Combining medication and adjunct services for opioid use disorder: Identifying cost-saving combinations that reduce risk of overdose and death
Given limited treatment resources and unmet treatment needs for opioid use disorder, it is essential to identify exactly which treatments are worth the investment. Looking at the effects of medication treatments alone and combined with psychosocial services, and their cost-effectiveness can help determine their benefits and what provides the greatest benefit at the lowest cost. This study evaluated the effects of medication and add-on services on overdose and death, as well as their cost-effectiveness.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Opioid use disorder is a major cause of death and disability. Medication treatments for opioid use disorder (e.g., agonists like methadone and buprenorphine, as well as antagonists like extended release injectable naltrexone) are effective and lifesaving and support successful treatment and recovery outcomes, reducing death and disability. Although previous studies have examined the effects and cost effectiveness of these medications, research has yet to look at the effectiveness of these medications in combination with other add-on treatments which, in some studies, have shown to enhance treatment retention and/or recovery outcomes.
Effectiveness studies help determine the benefits of various treatments and cost-effectiveness studies help determine which treatments are best when considering both the benefits the treatment produces and the economic resources needed to provide them. Together, this key combination of data can ultimately inform policies related to such treatments. The current study examined the effects of opioid use disorder medication treatment alone and in combination with three adjunct interventions (contingency management, psychotherapy, and overdose education/naloxone), on overdose and mortality, as well as their cost-effectiveness across an individual’s lifetime.
HOW WAS THIS STUDY CONDUCTED?
The authors conducted a model-based analysis of 100,000 simulated individuals representative of the US population with opioid use disorder to assess the effects of various treatments on fatal and non-fatal overdoses, as well as all-cause deaths (including those due to overdose) over a five-year period. The cost-effectiveness of each treatment was also evaluated across one’s lifetime, relative to no treatment.
Values entered into the model were based on the scientific literature, expert opinion, and data from the Veteran Affairs, which is the largest provider of addiction treatment in the United States. Medication treatment was assumed to include drug counseling and medication management (medication counseling ~2x per week).
Figure 1. Medication treatment with adjunct services.
The researchers evaluated three medication treatments, alone and in combination with three adjunct services. The following medication treatments and adjunct services were examined:
- Medication treatment (assumed medication-specific costs of the drug and its administration, based on data from the federal government):
- Methadone
- Buprenorphine (also known by the brand names Suboxone or Subutex)
- Injectable
- Adjunct services:
- Contingency management
- Assumed to consist of two 15-minute clinical psychologist sessions per week, with a weekly cost of $65 for personnel, drug screening, and incentive payments (i.e., paying patients for negative drug tests).
- Psychotherapy
- Assumed to consist of one 1-hour cognitive behavioral therapy session per week with a clinical psychologist, with a weekly cost of $83 per week.
- Overdose education and receipt of the overdose reversal medication, naloxone
- Assumed to cost $71 per session.
- Contingency management
To assess cost-effectiveness, the authors calculated the lifetime healthcare and criminal justice system costs for each medication treatment, alone and in combination with various adjunct services, and the quality adjusted life years (a measure of disease burden that takes into consideration the quality of life and length of life lived in a given health state, where higher values indicate better outcomes) associated with each treatment modality. Health care costs included age, sex, and state–specific health care costs, overdoses, and treatment, while criminal justice costs included the cost of crimes related to a given treatment. Cost effectiveness was examined as the cost of treatment for each quality adjusted life year gained, relative to no treatment.
WHAT DID THIS STUDY FIND?
In the absence of treatment, there were 42,717 overdoses and 12,660 all-cause deaths.
Of 100,000 simulated patients and in the absence of treatment, an estimated 43% would be expected to overdose and ~13% would be expected to die from all causes (including fatal overdose) at some point over a five-year period.
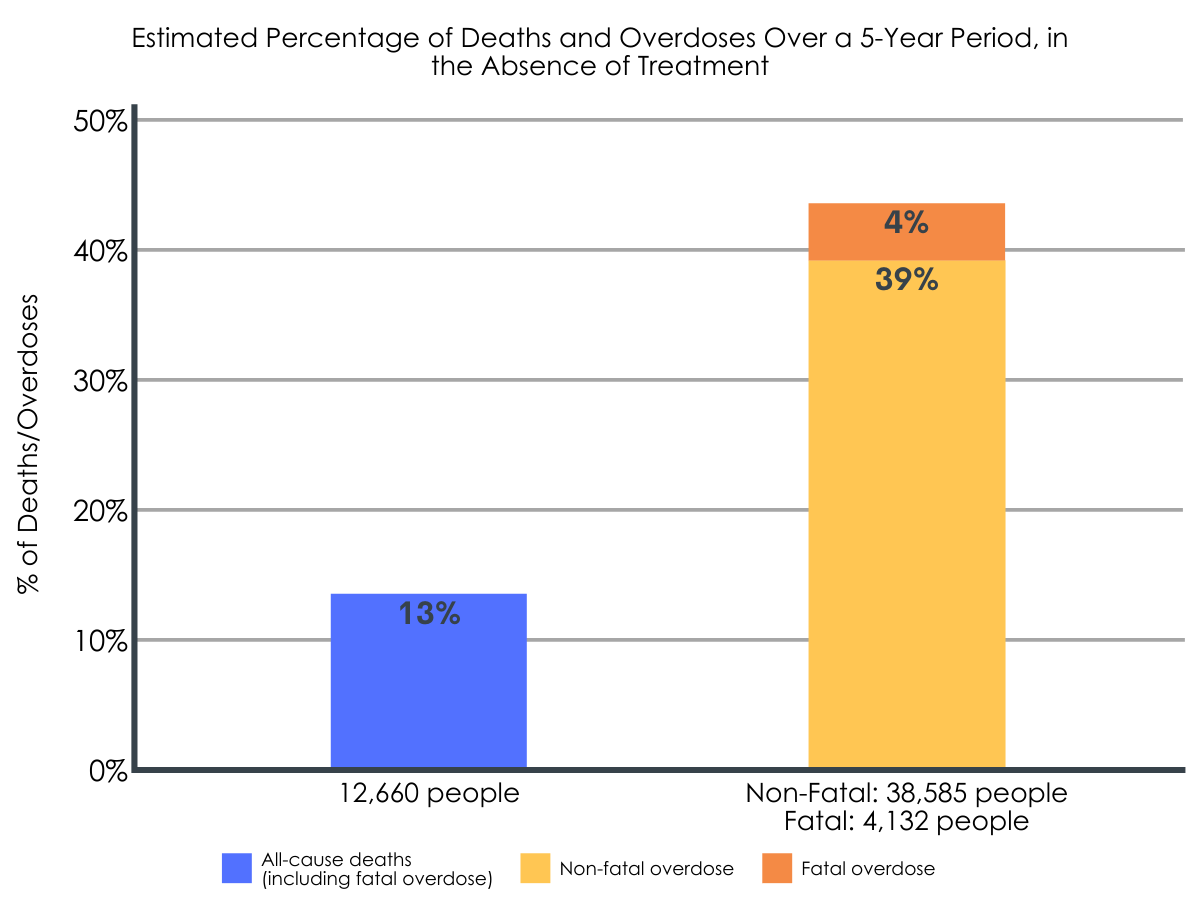
Figure 2.
Medication treatments, alone and combined with adjunct services, were associated with a lower rate of overdose when compared to no treatment.
Across all medications, the greatest reduction in overdose was seen when medication treatment was combined with contingency management, either alone or along with other add-on services (Figure below). The benefits of buprenorphine and extended release injectable naltrexone were almost identical. Smaller decreases in overdose were seen for methadone, but this was likely due to the increased risk of overdose during the early stages of induction.
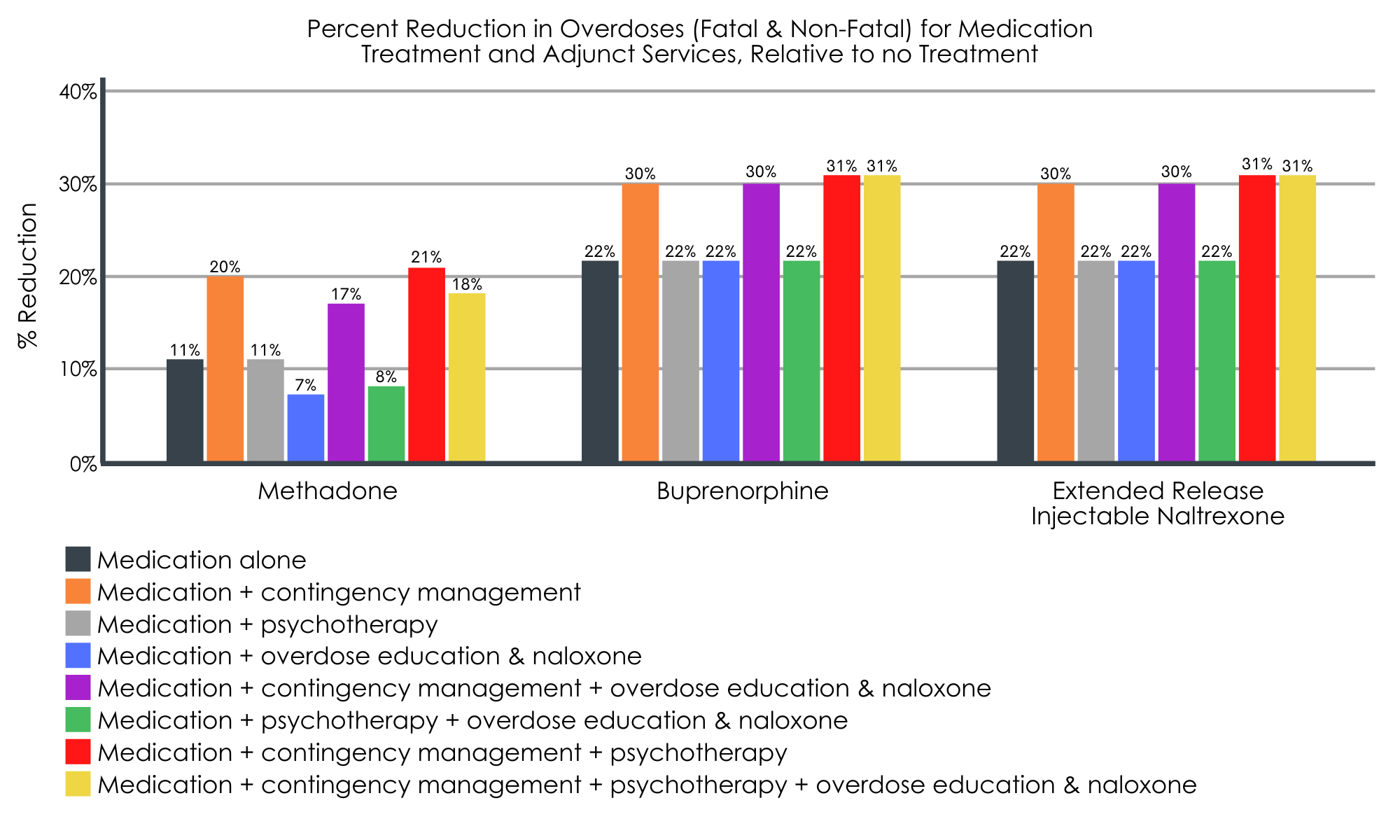
Figure 3.
Medication treatments, alone and combined with adjunct services, were associated with a lower prevalence of all-cause deaths (including fatal overdoses), relative to no treatment.
Across all medications, the greatest reductions in all-cause death were seen when medication treatment was combined with contingency management, with or without other add-on services (i.e., psychotherapy; overdose education and naloxone receipt). Again, the benefits of buprenorphine and extended release injectable naltrexone were almost identical. Smaller decreases in deaths seen for methadone were likely due to the higher risk of death associated with the first month of methadone treatment.
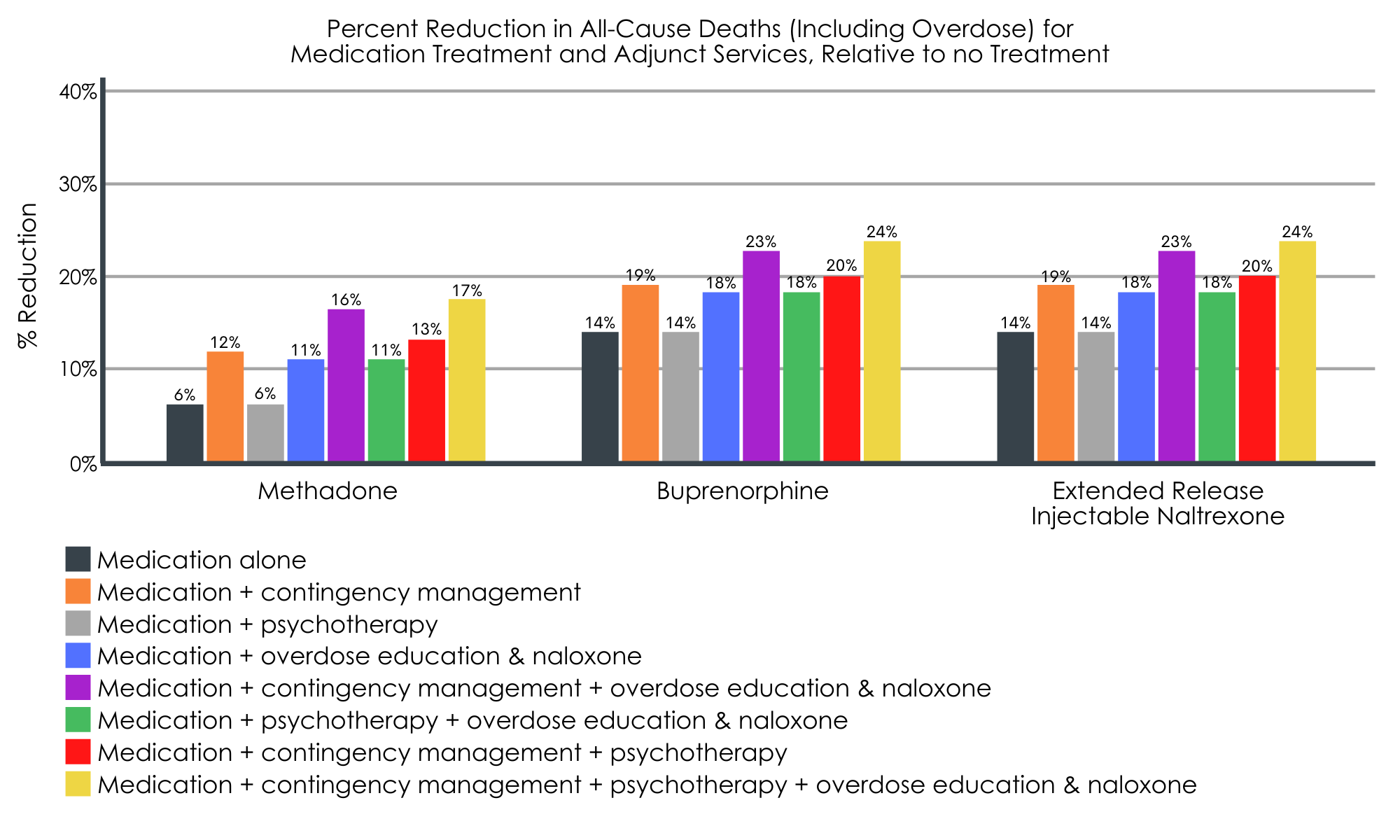
Figure 4.
Relative to no treatment (quality adjusted life years = 11.6), all medication treatments, alone and combined with adjunct services, were associated with gains in quality adjusted life years.
Across all medications, the greatest gains in quality adjusted life years were seen when medication treatment was combined with all three adjunct services (i.e., contingency management, psychotherapy, overdose education and naloxone receipt; gain of 1.7 years, from 11.6 to 13.3). In general, the benefits of Methadone, buprenorphine, and extended release injectable naltrexone were all equivalent.
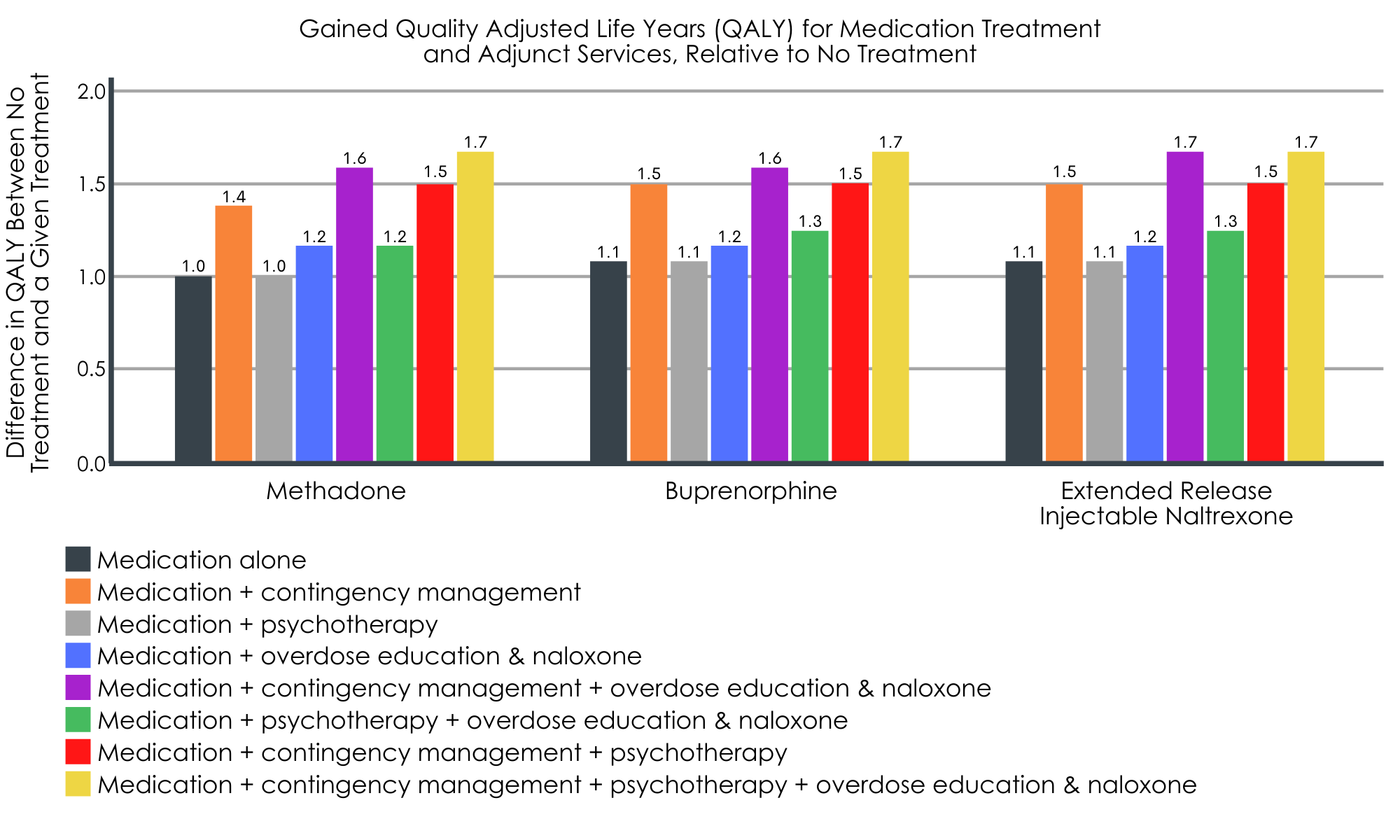
Figure 5.
Relative to no treatment (total lifetime healthcare & criminal justice costs per person = $613,000), all medication treatments, alone and combined with adjunct services, were associated with cost savings.
Across all medications, the greatest cost savings were seen when medication treatment was combined with contingency management (e.g., cost of contingency management plus: methadone = $508,000, buprenorphine = $536,000, extended release injectable naltrexone = $564,000). In general, methadone saved more money than buprenorphine, and buprenorphine saved more money than extended release injectable naltrexone.
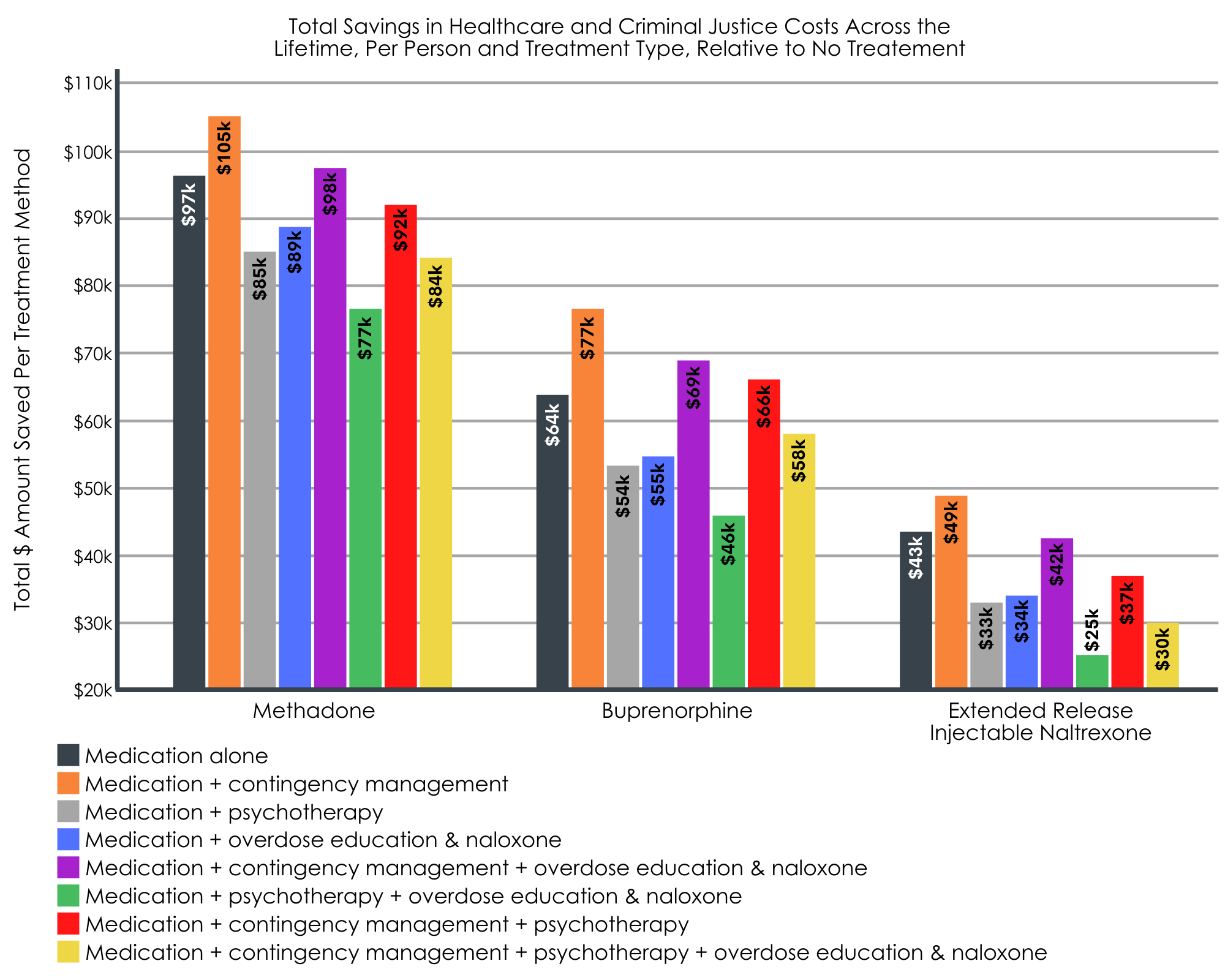
Figure 6.
All medications, with and without adjunct treatments, were more cost effective than no treatment.
When the authors considered total cost savings (healthcare & criminal justice costs) in the context of quality adjusted life years gained (i.e., cost effectiveness), all medications were cost effective. However, methadone plus contingency management emerged as the most cost-effective option relative to no treatment (i.e., saved $105,000 over one person’s lifetime and gained 1.4 quality adjusted life years above that of no treatment).
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Studies like this help us better identify cost-effective methods for enhancing standard medication treatments for opioid use disorder that improve patient outcomes. This study found that all medications, alone or in combination with adjunct services (contingency management, psychotherapy and/or overdose education plus naloxone), were associated with lower rates of overdose (fatal and non-fatal) and all-cause death compared to no treatment. All medications and their adjunct service combinations were also associated with cost savings ($25,000 – $105,000 saved) and gains in quality adjusted life years (1.0-1.7 years gained) relative to no treatment. Thus, providing medication in clinical settings appears to not only be essential for saving lives and reducing overdose rates, but also for saving money from a societal perspective. This is because individuals who do not receive treatment ultimately end up using more healthcare services (e.g., emergency department visits for overdose, primary care visits for comorbid health conditions, etc.) and are more likely to have repeat offences that result in criminal justice involvement (e.g., drug possession charges, incarceration).
With regard to overdose and all cause deaths, findings highlight the potential benefits of medication treatment combined with contingency management. Contingency management is shown to improve treatment retention and abstinence rates, and it therefore makes sense that it would help to lower rates of overdose and death, and increase quality adjusted life years. It may provide clearer benefit as a medication adjunct when individuals are not seen for structured, weekly medication management sessions or for patients with more psychosocial challenges. These data suggest contingency management is a cost-effective adjunct to medications for opioid use disorder, but there remain important barriers to its implementation that need addressing before it can be more widely used (e.g., concerns about its resemblance to gambling given chance elements to the rewards for abstinence).
Interestingly, adding overdose education and naloxone distribution did not seem to benefit overdose, but somewhat reduced all-cause deaths. This may be due to the fact that naloxone is meant to reverse an overdose (not prevent one) and education often involves information around the importance of using illicit opioids around another person who could administer naloxone in the event of an overdose. Thus, naloxone would not necessarily affect the occurrence of overdose events, but could save many lives in the event of an overdose where naloxone is used (i.e., by reversing it and preventing death).
Alternatively, psychotherapy did not reduce rates of overdose or all-cause death over and above medication. CBT is designed to help individuals actively cope with craving and relapse risk, targets also addressed by medication. Especially when medication is combined with medication management – which provides monitoring, support, and advice to engage with mutual-help groups – CBT may not provide added benefit. Like contingency management though, CBT and other adjunct interventions may be important add-ons for individuals who have more psychosocial challenges. Mutual-help groups and other community-based resources like recovery community centers may offer elements that complement medication, helping people to change their social networks for example. These can also provide natural social contingencies after the clinic based contingency management protocols end. Such community-based add-on services were not examined in this study.
When the researchers looked at cost savings and gains in quality adjusted life years, a similar pattern emerged. Medication treatment combined with contingency management alone or in addition to other adjunct services was associated with the greatest gains in quality adjusted life years and the largest savings across an individual’s lifetime. Therefore, combining medication and contingency management for opioid use disorder treatment appears to be a good option, not only for its cost savings but also its ability to enhance quality adjusted life years, and to lower risk of overdose.
- LIMITATIONS
-
- These analyses and models were simulated and based on available data or expert opinion. Therefore, outcomes are likely close-to but not an exact reflection of actual costs accrued by individuals and longitudinal studies with larger samples are needed to confirm these findings.
- Other versions of medication treatment, such as extended-release buprenorphine (i.e., Sublocade) were not assessed in this study and additional research is needed to determine its effects and cost-effectiveness when combined with add-on services.
- The benefits of medication may be underestimated here, as the researcher’s models did not account for incarceration (despite accounting for general criminal justice costs), treatment retention or outcomes based on treatment history, improvements in quality of life with sustained abstinence during treatment, or the reduced costs of health care and treatment discontinuation for patients on long-term medication treatment.
BOTTOM LINE
Studies like this help us better identify opioid use disorder treatments and their combinations that are the most effective and financially sustainable, which can ultimately inform policies and shed light on treatment combinations that are worth pursuing on a larger scale. This study found that, compared to no treatment, all medications were more cost-effective, increased quality adjusted life years, and resulted in fewer overdoses and all-cause deaths, regardless of whether they were administered alone or with adjunct services. Methadone emerged as the most cost-effective option, whereas buprenorphine and extended release injectable naltrexone showed the lowest rates of overdose and all-cause deaths (likely due to increased risk of overdose death during the early stages of methadone induction). Furthermore, adding contingency management to medication treatment may be particularly cost effective for improving quality adjusted life years and reducing overdose/death rates. Given the benefits of medication treatment and the mixed findings for add-on services, more research is needed to identify which treatment combinations are most beneficial and cost effective for different patients and to better understand how these combinations affect other outcomes, like patient well-being and long term recovery outcomes (sustained remission, substance use, recovery capital) at an individual and societal level.
- For individuals and families seeking recovery: Individuals who are receiving opioid use disorder medication treatment might benefit from add-on services like contingency management and overdose education plus naloxone, as it could reduce one’s risk for overdose and death, and increase their quality adjusted life years. Contingency management is not a widely offered treatment, so interested individuals should speak to their healthcare providers to learn more and find a program near them.
- For treatment professionals and treatment systems: Healthcare systems might consider providing contingency management with opioid use disorder medication treatment, as this appears to be a cost-effective option that can help prevent overdose/death and increase patients’ quality adjusted life years. Given that medication, alone or combined with adjunct services, is more cost effective and results in better outcomes than no treatment, it is essential that treatment systems offer opioid use disorder medication whenever possible.
- For scientists: Additional research is needed to determine the patient benefits and cost-effectiveness of concurrent opioid use disorder medication and adjunct services, including research using real-world data, aimed at identifying (1) effects other than overdose/death, (2) which patient sub-populations confer the greatest benefits from various treatment combinations and (3) the most cost-effective combinations across various healthcare settings.
- For policy makers: Medication treatments are cost-effective compared to no treatment, saving of $43,000 to $97,000 across a person’s lifetime. Adding contingency management to medication resulted in additional savings ($49,000 – $105,000) and gains in quality adjusted life years (.4 years gained vs. medication alone). Thus, contingency management is a potential cost-effective option for enhancing medication treatment and reducing opioid overdose rates in the US. Additional funding is needed to expand access to contingency management. Additional research funds will also help identify patients for whom this combination is most beneficial and cost effective.
CITATIONS
Fairley, M., Humphreys, K., Joyce, V. R., Bounthavong, M., Trafton, J., Combs, A., . . . & Owens, D. K. (2021). Cost-effectiveness of treatments for opioid use disorder. JAMA Psychiatry. DOI: 10.1001/jamapsychiatry.2021.0247

