Screening for alcohol use disorder in primary care medical settings: There’s an avatar for that
Screening for alcohol use disorder in primary care medical settings has been a public health priority for some time. In the context of a busy medical practice, however, this kind of screening can often get missed, and sometimes when needed, appropriate referrals don’t get made. This study assessed a new computer-driven, avatar-based intervention designed to screen for alcohol use disorder in primary care medical settings and make referrals to treatment.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
In the early 2010s, the Substance Abuse and Mental Health Services Administration (SAMHSA) announced its goal of more aggressively screening for alcohol use problems in medical settings. By identifying alcohol use problems in primary care clinics and emergency departments, more people could be directed to treatment to address their drinking problem. In turn, these initiatives may be the impetus needed to actively link individuals with more severe forms of alcohol use disorder to specialty substance use disorder care. For others, these screenings might help catch a worsening alcohol problem before it progresses (e.g., to alcohol use disorder), in turn, avoiding many drinking-related consequences. To help achieve this goal, they introduced the Screening, Brief Intervention and Referral to Treatment initiative – best known by its acronym SBIRT.
While this kind of alcohol problem screening has demonstrated efficacy (i.e., it works under best case conditions like a well-controlled research study), interventions like SBIRT have been hard to implement in primary care medical practices, and have demonstrated limited effectiveness in these real-world settings. Barriers include an already very high burden on treatment providers’ time, competing assessments that need to be done for other issues, and complex electronic medical record systems in which information and notifications can be missed.
It is thought that advances in computer technology could be leveraged to improve the uptake and implementation of brief alcohol use problem screening intervention in medical settings. In theory, by computerizing/animating the intervention, nurses and doctors would have less task burden, screening would be more likely to get done, and as a result, appropriate referrals would be more likely to be made.
Computer-based relational agents—computerized avatars designed to build social-emotional relationships with people—represent a promising new line of intervention technology that can be used in medical settings. As noted by the researchers, relational agents are designed to simulate face-to-face counseling, build rapport, and establish a therapeutic alliance, and can be tailored to respond to incoming information from patients in real-time. Relational agent interventions have been shown to be effective in promoting behavior change, but had not been used to address substance use problems until this study.
The researchers in this study developed a relational agent and tested it in the context of three, busy, primary healthcare clinics in the US Veteran’s Health Administration system.
HOW WAS THIS STUDY CONDUCTED?
This study was a randomized trial with 192 participants receiving care in one of three US Veteran’s Health Administration primary care clinics, who received either alcohol problem screening using a relational agent + treatment as usual, or treatment as usual only, to determine the effectiveness of this computer-based intervention. Study outcomes included alcohol use between study baseline and 3-month follow-up, and rates of brief intervention and referral to treatment.
Eligibility criteria included: 1) a positive Alcohol Use Disorders Identification Test-C screening (AUDIT-C; ≥ 3 for women and 4 for men in the last 3 months), 2) drinking above the National Institute on Alcohol Abuse and Alcoholism (NIAAA) guidelines within the past 30 days (i.e., > 3/7 standard drinks per day/week for women, > 4/14 drinks per day/week for men), 3) current stable phone number and address for follow-up, and 4) willingness to provide contact information for at least one “locator” (i.e., a person who always knows their whereabouts for follow-up). Participants were excluded if they had past 30-day substance use treatment.
Treatment as usual included standard annual screening by the nurse or health technician for alcohol problems using the 3-item AUDIT-C. In line with standard procedure, patients’ primary care physician was alerted through the electronic medical record if the patient screened positive and were prompted to provide a brief intervention using a prepared checklist of items, and then refer patients who score 8 or above to specialty care. Patients were recruited to the study after this process concluded.
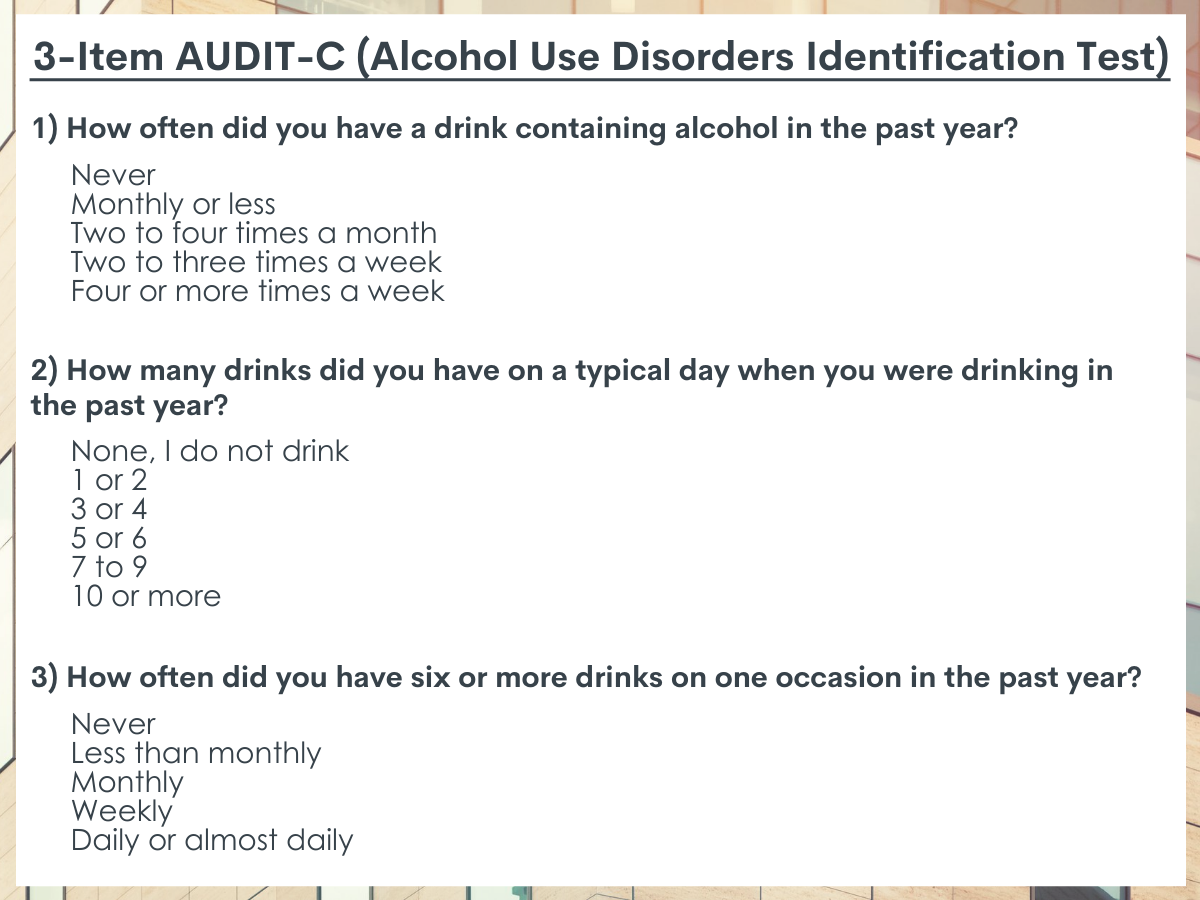
Participants randomized to the relational agent group met with the computerized relational agent the same day as their primary care medical appointment after they had completed the usual clinic screening procedures (i.e., the 3-item AUDIT-C), and again for a follow-up appointment with the relational agent 1 month later. The relational agent is programmed to speak with patients, who respond by choosing buttons containing phrases on a touch screen. The relational agent administered the full-length AUDIT because additional information was needed to conduct the brief intervention. It was designed to deliver the same kind of care as the primary care physician would ideally deliver and to conform to SBIRT procedures.

The brief intervention was based on Motivational Interviewing strategies, such as eliciting concern about consequences of drinking, bolstering motivation (e.g., importance, confidence, and readiness rulers; decisional balance exercise), and providing reflections and summaries of the interaction. At the end, the relational agent asked for a commitment to change. If the participant screened positive for alcohol problems, the relational agent offered a treatment referral and generated a report for the patient. Because all participants also received usual alcohol problem screening from the clinic, it is possible some participants were intervened on twice, however, because of the way referrals are delivered in the primary care clinics housing this study, participants only ever received one referral at the end of their clinic visit.
At study entry (i.e., baseline), all participants were administered questionnaires assessing past 30-day alcohol consumption, and recent negative consequences associated with their drinking. Then, three months after study entry, all participants were contacted by phone, and these items were readministered. For patient encounter information, such as brief intervention received and referrals made, the researchers used data collected and stored by the relational agent software, as well as data recorded by primary care providers and/or primary care providers staff within patients’ electronic health records during their in-person visits.
In total, 192 patients were enrolled and randomized to the relational agent + treatment as usual intervention arm (n= 95) or treatment as usual only arm (n= 97). A total of 1,417 (88.1%) individuals were excluded from randomization, with 175 participants not meeting inclusion criteria and 1,242 participants declining to participate. Fifteen participants were excluded from analyses due to mistakes in eligibility found after randomization, resulting in a final sample for analysis of 178 patients.
Participants were 89% male, 21% female, with the majority of participants identifying as 67% White (67%). 89% of participants completed the 3-month follow-up. Treatment arms were similar on demographic measures, however, the relational agent + TAU group endorsed fewer average drinks per day and drinking days per week at study baseline but some regarding baseline alcohol scores.
WHAT DID THIS STUDY FIND?
Groups had similar reductions in alcohol use.
Participants receiving the relational agent intervention and treatment as usual only both reduced their average number of drinks per drinking day by around 1 drink per day, and heavy drinking days per week by around 1 drink per week from baseline to 3-month follow-up, with the groups being similar in their extent of drinking reductions.
Participants in the relational agent group were more likely to receive a brief intervention about their drinking and get referred to treatment.
As would be expected given the automated nature of its screening protocol, all participants in the relational agent + treatment as usual condition received brief intervention via the relational agent platform, compared to 43.8% from their primary care physician providers in the treatment as usual only group.
In total, 25 participants received a referral to specialty substance use disorder treatment: 24 in the relational agent + treatment as usual group, and 1 from their primary care physician in the treatment as usual group. Seventy-one percent of participants attended the referral appointment.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Though the relational agent and treatment as usual only groups appeared to produce similar benefits in terms of reducing alcohol use over the study period, the relational agent intervention was much more effective at intervening when problem drinking was detected and referring patients to treatment.
Many things may get in the way of a primary care physician intervening and making a referral to treatment when screening forms detect problematic alcohol use. For instance, in the context of the primary care appointment, physicians may have to prioritize addressing other medical concerns, or may not see screening scores in time. A clear benefit of a relational agent is that intervention is automatically delivered with precision and consistency when a patient hits a certain threshold on a screener and can deliver a referral.
One concern is that patients may not follow up on a referral given to them by a computerized relational agent. This however did not appear to be the case, with 71% of participants attending their first referral appointment to specialty treatment, which is on par with typical attendance rates for substance use disorder referral appointments. Future work is needed, however, using tools like the Washington Circle Group criteria for ‘treatment engagement’, to determine whether these referrals are leading to actual specialty treatment engagement versus simply showing up for an initial treatment appointment.
The authors also highlight that participants in the relational agent condition started out with lower drinking levels and thus had less room to improve. The control group, by comparison, had higher baseline levels of alcohol use and more room to improve. If alcohol use in the relational agent condition was similar to the control condition at baseline, it’s possible that the relational agent intervention may have in fact product a statistically significant improvement in drinking. It’s also possible, however, that participants were not engaging in treatment after initial referral (even though the majority of participants got to an initial specialty treatment session), or that longer term follow-up was needed to capture an intervention effect on alcohol use (i.e., beyond 3 months).
It’s important to note that the relational agent can provide SBIRT without burdening primary care staff and could be administered in many contexts outside of the clinic. Also, the efficiency of the relational agent could lead to more consistent assessment of alcohol use problems without placing more administrative burden on clinical staff.
- LIMITATIONS
-
As noted by the authors:
- The current study was limited in that eligibility was determined by, and recruitment was contingent on AUDIT-C scores obtained by clinic staff who appear to have administered the measure in an inconsistent manner.
- Generalizability of the results should be interpreted in light of under-representation of women, which is expected in the male-dominated veteran population, and racial and ethnic diversity.
Also:
- All participants received some form of alcohol problem screening; thus, the study lacked a true control group limiting the researchers’ capacity to explore how the relational agent may have influenced drinking outcomes versus no screening whatsoever.
- Many individuals with screener scores suggesting problematic alcohol use declined participation in the study, suggesting enthusiasm for engaging with a computerized relational agent about one’s alcohol use is low, although this may simply reflect a lack of enthusiasm many individuals have for discussing a potential drinking problem.
BOTTOM LINE
This randomized trial of a relational agent-based intervention for alcohol use disorder showed that technology can be leveraged to deliver screening and referral to treatment for alcohol use problems in primary care medical settings. While this intervention did not produce greater reductions in drinking than a standard SBIRT intervention, it was much more consistent in terms of intervening when problematic alcohol use was detected and making referral to treatment.
- For individuals and families seeking recovery: This study demonstrates the potential benefit of technology-based screening interventions for alcohol use problems in primary care medical settings. A great potential benefit of this kind of intervention is that problematic drinking might be caught sooner, avoiding further consequences for those with alcohol use disorder for some, or before it progresses to full blown alcohol use disorder for others. Overall, these approaches could help individuals with drinking problems connect to care and catalyze the recovery process for those who otherwise may not be actively seek help.
- For treatment professionals and treatment systems: This study demonstrates the potential benefit of technology-based screening interventions for alcohol use problems in primary care medical settings, and highlights some of the benefits of automating aspects of the SBIRT screening process. Such technology-based solutions have the potential to cover existing gaps in the SBIRT process, though more research is needed to understand how best to deliver the services so that individuals receive effective and ongoing care.
- For scientists: This study demonstrates the potential benefit of technology-based screening interventions for alcohol use problems in primary care medical settings, and highlights some of the benefits of automating aspects of the SBIRT screening process. Such technology-based solutions have the potential to cover existing gaps in the SBIRT process. More research is needed however to fully understand the potential of such interventions and their mechanisms of action. Future work is also needed to determine whether these referrals are leading to actual specialty treatment engagement versus simply showing up for an initial treatment session.
- For policy makers: This study demonstrates the potential benefit of technology-based screening interventions for alcohol use problems in primary care medical settings, and highlights some of the benefits of automating aspects of the SBIRT screening process. Screening for problematic alcohol use in primary care and other medical settings has already had a major impact on public health. Supporting initiatives that improve existing screening approaches has tremendous benefit to further improve public health by identifying problematic drinking before it progresses to more severe forms of harmful drinking (e.g., alcohol use disorder) and helping people with drinking problems connect to care who otherwise may not be actively seeking help.
CITATIONS
Rubin, A., Livingston, N. A., Brady, J., Hocking, E., Bickmore, T., Sawdy, M., . . . Simon, S. (2021). Computerized relational agent to deliver alcohol brief intervention and referral to treatment in primary care: A randomized clinical trial. Journal of General Internal Medicine, [Epub ahead of print]. doi: 10.1007/s11606-021-06945-9

