21st century Addiction Treatment: Integrating Technology into Community Programs
The field of telemedicine – a term used to describe technology-based or facilitated interventions (contrasted with conventional face-to-face interventions) – has made growing contributions to clinical addiction research.
Although not without exception, telemedicine interventions including telephone-based services, videoconferencing, smartphone apps, and web-based interventions have shown promise in clinical research studies.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
For example, patients with alcohol use disorder randomly assigned to use a smartphone “app” called Addiction-Comprehensive Health Enhancement Support System (A-CHESS) in addition to standard continuing care after residential treatment had fewer risky drinking days (risky drinking is defined as 4+ drinks for a man or 3+ for a woman in a 2 hour period or less) than patients who engaged with only standard continuing care (see here).
However, community treatment programs have not widely adopted these evidence-based telemedicine applications due to several barriers including the prevailing insurance reimbursement model that typically does not cover these services.
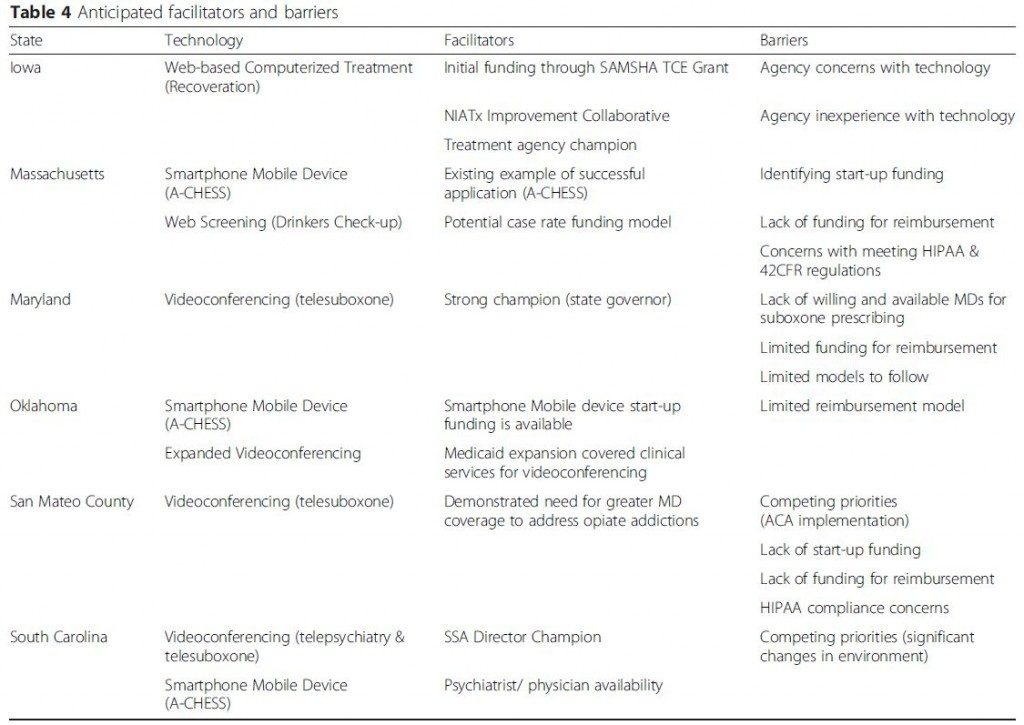
The current study sought to examine facilitators of and barriers to integrating telemedicine into addiction treatment programs in 5 states (Iowa, Maryland, Massachusetts, Oklahoma, South Carolina) and 1 county (San Mateo) as part of the Substance Abuse and Mental Health Services Administration-funded Strengthening Treatment Access and Retention – State Implementation (SAMHSA-funded STAR-SI) program.
HOW WAS THIS STUDY CONDUCTED?
In the current study, each state/county was represented by groups of payers who oversee federal and state funding for substance use disorder treatment programs.
In addition to selecting telemedicine applications and developing a proposal to implement these applications, payers identified facilitators and barriers to implementation. Researchers used Eisenhardt’s iterative Process of Building Theory from Case Study Research, which focuses on using qualitative data from individual cases to build a testable set of hypotheses (see here for more information on this qualitative analysis procedure).
WHAT DID THIS STUDY FIND?
Apart from South Carolina and San Mateo county (California), states had already been using telemedicine applications in clinical practice, including telephone-based services, videoconferencing, and a web application called Recoveration which facilitates online communication between therapists and patients between sessions.
Anticipated benefits of telemedicine applications that were chosen for the STAR-SI project included enhanced reach to patients who might not otherwise be able to access treatment and increased recovery support between sessions.
Facilitators to implementation included:
- having state leadership in support of their use
- funding or a reimbursement model to support their use
- existing examples of how the applications are used
Barriers to implementation included:
- lack of funding
- concerns about confidentiality
- absence of an implementation model that could be used as a guide
Qualitative studies like this one could inform research that evaluates the effect of implementing evidence-based telemedicine applications in real-world clinical settings on patient outcomes.
WHY IS THIS STUDY IMPORTANT
The study highlighted the challenges of adoption of evidence-based telemedicine applications in real-world health care systems that operate in a third-party payer model (e.g., billing insurance companies for individual services rendered).
Enhancing treatment and recovery through evidence-based telemedicine applications may be a complex and multi-step process. This process is informed by clinical research and ultimately requires a collaborative effort by funding sources, community treatment programs, policy makers, and third-party payers.
- LIMITATIONS
-
- It is unclear whether benefits of telemedicine applications, as well as facilitators and barriers identified by policy makers in these six areas, are representative of all relevant groups that allocate state and federal funds for substance use disorder (SUD) treatment.
NEXT STEPS
The next steps include evaluating the extent to which real-world clinical settings adopt these services, patient satisfaction and engagement with these services, and measuring the effect of their implementation on patient outcomes over time.
BOTTOM LINE
- For individuals & families seeking recovery: Clinical research suggests several telemedicine or mobile health applications can reduce drinking or other drug use and may boost chances for remission and recovery. Although not limited to these, several smartphone applications including A-CHESS, and web-based interventions including the Therapeutic Education System, have been shown to improve treatment outcomes. Some may require a fee to access them while others may be free. At present, few community programs use these applications, so ask a therapist or program director about how to access them.
- For scientists: Research is needed on the adoption and implementation of telemedicine, or mobile health, applications to build on clinical research that has examined its efficacy.
- For policy makers: Strongly consider funding that is dedicated to enhancing the adoption of technology-assisted interventions shown to improve patient outcomes in clinical research.
- For treatment professionals and treatment systems: In the absence of state or federal funding or a model that enables providers to bill services that use telemedicine applications, consider linking your patients with free or relatively inexpensive mobile applications and web-based services that have been shown to improve patient outcomes (e.g., moderatedrinking.com).
CITATIONS
Molfenter, T., Boyle, M., Holloway, D., & Zwick, J. (2015). Trends in telemedicine use in addiction treatment. Addict Sci Clin Pract, 10, 14. doi:10.1186/s13722-015-0035-4

