From “intensive” to “extensive” interventions: Can a brief telephone monitoring intervention improve outcomes after inpatient detoxification?
It is common for some to complete multiple inpatient detoxification admissions before experiencing a sustained period of remission from alcohol or other drug use disorders. One reason may be that many people have difficulty attending ongoing services via outpatient treatment and/or mutual help after detoxification. The authors of this study showed that, relative to usual care, a 3-month telephone monitoring intervention reduced detoxification readmissions and improved substance use outcomes following discharge from inpatient detoxification, but that advantage disappeared after the 3-month intervention ended.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Stable recovery from substance use disorder (SUD) can take several years and multiple treatment episodes to initiate, particularly for those with more severe substance use profiles. For many, treatment for alcohol and opioid use disorders begins with inpatient detoxification to manage withdrawal symptoms and avoid potential medical complications. It is not uncommon to attend detoxification treatment multiple times on the path to recovery. For example, in 2017, nearly 70% of people who were admitted to inpatient detoxification in the U.S. reported at least one previous admission. About half of individuals who attend detoxification will not access any form of support after discharge, and while some programs offer enhanced treatment, detoxification is largely focused on basic medical stabilization.
While there are a multitude of reasons why an individual may not engage with recovery-supportive services after detoxification, including limited professional resources to help with active linkages, research shows that attending formal treatment, mutual-help groups, or some combination of these after detoxification decreases the chance of returning to substance use and additional inpatient admissions.
Building on previous research showing that a brief telephone monitoring intervention helped patients remain in SUD treatment, the authors of this study sought to test the effectiveness of such monitoring on readmission and other outcomes following a detoxification admission. The intervention emphasized a motivational interviewing approach, which is collaborative in nature and seeks to help people build intrinsic motivation for recovery-oriented behavior and activities.
HOW WAS THIS STUDY CONDUCTED?
This was a randomized clinical trial with 298 participants recruited from two Veteran’s Affairs inpatient detoxification treatment facilities. Participants were randomly assigned to receive either the telephone monitoring intervention (referred to here as “monitoring” or “intervention”) or detoxification as usual (referred to here as “usual care” or “control”), and were assessed for detoxification readmissions, substance use, and treatment and mutual-help participation at the end of the three-month intervention period (referred to here as “end-monitoring”), and again three months later (referred to here as three-month follow-up).
To create the monitoring intervention, the authors adapted a manual designed for supporting patients during the transition from inpatient to outpatient settings. The authors enhanced this manual by adding components of motivational interviewing to all sessions, emphasizing the importance of empathy and supporting participants’ self-efficacy to make changes to their substance use. Study therapists met with participants for one initial 50-minute, in-person session during their hospital stay. This meeting focused on introducing participants to the study intervention, and discussing a plan for attending follow up treatment, mutual-help groups, or both, following discharge. Participants also signed a contract stating the effectiveness of follow up treatment together with their personal plan to attend follow up treatment and/or mutual-help groups. After discharge, treatment consisted of 12 weekly, 15-minute phone sessions with the same therapist. During these sessions, the study therapist assessed for substance use as well as treatment and mutual-help group attendance over the preceding week. Study authors rigorously checked for how well therapists delivered the monitoring intervention showing generally high levels of therapist competence and fidelity.
In the usual care control condition, participants completed assessments on the same time schedule as those receiving the monitoring intervention but did not receive any monitoring phone calls. Of note, participants in both groups were offered outpatient follow up care within the same VA system where they completed detoxification treatment.
A team of research assistants conducted study assessments at baseline, end-monitoring, and three-month follow-up time points. These research assistants were “blinded” to study condition, meaning they did not know which participants were receiving the monitoring intervention and which were not. The primary outcome for this study was readmission to detoxification treatment during the follow up period, as reported by participants. Assessors also gathered information on secondary outcomes, which included outpatient treatment attendance, mutual-help group attendance, measures of addiction severity, and participants’ confidence in their ability to maintain abstinence from substances (“self-efficacy”).
The participants in this study were approximately 50 years old on average and were mostly male (95%) and white (76%). They had presented for detoxification treatment to manage their withdrawal from alcohol (68%), opioids (11%), or both (21%). Most (98%) had received inpatient detoxification at least once in the past, and more than half (60%) also reported a history of attending outpatient SUD treatment. The treatment and control groups did not differ from each other on any of these characteristics. Participation in the intervention and follow-up assessments was relatively high across the study period. Intervention group participants completed, on average, 7.5 of the 12 scheduled calls. Follow up assessment completion was high for both groups, with about 89% of study participants completing the final three-month follow up assessment.
WHAT DID THIS STUDY FIND?
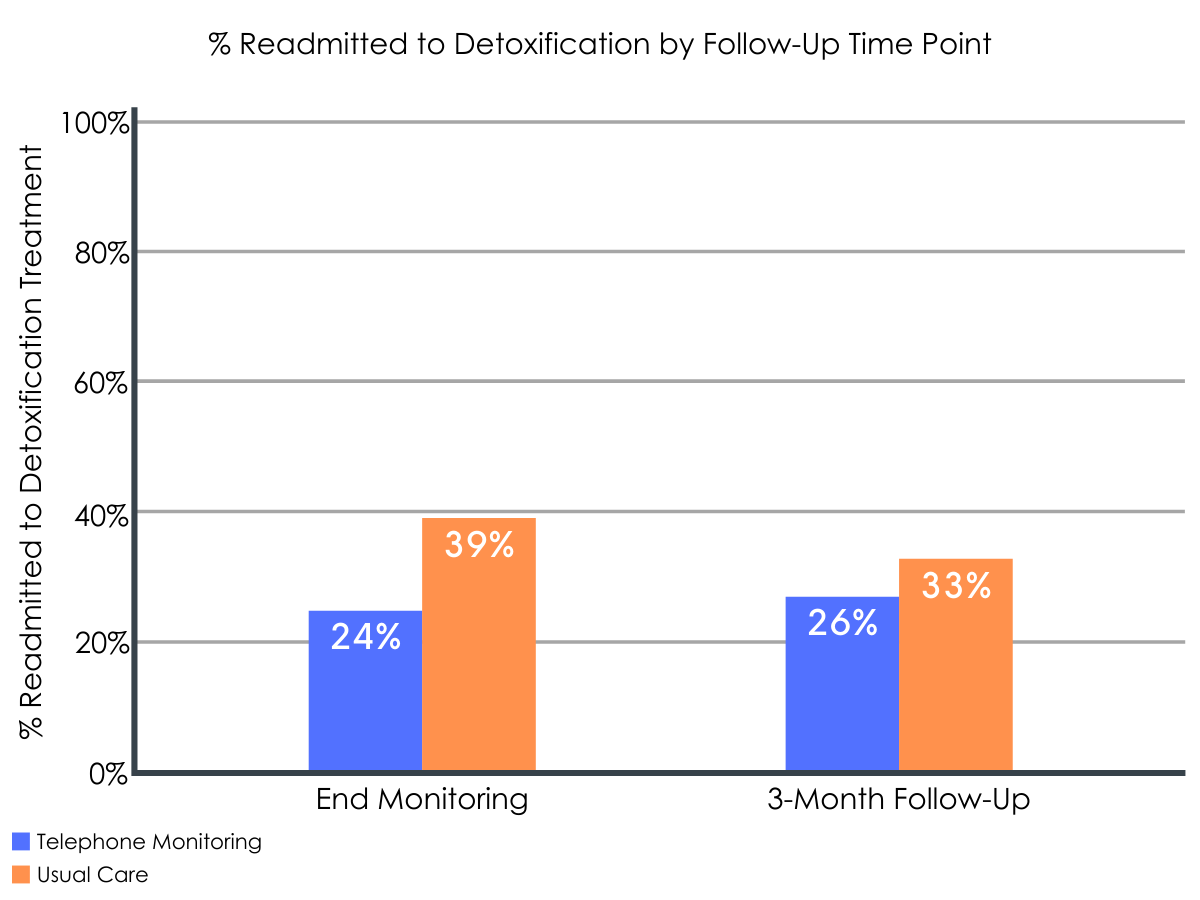
Figure 1.
By the end of the intervention period, participants in the telephone monitoring group fared better overall compared to usual care group participants.
The intervention group was significantly less likely to be readmitted to detoxification, with 24% reporting readmission compared to 39% of the usual care group. The intervention group also reported, on average, fewer days of substance use than the usual care group. For alcohol, the intervention group reported less than four days on average, compared to about six days in the usual care group. For opioids, the intervention group reported using less than one day, on average, compared to almost two days in the usual care group. Those in the intervention group, however, were no more likely than usual care participants to report attending outpatient treatment (24% intervention vs. 35% usual care) or mutual-help groups (72% intervention vs. 66% usual care) after discharge.
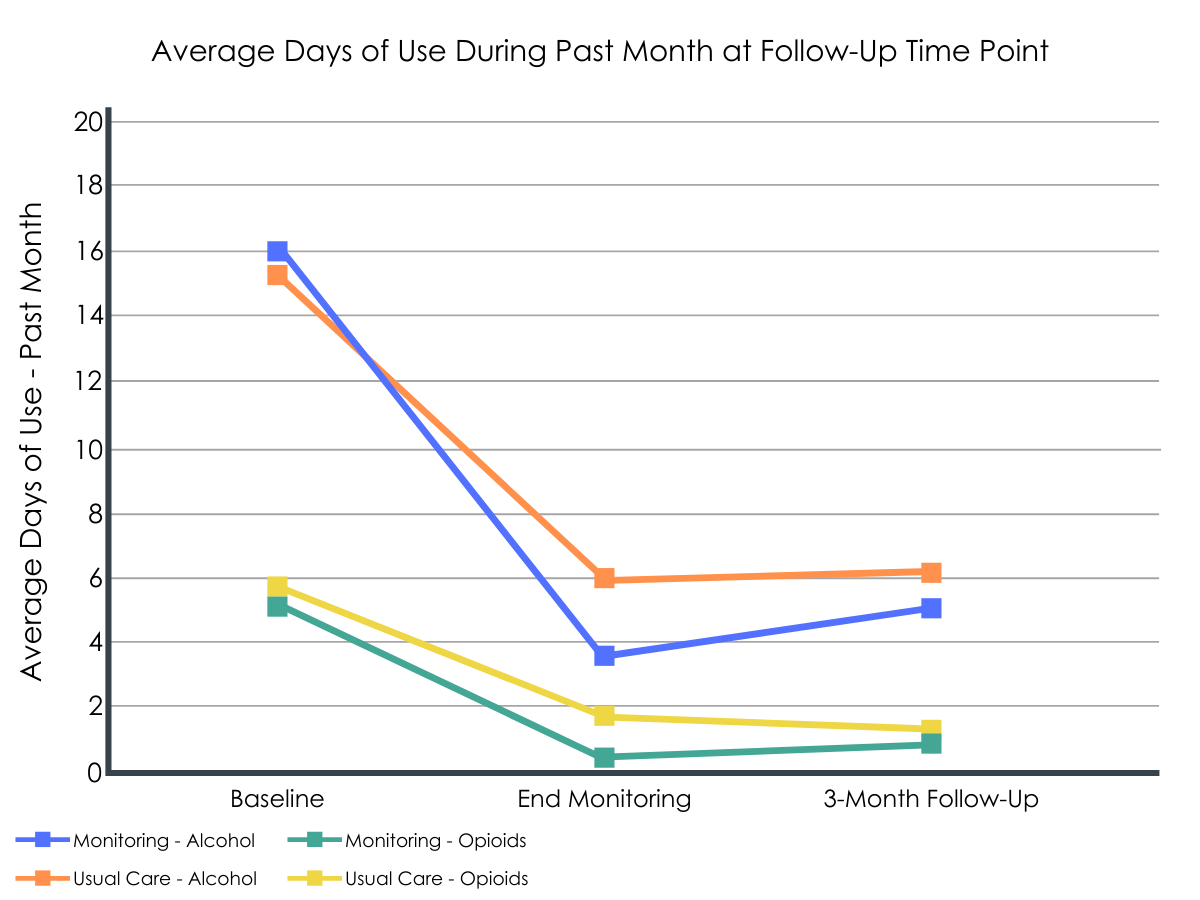
Figure 2.
At the three-month follow-up, the benefits of the intervention had dissipated.
Three months after the intervention period ended, participants reported similar rates of substance use and detoxification readmission across the two groups. While outpatient treatment attendance rates were similar for the intervention (30%) and usual care (35%) groups, a significantly higher percentage of usual care group participants (64%) attended mutual-help meetings during this period compared to the intervention group (53%).
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Many people who attend medically-supervised detoxification services to aid withdrawal from alcohol or drugs will be readmitted. Engaging in treatment, including medications, psychotherapy, and mutual-help after discharge reduces the risk of readmission to detoxification and improves overall outcomes. However, such engagement is too often the exception. Low-cost outreach follow-up interventions have the potential to increase the rates of post-detoxification engagement with supports and may even improve outcomes as standalone interventions. This study found that brief, weekly check-ins reduced overall substance use and the risk of readmission for detoxification during the three-month intervention period. These results align with similar studies showing that brief monitoring interventions after detoxification improve outcomes and reduce overall healthcare costs.
Contrary to expectations, the monitoring intervention did not increase attendance for outpatient treatment engagement or mutual-help groups. Although treatment engagement was the focus of the 15-minute intervention check-ins, the motivational approach of these calls from the study therapist may have functioned as a standalone treatment, increasing motivation more generally. In other words, the accountability of weekly check-ins with an empathic professional may have helped participants reduce their substance use regardless of whether they attended the additional in person treatment that was the specific focus of the check-in conversations. This would fit with other research showing that the frequency and intensity of research follow–ups can influence addiction treatment outcomes. However, without research examining the separate components of the intervention (known as “dismantling” studies), it is difficult to be sure which aspects of the intervention led to positive results. It is worth noting that rates of mutual-help attendance were quite high for both groups across both time points.
Figure 3.
Three months after the monitoring intervention ended, outcomes were similar across the two study groups. It is possible that the positive effects would continue with a longer format intervention, and as the authors note, the low cost and intensity of this treatment means that even longer-term formats could be impressively cost-effective in the long run. The loss of intervention effects soon after treatment ended is consistent with other research, and it is unclear how long an intervention would be required to see long lasting treatment effects. For example, one similar study of an 18-month intervention reported loss of treatment effects soon after the intervention ended.

Figure 4.
The goal of increasing follow up treatment engagement is an important one, given the frequency of readmission to inpatient detoxification and the broad ranging benefits of accessing support following discharge. Creative approaches to addressing barriers to follow up care are an important area of ongoing research. In addition to telephone interventions like the one in this study, there are efforts to increase access to more traditional forms of therapy using video platforms and smartphone-based interventions, ranging from text reminders to full “app”-based interventions, are also on the rise.
- LIMITATIONS
-
- This study compared a number of different outcomes across the two treatment conditions and did not adjust their analyses for this. This can be problematic from a statistical perspective, in that the more questions researchers test, the more likely they are to find a significant effect, and the less likely these effects are to be replicated in future studies.
- The study sample was predominantly male, which in part reflects higher rates of SUD among men and the higher proportion of male military service members. However, the gender distribution of service members is changing, and rates of SUD are rising among women, so it is important to replicate findings like these in more balanced samples.
- This study took place within the Veteran’s Affairs Healthcare system, which is an integrated healthcare system with a comprehensive continuum of care that differs from civilian treatment models in a number of ways. Lack of insurance barriers and psychosocial supports provided by Veteran’s Affairs facilities, such as housing and supportive work, may influence SUD treatment outcomes in a positive way compared to civilian settings. The integrated treatment setting may have also contributed to the high follow up rates in this study.
BOTTOM LINE
- For individuals and families seeking recovery: In this study, authors found that brief telephone check-ins reduced substance use and rates of readmission to detoxification treatment in the three months after discharge. The effects of this intervention dissipated, however, soon after it ended. The monitoring group did not increase treatment and mutual-help attendance, so it is possible that the positive effects on substance use and readmission were less the result of specific intervention techniques and more by the benefits of ongoing, frequent check-ins with an empathic professional. The main goal of detoxification treatment is medical management of withdrawal symptoms, which means that receiving empirically-supported treatment (e.g., therapy, medication, mutual-help attendance) for the substance use disorder itself is important. Treatment may be offered in a variety of formats, ranging from telephone follow ups to outpatient treatment. If a facility offers follow-up support in a nontraditional format, the evidence thus far is that these can be effective for reducing risk of return to substance use and may be easier to engage with in a consistent manner. Importantly, mutual-help groups are also an empirically-supported resource for improving outcomes following detoxification and may be easier to access based on location and timing than outpatient treatment.
- For treatment professionals and treatment systems: In this study, authors found that weekly, telephone-delivered 15-minute check-ins improved some SUD outcomes following detoxification; for example lowering rates of substance use and readmission during the active treatment phase. However, since the monitoring group did not attend treatment and mutual-help more frequently (the main focus of check-in), it is possible that the positive outcomes were due to general effects of regular follow ups rather than the intended targets of the intervention which was to increase outpatient treatment participation and mutual-help attendance. Readmission rates following detoxification admissions are quite high, and many do not access follow up care after discharge. Those who do experience substantial benefits, which highlights the importance of increasing rates of engagement with treatment and mutual-help following detoxification. Treatment systems wishing to reduce readmission rates and improve overall outcomes may consider incorporating active outreach and monitoring approaches, like the one used in the current study, following discharge from inpatient detoxification.
- For scientists: In this study, authors found that a weekly monitoring intervention decreased substance use and readmission rates following discharge from inpatient detoxification treatment. Three months after the intervention ended, the positive effects had dissipated. The intervention group did not attend more outpatient treatment or mutual-help meetings than the usual care group at either time point, despite the focus on in-person treatment engagement during the weekly intervention calls. It is possible that the positive outcomes reported are the result of study check-ins overall rather than the specific focus of the intervention, and future research would need to take a dismantling approach to disaggregate the active components of this very brief intervention. Increasing rates of engagement with follow up care is an important goal for addiction treatment and research, given low rates of follow up together with increased mortality for those who do not engage in care after discharge. As technology increases the range of creative solutions available for this problem, future work will need to identify the most resource-friendly approaches to supporting sustained changes for those seeking treatment for SUD.
- For policy makers: In this study, authors found that weekly, 15-minute telephone-delivered check-ins improved some SUD outcomes following detoxification, lowering rates of substance use and very importantly, expensive readmissions to detoxification settings during the active treatment phase. The intervention did not lead to increased in-person treatment and mutual-help attendance, so the study outcomes may be accounted for less by the intervention’s ability to increase such attendance and more by the benefits of ongoing, frequent check-ins with an empathic professional who can provide accountability and raise consciousness around relapse prevention. Readmission rates following detoxification admissions are quite high, and people who do not follow up after discharge or more likely to be readmitted and also more likely to die. Telephone monitoring interventions are a cost-effective way to support recovery and improve outcomes, and allocating resources to further examining how to improve these types of active outreach interventions may help improve outcomes and save money in the long run through reduced need for multiple detoxification admissions. In addition to supporting further research in this area, current insurance reimbursement models may not always support this intervention format and may be worth revisiting in light of these and related findings.
CITATIONS
Timko, C., Below, M., Vittorio, L., Taylor, E., Chang, G., Lash, S., . . . Brief, D. (2019). Randomized controlled trial of enhanced telephone monitoring with detoxification patients: 3-and 6-month outcomes. Journal of Substance Abuse Treatment, 99, 24-31. doi: 10.1016/j.jsat.2018.12.008

