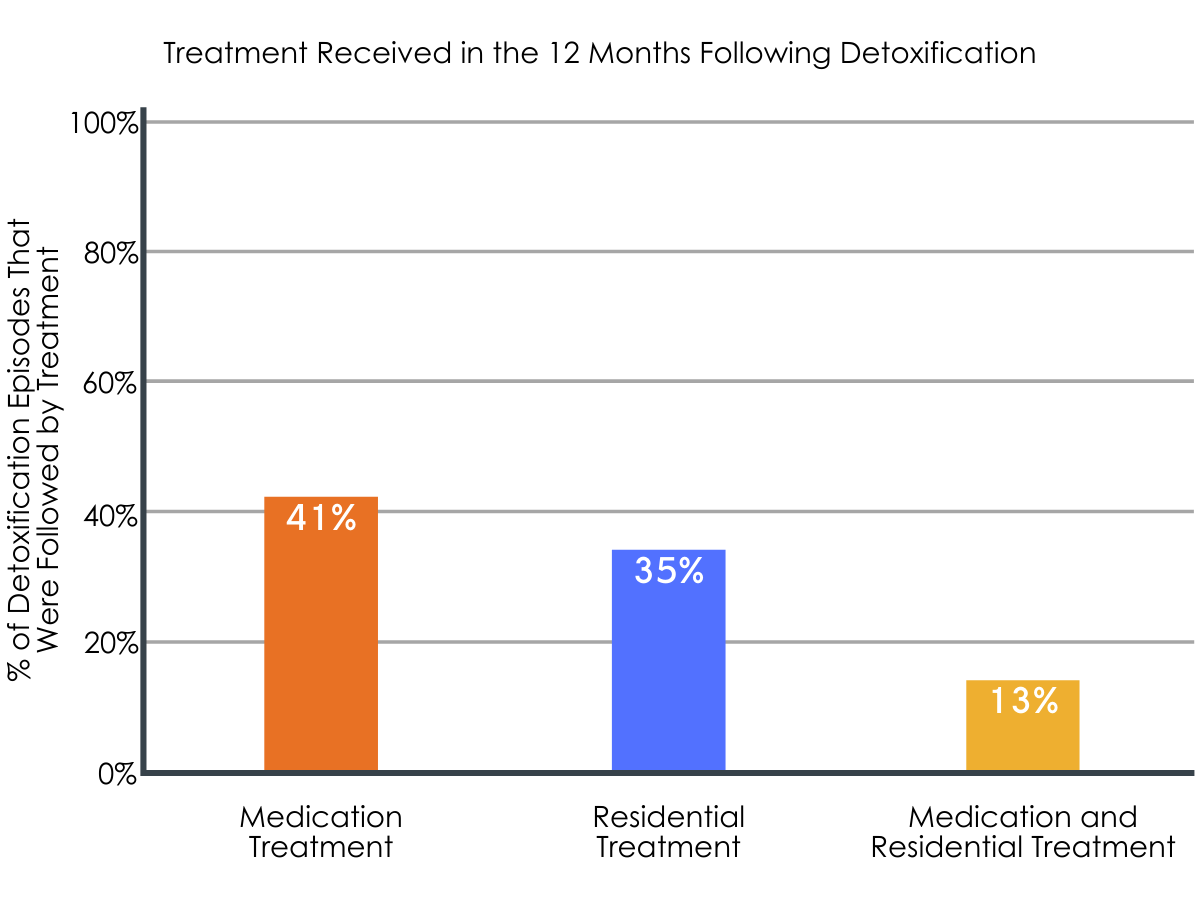
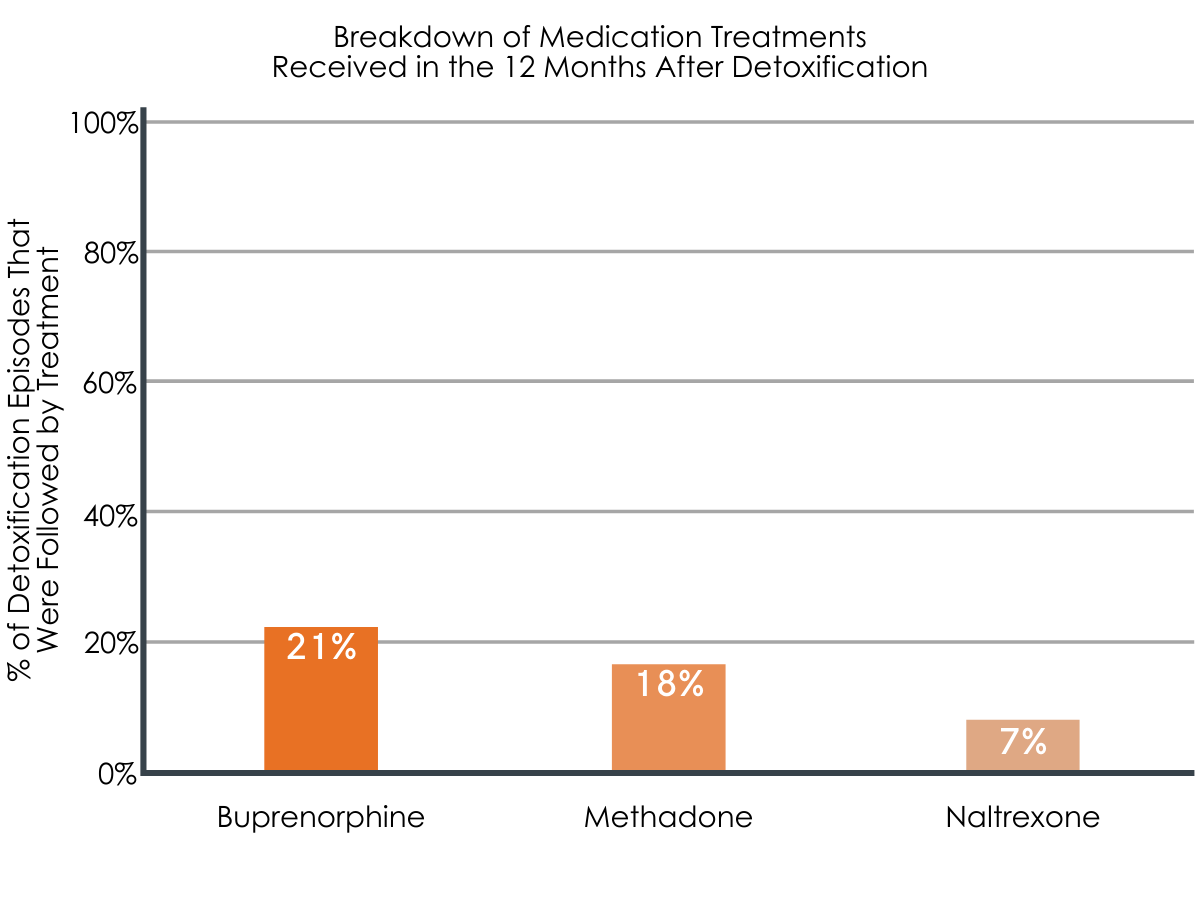
Figures 2 and 3. The images above show the percentage of detoxification episodes that were followed by receipt of various treatment types. Percentages shown for specific medication treatments sum to greater than 41% because individuals could have had multiple detoxification episodes and, thus, multiple post-detoxification treatments, including more than one type of medication treatment.
Risk of all-cause mortality and opioid-related mortality were reduced in individuals who received treatment.
Mortality risk was reduced in individuals who received medication treatment (0.81 all-cause deaths & 0.52 opioid-related deaths per 100 person years), residential treatment (1.27 all-cause & 1.06 opioid-related deaths per 100 person years), or a combination of the two (fewer than 1.23 all-cause and opioid-related deaths per 100 person years), relative to those who did not receive treatment (2.04 all-cause deaths & 1.42 opioid-related deaths per 100 person years) within the 12 months following detoxification. Although the authors did not explicitly test for differences between treatment types, descriptively, the risk of mortality decreased the greatest with combined medication and residential treatment, followed by medication treatment alone, and residential treatment alone, when compared to no treatment.
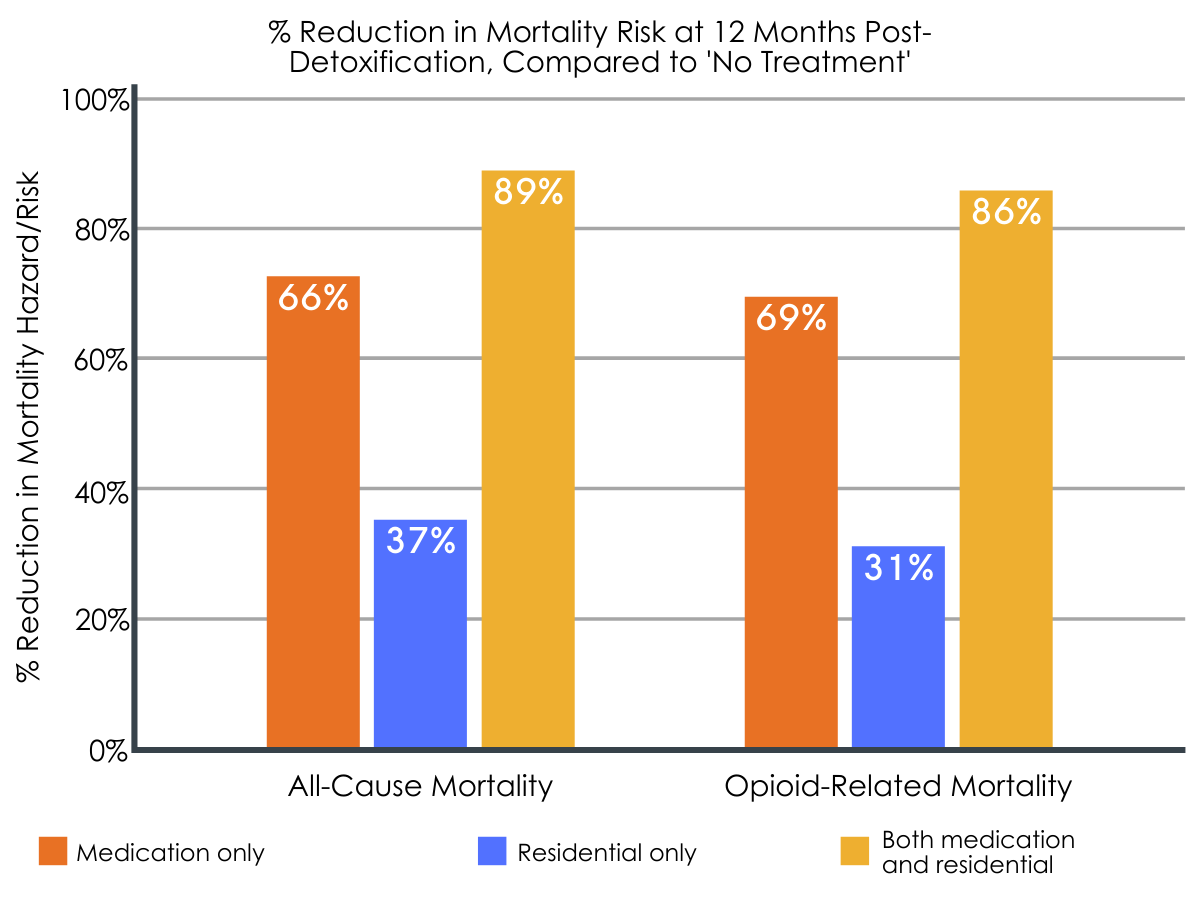
Figure 4. This figure shows the degree to which each treatment type reduced mortality risk in the 12 months following detoxification, compared to no treatment. Higher rates reflect larger reductions in mortality risk (i.e., lower risk of death).
Treatment was also associated with reduced risk of all-cause mortality and/or opioid-related mortality in the month immediately after discontinuing/stopping treatment, with medication treatment being generally superior.
All-cause mortality in the first month following discontinuation was significantly lower among all three treatment groups (number of all-cause deaths per 100 person years: 1.17, 1.49, and < 1.13 for medication, residential, and combined treatment, respectively), compared to the no treatment group (1.94 all-cause deaths per 100 person years). Regarding opioid-related mortality, however, only medication treatment (alone or in combination with residential treatment) was significantly associated with reduced risk of death compared to no treatment (number of opioid-related deaths per 100 person years: 0.75, 1.26, and ≤ 1.23 for medication, residential, and combined treatment, respectively, vs. no treatment: 1.35 deaths per 100 person years).
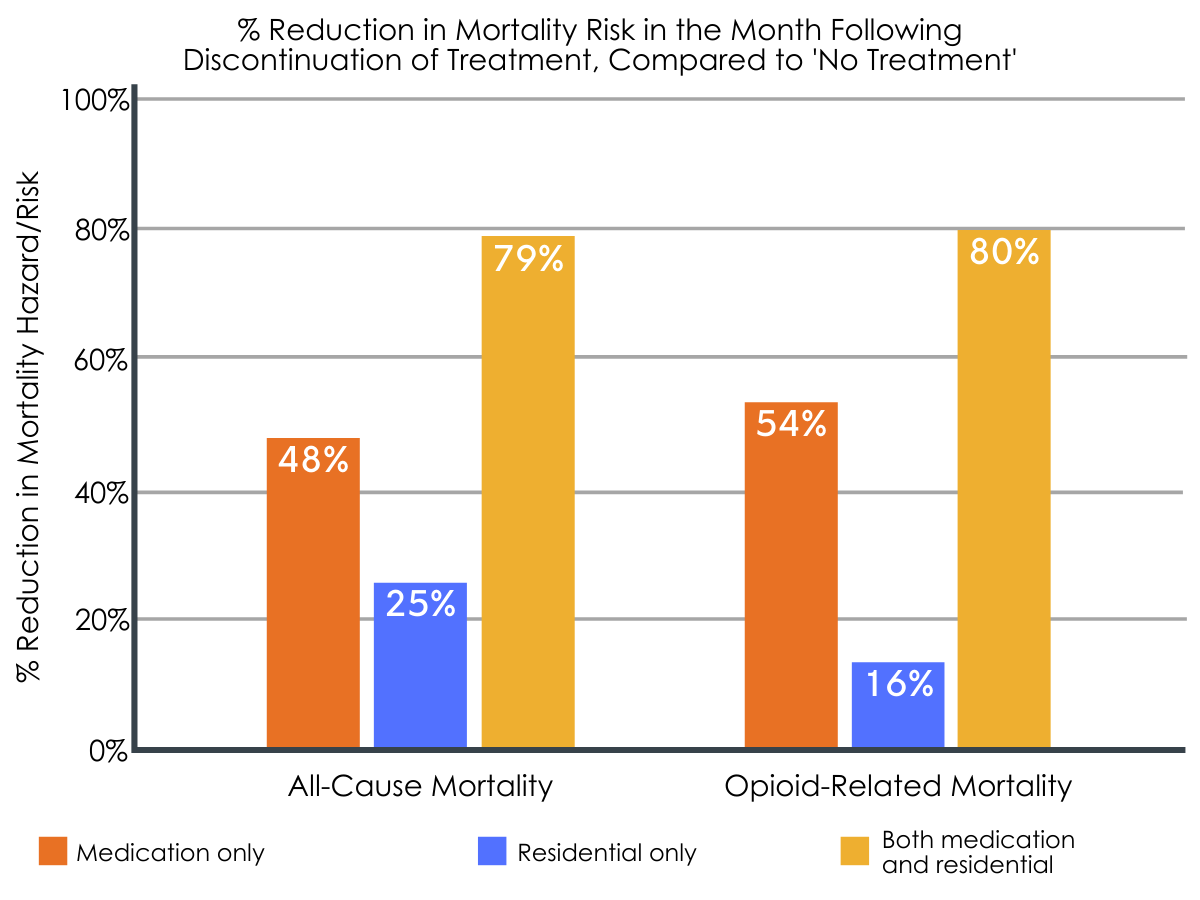
Figure 5.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Studies like this highlight the importance of receiving continued care after detoxification to reduce mortality and overdose. In line with previous work, the authors found high rates of mortality (1.5-2 deaths per 100 person years) among those who did not receive treatment post detoxification. However, their findings suggest that engagement in medication and/or residential treatment after detoxification can decrease risk of all-cause (i.e., not related to disorder or disease) deaths and opioid-related overdose deaths. More specifically, medications for opioid use disorder appear to be the best therapeutic option for reducing risk, which is consistent with other studies highlighting the benefits of medication treatment, particularly agonists like buprenorphine and methadone, even when compared to other treatment options like intensive behavioral or intensive outpatient treatments.
This study also suggests that residential treatment can benefit individuals, particularly when it is accompanied by medication treatment – receiving a combination of the two treatments resulted in the highest reduction in mortality risk when compared to no treatment. That said, this reduced risk via residential treatment alone is important because 20-40% of those with opioid use disorder who receive detoxification services decline the recommendation for medication. Given the relatively small number of individuals who received both treatments during the course of the study (translating to a limited number of deaths in analyses), randomized controlled studies are needed to determine whether combining residential and medication treatment has an additive protective effect, and if certain aspects of residential treatment – such as linkages to community-based mutual-help groups – might underlie these potential benefits.
Nevertheless, medication treatment with or without residential treatment was associated with the most substantial decline in mortality risk, emphasizing the importance of medication treatment for supporting the benefits of short-term detoxification. Interestingly, a relatively high number of individuals in this study received medication treatment after detoxification (~41%), with other studies reporting that only about 13% to 36% of patients go on to receive continued care after detoxification. Prevalence rates in the current study may reflect Massachusetts state’s more progressive/universal health care system and emphasis on addressing addiction. An investigation of medication treatment receipt within the Veterans Administration similarly revealed a prevalence estimate of 41%, further suggesting the potential role of healthcare system models in medication access and receipt. Furthermore, Massachusetts has more mental health care providers per person than any other state, which could ultimately translate to more thorough referral to continuing care once someone has already had a treatment-system encounter (i.e., engagement in a detoxification program).
Out of all the medication treatment services provided, methadone resulted in the longest treatment duration (~5 months), followed by buprenorphine (~3 months), and naltrexone (~1 month). Treatment duration is an important factor in recovery and mortality – when examining agonist medications, only those who remain on medications for an extended period of time (e.g., 6 months) appear to reliably experience reduced risk. Given that the average treatment duration for all treatment modalities was fewer than six months in the current study, more efforts are needed to understand the reasons for the low rates of clinically-recommended prolonged engagement in treatment. Importantly, risk of opioid-related overdose death was not reduced in the month after discontinuing residential treatment (without medication). Therefore, individuals seeking medication-free treatment options should be aware of the potential increased risk for opioid overdose and death without medication treatment, and the importance of overdose reversal medications (Narcan) in the instance of relapse and overdose.
Although opioid overdose rates generally declined in the past couple of years, rates of overdose due to synthetic opioids other than methadone, like fentanyl, have continued to rise. With so few individuals receiving care after detoxification, active linkage to treatment services after an acute care episode may be needed to address the ongoing opioid overdose crisis. However, when active linkages are made some patients are nevertheless reluctant to engage with further medication or other treatment, and studies have yet to fully characterize the reasons for this. Therefore, it is unclear whether low rates of post-detoxification care are due to a lack of clinician referral and linkage of patients to continued care, or if patients lack the desire for treatment after detox, and additional research is needed.
- LIMITATIONS
-
- This research was based on a dataset of Massachusetts residents and may not generalize to other geographic regions, as overdose and mortality may also be affected by healthcare systems, harm reduction programs, and treatment/recovery support resources offered in the region of interest. The authors did not distinguish between different formulations of medication treatment (e.g., injectable vs. oral naltrexone), which is shown to influence treatment retention/outcomes, warranting further investigation.
- The authors excluded individuals with more than five detoxifications within the time frame assessed and did not examine opioid use disorder diagnosis or control for opioid use disorder severity. Therefore, findings may not apply to all individuals with opioid use disorder. The analyses were based on a cumulative state healthcare dataset, heightening risk for misreported or undocumented treatment episodes. Furthermore, use of any treatment modality within a given month was categorized as treatment received, regardless of treatment duration. Thus, individuals with a single day of treatment may be included as treatment receivers in those analyses, which could mask the full magnitude of the treatment effect on mortality risk.
- Any given participant could have used multiple different treatment modalities across the 12-month period; thus, treatment categories were not exclusive. Moreover, discontinuation was defined as the end of a treatment episode regardless of whether or not that treatment was completed or not. Additional research is needed to determine the influence of transition to other treatment modalities on mortality and to examine the nuances of discontinuation is it pertains to treatment completion. Patients also self-selected their post-detoxification plans, which could lead to inherent individual differences not accounted for in this study and randomized controlled trials are needed to directly compare the effectiveness of these treatment modalities.
BOTTOM LINE
- For individuals and families seeking recovery: Relatively few individuals go on to receive treatment after completing opioid-related detoxification. Detoxification leads to a loss of opioid tolerance and, should relapse occur, individuals are at increased risk for overdose. The current study assessed the relationship between post-detox care and mortality, highlighting the importance of receiving continued care after detoxification to reduce mortality and opioid-related overdose. More specifically, utilization of medication treatment and/or residential treatment was associated with reduced risk of death when compared to no treatment post detox. Although completion of residential treatment alone somewhat reduced mortality risk, medications for opioid use disorder (e.g., methadone, buprenorphine), either alone or in combination with residential treatment, appear to be associated with the greatest reduction in risk. Therefore, receiving treatment, particularly medication treatment services, after detoxification appears to be an important step in the treatment process and a key component to help protect individuals from an opioid-related death. Individuals interested in post-detoxification treatments are encouraged to contact their health care and insurance providers to inquire about the right option for them.
- For treatment professionals and treatment systems: While relapse is a common part of the recovery process, returning to opioid use after a period of sustained abstinence can increase one’s risk for overdose. Medically managed opioid withdrawal (detoxification) is one such instance in which tolerance is reduced, and with so many individuals failing to receive subsequent treatment, overdose is a major concern. The current study highlights the importance of receiving continued care post detoxification to reduce mortality and overdose. Although both medication and residential treatment reduced mortality risk, medication treatment was associated with the greatest reduction, regardless of treatment retention/discontinuation or administration with/without residential treatment. Residential treatment alone showed somewhat reduced risk of opioid-related mortality compared to no treatment, but this benefit was not observed in the month immediately following treatment discontinuation. Therefore, receipt of post-detoxification treatment, particularly medication treatment services, appear to be an essential component to reduce patient risk of all-cause and opioid mortality. Detoxification presents an ideal opportunity for intervention and active linkage to continued care. Additional research looking at the real-world effects of active linkage to treatment after detoxification and reasons underlying treatment refusal with and without linkage to further care are needed to help identify best practices for boosting patient outcomes and reducing risk of death.
- For scientists: This retrospective cohort study examined the relationship between treatment receipt post detoxification (medically managed opioid withdrawal) and mortality risk. The authors found that receipt of medication and/or residential treatment after acute detoxification was associated with reduced risk of all-cause and opioid-related mortality in the 12-months following detoxification, relative to no treatment; the magnitude of risk reduction appeared to be greatest for combined medication plus residential treatment, followed by medication treatment alone, and residential treatment alone. However, additional research is needed to directly compare these treatment modalities, as they were not statistically compared in this study. When the authors assessed mortality risk in the month following treatment discontinuation, residential treatment (alone) was no longer associated with reduced risk, emphasizing the importance of medication treatment in the context of opioid-related mortality. Given the relatively small number of individuals who received both residential and medication treatments during the course of the study, randomized controlled investigations are needed to determine if combined treatment produces an additive effect and to understand more about which individuals in particular may be more likely benefit from the combination of residential and medications. Research is also needed to disentangle these outcomes as they pertain to specific pharmacotherapy compounds, psychosocial treatment aspects underlying these effects, and applicability across other states and healthcare systems.
- For policy makers: Medically managed opioid withdrawal (detoxification) programs are in-patient short-term programs that help individuals overcome the most severe aspects of their physical dependence on opioids. Many individuals fail to receive treatment after detoxification, and this is particularly concerning because opioid tolerance diminishes during detoxification, increasing one’s risk of overdose should individuals relapse. While relapse is a common part of the recovery process, this study suggests that receiving treatment following detoxification, particularly medication treatment (e.g., methadone, buprenorphine), can reduce risk of all-cause and opioid-related mortality. To the extent that the lack of medication or residential treatment use is due to lack of assertive clinical linkage following receipt of detox services, findings could suggest that linking individuals to continued care post detoxification could further reduce deaths in the year following opioid detoxification. Additional funding for research will help determine the comparative effectiveness of these various treatments, the specificity of these outcomes to different medication compounds, and the psychosocial treatment aspects underlying these effects. Moving forward, it will be particularly important to examine whether or not these outcomes hold true in states with different healthcare systems, including those with less universal health insurance and access to care than Massachusetts.
CITATIONS
Walley, A. Y., Lodi, S., Li, Y., Bernson, D., Babakhanlou‐Chase, H., Land, T., & Larochelle, M. R. (2020). Association between mortality rates and medication and residential treatment after in‐patient medically managed opioid withdrawal: A cohort analysis. Addiction, 115(8), 1496-1508. doi: 10.1111/add.14964

