Same-day versus delayed buprenorphine prescribing: Does timely treatment enhance retention?
The opioid use disorder medication, buprenorphine (i.e., Suboxone, Subutex), can ease opioid withdrawal and craving and help prevent opioid overdose. However, discontinuation of buprenorphine treatment is an ongoing concern and there is a need to evaluate factors that might influence a patient’s decision to stay in or discontinue it. One factor that might play a role in treatment retention, but requires further research, is the time at which buprenorphine treatment is started. This study assessed the relationship between prescribing practices (same-day vs. delayed prescribing to patients wishing to start buprenorphine), patient characteristics, and treatment retention after 30 days.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Buprenorphine (e.g., Suboxone, Subutex) is a medication used for the treatment of opioid use disorder. With the potential to ease withdrawal and craving, and prevent opioid overdose, buprenorphine is a key player in the fight against the opioid epidemic. Despite the benefits of this lifesaving medication, treatment dropout is an ongoing concern. About two-thirds of individuals discontinue their buprenorphine within the first 6 months of treatment, with dropout most commonly occurring in the first month of treatment. This is important because receiving buprenorphine treatment for longer than 6 months is associated with substantially reduced risk of overdose and fewer emergency department visits and hospitalizations.
Patients’ treatment experiences and their providers’ clinical decisions at the early stages of treatment, including the dose, duration, and timing of buprenorphine initiation, might have an influence on treatment success.
Treatment guidelines recommend that providers do a comprehensive medical assessment to evaluate the patient’s suitability for buprenorphine. However, there are no established set of rules as to whether or not patients should be started on buprenorphine at the first medical visit. Studies suggest that same-day prescribing (starting a patient on buprenorphine during the first medical visit, without any delays) may be much less common than delaying prescribing to subsequent office visits. This may be due to the difficulties of same-day prescribing, including factors like appointment availability and staff resources at medical facilities, patients’ willingness to start treatment at the first office visit, and a provider’s level of concern with obtaining medical testing results (e.g., blood tests for liver function and urine drug testing) prior to prescribing.
Regardless, delaying treatment has the potential to negatively affect treatment initiation, retention, and outcomes. For example, patients might reduce or stop their illicit opioid use in anticipation of starting buprenorphine at the first office visit, and delays might result in frustrations and lack of trust in the medical system that drive patients away from treatment and back to opioid misuse, increasing their risk for opioid overdose due to a reduced opioid tolerance after cutting back. On the other hand, delaying treatment might help providers identify whether or not a given patient is a good candidate for buprenorphine treatment to ultimately improve patient outcomes.
There has been little research, however, that looked at the effects of buprenorphine treatment timing on patient’s treatment outcomes. Identifying the potential benefits and harms of different initiation methods can help us better understand the best prescribing practices for helping individuals achieve successful treatment and recovery outcomes. The current study assessed the relationship between prescribing practices (same-day vs. delayed), patient characteristics, and treatment retention 30 days after patient’s received their first buprenorphine prescription.
HOW WAS THIS STUDY CONDUCTED?
The investigators conducted a retrospective cohort study of 237 individuals who started buprenorphine treatment at a community health center between June of 2015 and December of 2017. Data were obtained from the medical records of a single buprenorphine treatment program within a large primary care practice located in an urban area with high rates of poverty and opioid overdose deaths. At the time of investigation, this facility was designated as a federally qualified health care center and had a large volume of buprenorphine waivered prescribers (13 providers). Standardized medical intakes and evaluations were typically completed by the program’s buprenorphine coordinator (i.e., a clinical pharmacist). However, buprenorphine prescribing primary care physicians were also able to initiate buprenorphine before the patient completed their full medical evaluation.
Patient requests to start buprenorphine were made by phone, in person, or during the primary care visits. After making a request, patients were scheduled for an intake appointment with the buprenorphine coordinator (i.e., clinical pharmacist) and/or primary care physician. Patients could either receive same-day buprenorphine prescriptions (prescribing at the patient’s first medical visit without any delays in treatment), or be scheduled for a follow-up visit to start buprenorphine at a later date (i.e., delayed buprenorphine prescribing, requiring multiple doctor’s visits for medical evaluation before starting the patient’s treatment). According to national guidelines, the health care center did not offer buprenorphine to patients with severe alcohol / benzodiazepine use disorder and/or patients taking more than 60mg of methadone per day. Patients included in this study were required to have received at least one buprenorphine prescription within the study period.
The researchers (1) compared socio-demographics and clinical characteristics between patients with delayed and same-day buprenorphine treatment, (2) evaluated whether different providers were linked to specific prescribing patterns (same day vs. delayed) and treatment retention outcomes, and (3) assessed relationships between same day / delayed buprenorphine prescribing and retention in treatment over a period of 30 days.
To assess same-day and delayed prescribing, the research team measured the amount of time between an individual’s first request for buprenorphine treatment and when a provider actually wrote a given patient their first buprenorphine prescription. When delays were observed, the length of the delay was categorized as short (1-7 days between request and prescription), medium (8-14 days), or long (15-30 days). Examination of prescription delays was limited to those individuals who experienced delays of less than or equal to 30 days to avoid the influence of factors outside the provider’s control. Same-day prescriptions were defined as receipt of buprenorphine prescription during the first health care appointment without delays (categorized as yes vs. no). 30-day treatment retention was defined as having an active prescription between 30 and 90 days after the date of the first buprenorphine prescription.
Other clinical and demographic measures that were documented in patient medical records and assessed in this study included age, sex, race/ethnicity, benzodiazepine use in the past 30 days (confirmed by self-report and/or positive urine drug tests at the time of patients’ intake appointments), and the name of each patient’s initial provider who made decisions around same day versus delayed buprenorphine prescribing.
Of the 237 patients who received buprenorphine between June of 2015 and December of 2017, 222 individuals (94%) had delays of less than or equal to 30 days and were included in the analysis (i.e., 15 individuals were excluded from the study due to prescribing delays greater than 30 days). The final sample mostly consisted of publicly insured (74%), middle-aged (average of 46 years), Hispanic (72%) men (79%).
WHAT DID THIS STUDY FIND?
The majority of patients (i.e., 133 out of 222) experienced delays in receiving their first buprenorphine prescription.
About 60% of patients experienced delays in treatment, whereas only 40% of individuals received same-day prescriptions. Among patients who experienced prescription delays, it took an average of about 8 days from requesting to obtaining their first buprenorphine prescription. A short delay (1-7 days) was most common, followed by medium delays and long delays in buprenorphine receipt.
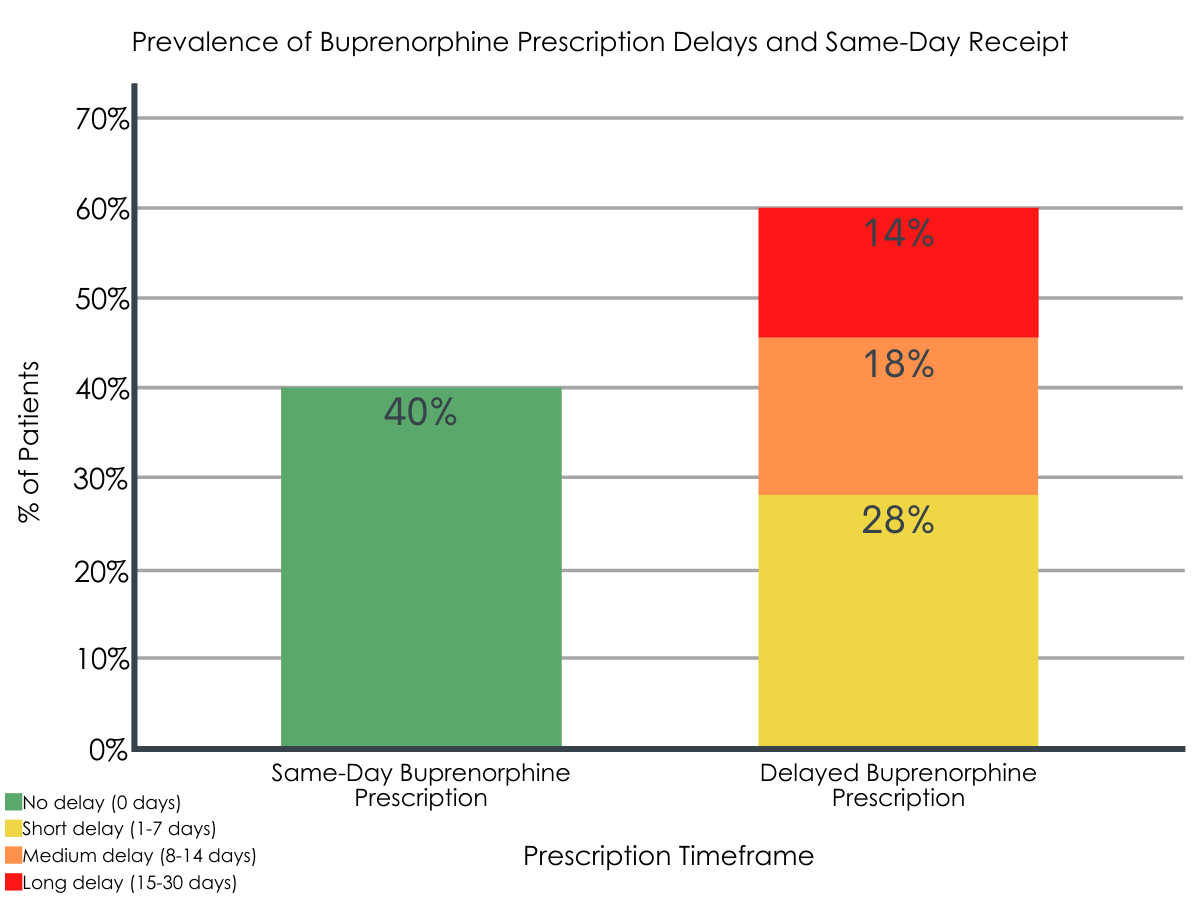
Figure 1. Figure depicts the percentage of patients who received same-day and delayed buprenorphine prescriptions. Delayed prescriptions were categorized based on the amount of time from initial treatment request to prescription receipt.
Race/ethnicity, substance use, and initial provider interactions differed between patients with same-day and delayed buprenorphine receipt.
Patients who experienced delays in treatment were more likely to be non-Hispanic White individuals (11% vs. 2%), and engage in alcohol (43% vs. 21%) and benzodiazepine (22% vs. 9%) use in the 30 days prior to their intake appointment. Compared to those who received same-day prescriptions, patients with delayed buprenorphine receipt were more likely to have seen the buprenorphine coordinator, rather than one of the primary care physicians, as their initial provider at intake (57% vs. 13%).
The odds of treatment retention were similar for same-day and delayed prescribing, but lower among individuals who engaged in benzodiazepine use and saw a provider with low patient volume.
Among the entire sample of patients, 80% remained in treatment after 30-days of buprenorphine therapy. Controlling for demographic and other clinical characteristics, patients who received same-day and delayed buprenorphine prescriptions had generally similar retention rates.
Though same-day buprenorphine receipt was not associated with treatment retention, patients’ misuse of benzodiazepines and their initial buprenorphine provider were.
Patients who did not use any benzodiazepines were 2.6 times more likely than patients who did use them to remain in treatment after 30 days of buprenorphine. Additionally, patients who had the buprenorphine coordinator, rather than a low volume prescriber (10 or fewer buprenorphine patients), as their initial provider were 2.8 times more likely to remain in treatment after 30 days.
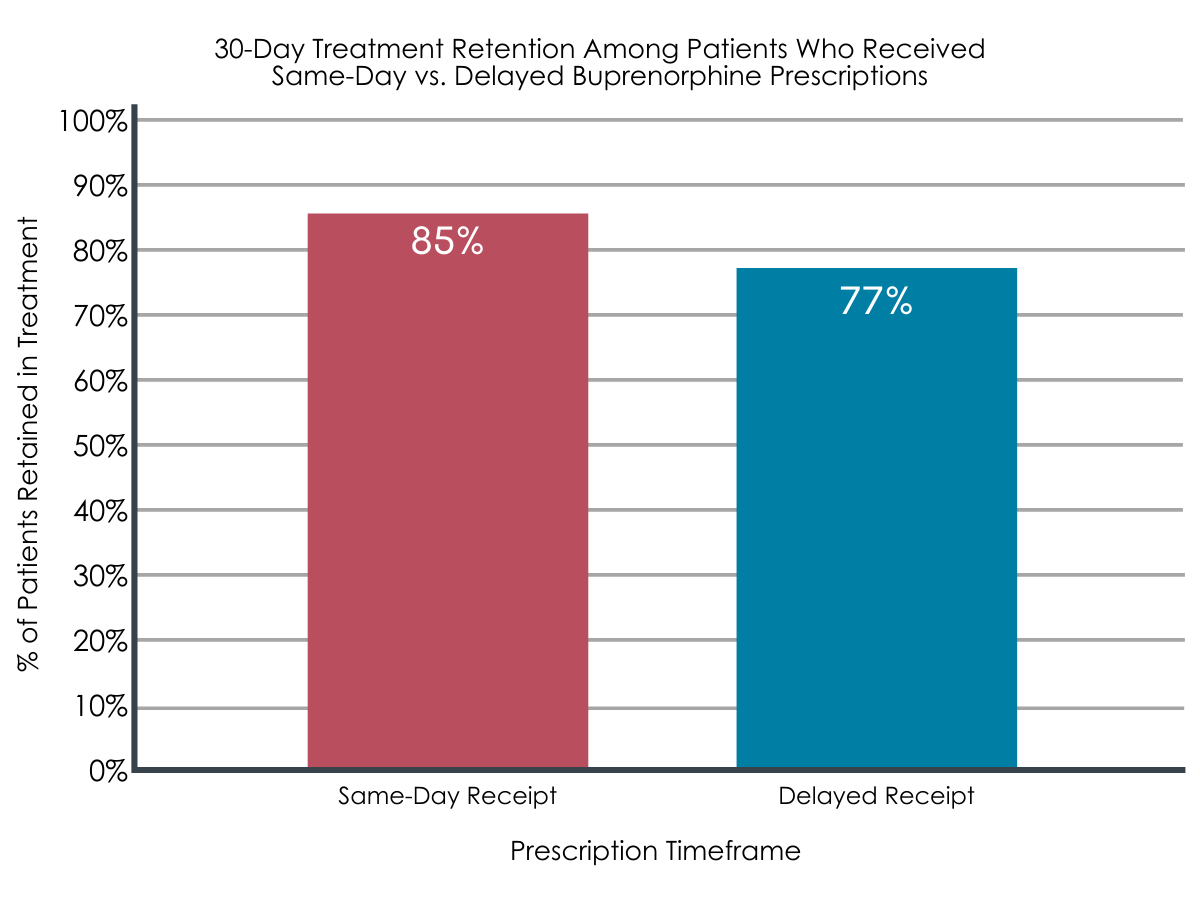
Figure 2. Figure depicts the percentage of patients who were still in treatment after 30 days. After controlling for demographic and other clinical characteristics, treatment retention did not significantly differ between the two patient groups.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Buprenorphine is a much-needed medication for the treatment of opioid use disorder. However, discontinuation of buprenorphine treatment is an ongoing concern and there is a need to evaluate factors that might influence patient’s decision to stay in or discontinue buprenorphine. The current study evaluated relationships between same-day buprenorphine prescriptions versus delayed prescriptions (not received during the first intake visit after requesting treatment) and retention in treatment after 30 days, as well as the influence of demographic and other clinical measures.
The majority of patients experienced delays in buprenorphine receipt, with most waiting about 1-7 days before they received a prescription. Interestingly, these delayed vs. same-day receipt was not associated with treatment retention after 30 days of buprenorphine treatment. This finding might suggest that delaying treatment initiation is not necessarily detrimental to remaining in treatment. Perhaps the benefits of the medication outweigh any frustration that might arise as a result of delayed prescribing. Alternatively, delays might give patients more time to make an informed decision about starting treatment. However, it is important to consider that all of the patients in this study had started buprenorphine treatment and might therefore represent a subset of the most motivated patients (i.e., returning to engage in treatment regardless of healthcare center hurdles or delays). Indeed, a large majority (80%) of these patients remained in treatment after 30 days. This might therefore reflect the fact that individuals who are motivated to engage in medication treatment are less likely to be affected by treatment delays. However, it is unclear what the program did to help patients during this initial delay in prescribing (e.g., coordinator check-ins with participants, etc.) and this might have influenced the current results if non-standard patient outreach was done during the delay period.
In addition, the current analysis does not speak to the number of individuals who expressed interest in treatment, arrived at their initial intake appointment, and did not return to receive a prescription due to prescription delays. Therefore, the effects of delayed buprenorphine receipt in this study could be underestimated, as delays might represent barriers to treatment entry that were not captured here. Additional research is needed to determine the effects of delayed prescribing on patients’ return to care after not obtaining their buprenorphine prescription at intake.
Of note, although no additional benefit was observed, same-day prescribing did not negatively affect treatment retention. Therefore, this study demonstrates that same-day prescribing is possible and may not harm patients. Given the current study’s sample, additional research is needed to determine the role of motivation in same-day versus delayed prescribing and initiation/retention outcomes, as same-day prescribing might be beneficial among patients who show interest in treatment but are less motivated in the initial stages of treatment seeking. Moreover, this study only looked at retention after 30 days of treatment and it is possible that differences in retention might emerge between patients who receive same-day and delayed prescriptions at later treatment stages.
Alcohol and benzodiazepine use were both related to greater likelihood of buprenorphine prescription delay. Providers might therefore be hesitant to prescribe buprenorphine to individuals who engage in alcohol and benzodiazepine use because both substances slow respiration and thus can be dangerous and potentially fatal when combined with buprenorphine, particularly at high buprenorphine doses.
This study also found that patients who used benzodiazepines were less likely to stay in treatment. Concurrent use of benzodiazepines and buprenorphine can increase risk for overdose and fatality by increasing respiratory depression.
Importantly, individuals who take prescription benzodiazepines with buprenorphine are 2 to 3 times more likely to experience an opioid-related overdose and associated fatality. Reasons for treatment dropout were not evaluated in this study. Therefore, it is possible that comorbid mental health conditions or overdose among individuals who use benzodiazepines and buprenorphine might have contributed to lower treatment retention (i.e., increased likelihood of treatment dropout). Although the combined use of prescribed buprenorphine and prescribed benzodiazepines has previously shown to somewhat increase the chances of treatment retention, the current study assessed the use of illicit benzodiazepines (use without a prescription), which could account for contradictory findings. Additional research is needed to clarify the role of benzodiazepine use in treatment retention. Despite the dangers of these drug interactions, it is important to consider the risk/benefit ratio, as the risk of untreated opioid use disorder might outweigh the risks of prescribing buprenorphine to individuals using other respiratory depressants. Providing patient education around the risks of concurrent use and requiring more frequent provider visits might help address provider concerns and enhance patient safety. Recovery coaching and daily check-ins may also help support such patients in their treatment and recovery. Although the exact reasons underlying delayed prescribing are not clear, prior research has reported provider concerns and prescribing barriers related to medication diversion, insurance issues, time constraints, and lack of available mental health or psychosocial support for patients. Addressing these concerns and barriers will ultimately help improve prescriber best practices and treatment access.
Patients receiving delayed instead of same-day buprenorphine treatment were more likely to be non-Hispanic White individuals, and to have had an initial provider appointment with the buprenorphine coordinator than a primary care physician. Interestingly, treatment retention was less likely among patients who had initial provider contact with a physician who had low buprenorphine patient volumes. Therefore, less experienced providers may not be as well versed in methods that can help keep patients engaged in treatment. Enhancing providers’ exposure to opioid use disorder patients and providing continuing education in this field might help to ensure optimal treatment experiences among patients and optimal provision experiences among a range of buprenorphine waivered prescribers.
Given that this study was conducted in the context of a single health care facility, additional research in this area is certain to further inform our understanding of how the timely receipt of medication treatment affects treatment initiation, retention, and recovery outcomes. Regardless of same-day or delayed prescribing, providing patients with additional check-ins or ongoing monitoring (e.g., technology-based check-ins, weekly patient reports of treatment benefits/difficulties) that enhances and maintains patient-provider communication, particularly at the beginning of treatment, might ultimately benefit patient retention.
- LIMITATIONS
-
- Examination of prescription delays was limited to those individuals who experienced delays of less than or equal to 30 days. Furthermore, it is not clear if patients who experienced delays sought treatment elsewhere or abandoned treatment seeking altogether. Among the entire sample of patients, 80% remained in treatment after 30-days of buprenorphine, and high rates of retention may have influenced outcomes. Studies are needed to examine whether same-day prescribing has effects on retention in programs/centers with lower retention rates.
- This study assessed a single health care center and results may not generalize to facilities located in non-urban environments with different operating procedures.
- The authors used medical records to obtain the time of patients’ first treatment request. Therefore, the first documented request for treatment may not be the actual first request if omitted from their medical record. The authors did not assess whether delays were considered appropriate or avoidable. Furthermore, data regarding substance use (e.g., alcohol, benzodiazepines) were incomplete or missing, limiting interpretation.
BOTTOM LINE
Studies like this help us better understand optimal opioid use disorder treatment protocols, as well as the factors that contribute to treatment retention. Focusing on buprenorphine, this study found that more than half of patients experienced delays (about 8 days) in receiving their buprenorphine treatment, and these patients were more likely to engage in alcohol and benzodiazepine misuse, but just as likely to be retained in treatment for 30 days. Importantly, same-day prescribing did not negatively affect treatment retention, suggesting that same-day prescribing is possible and may not harm patients when it comes to retention. Regarding the concurrent misuse of benzodiazepines and alcohol, providers might be hesitant to prescribe buprenorphine to individuals who engage in the misuse of these depressant drugs due to the increased overdose risk, but considering the risk/benefit ratio of prescribing to these individuals is essential given the risks of opioid use disorder when left untreated. Misuse of benzodiazepines was also related to a reduced likelihood of staying in treatment, highlighting the potential need for additional intervention/support among these patients. Given that patients who had an initial prescriber with a low buprenorphine patient volume had a reduced likelihood of retention, exposing providers to opioid use disorder patients and continuing education around medication treatment to further the patient-provider relationship might ultimately enhance treatment retention.
- For individuals and families seeking recovery: Although same-day buprenorphine prescriptions did not benefit treatment retention in this study, it was also not detrimental or harmful to retention. Despite mixed findings, individuals who misuse benzodiazepines may be more likely to drop out of buprenorphine treatment. Therefore, these patients should work with their providers to prevent treatment drop out and determine whether the risk of overdose with combined use outweighs the risk of untreated opioid use disorder. Individuals and families seeking treatment for the first time may also benefit from seeking out a provider with greater experience prescribing buprenorphine, as it might help retain patients in treatment.
- For treatment professionals and treatment systems: Although same-day buprenorphine prescriptions did not benefit treatment retention in this study, it was also not detrimental or harmful to retention. Given that the authors only evaluated patients who had success with receiving an initial buprenorphine prescription, it is still unclear if delayed prescribing might drive away less motivated patients who would otherwise benefit from treatment. Ongoing provider education around buprenorphine patients and prescribing might also help increase retention in buprenorphine treatment. Pending additional research, providers who are concerned about prescribing buprenorphine to patients who use alcohol or benzodiazepines might consider more frequent monitoring and check-ins as a method for reducing patient risk for harm.
- For scientists: Additional research is needed to evaluate whether same-day prescribing can benefit patients in other clinical environments and to determine the effects of patient motivation and delayed prescribing on patients’ return to care after not obtaining their buprenorphine prescription upon intake. Longitudinal research will help identify whether same-day prescriptions benefit longer-term treatment and recovery outcomes. Furthermore, additional mixed method studies will help elucidate the reasons why clinicians are or are not prescribing same-day buprenorphine, to help identify and address provider concerns. Innovative intervention (e.g., interim buprenorphine treatment and bridge services that initiate treatment and subsequently help patients transition to more permanent providers) should be developed and studied to further enhance treatment access and retention.
- For policy makers: Given that same-day buprenorphine prescribing did not affect treatment retention, it could be a potentially effective option for engaging patients in treatment who might not otherwise return if treatment were delayed. However, research on this topic is limited and this study was conducted at a single site, warranting additional studies to inform best-practice policies in health care environments, including the appropriateness of delaying buprenorphine treatment among individuals with concurrent benzodiazepine misuse. Given the risks of untreated opioid use disorder, and the need to enhance treatment seeking and retention among these patients, additional funding for research will help elucidate the most ideal provider practices for enhancing recovery and mitigating the opioid epidemic.
CITATIONS
Jakubowski, A., Lu, T., DiRenno, F., Jadow, B., Giovanniello, A., Nahvi, S., … & Fox, A. (2020). Same-day vs. delayed buprenorphine prescribing and patient retention in an office-based buprenorphine treatment program. Journal of Substance Abuse Treatment, 119, 108140. doi:10.1016/j.jsat.2020.108140

