Reminders and rewards both improve young adult treatment attendance, but a combination is best
Successfully engaging and retaining youth patients in substance use disorder treatment is a difficult endeavor. This study examined whether adding financial rewards and text messages – both individually and in combination – to traditional treatment help to improve treatment attendance and completion among youth in Denmark.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
A common hurdle for practitioners and families is successfully engaging youth in treatment so that they stay engaged until treatment completion. Health behavior change research suggests that one way to address this issue is to directly counteract potential barriers, for example, by including reminders to prevent forgetting appointments or to enhance motivation for treatment by offering incentives for attendance (also known as contingency management). This study examined whether the addition of vouchers and/or text messages to traditional substance use disorder treatment would improve treatment adherence and completion among youth in Denmark.
HOW WAS THIS STUDY CONDUCTED?
This study was a randomized clinical trial with 460 youth participants in Denmark across 9 municipal (i.e., county) outpatient treatment sites, all offering free outpatient treatment. Participants were assigned (using an alternative to true randomization called the minimization method) to 4 levels of active treatment that were meant to be completed during a 12-week period (once weekly sessions for 12 weeks).
All participants received standard outpatient counseling, which was a combination of cognitive behavioral therapy (CBT) and motivational enhancement therapy (MET). The first group only received this CBT/MET counseling and no additional services. A second group received vouchers in addition to the CBT/MET counseling. The vouchers were provided at every other session and valued at the equivalent of $30 USD; if a participant attended all 12 sessions, they would receive six vouchers ($180 total). Vouchers could be used for various items including movies, fast food restaurants or clothing stores. A third group received text message reminders in addition to the counseling. Each patient’s therapist sent a text message 1 day before their scheduled session. A fourth group received both text message reminders and vouchers in addition to the treatment. If a youth cancelled a session, they could reschedule it for a later date with no penalties, but if they did not show up for the session (“no-show”), they would lose that session’s ability to contribute toward their financial incentive. Participants were considered to have dropped out if they chose to discontinue the study or if they missed three consecutive sessions without cancelling them.
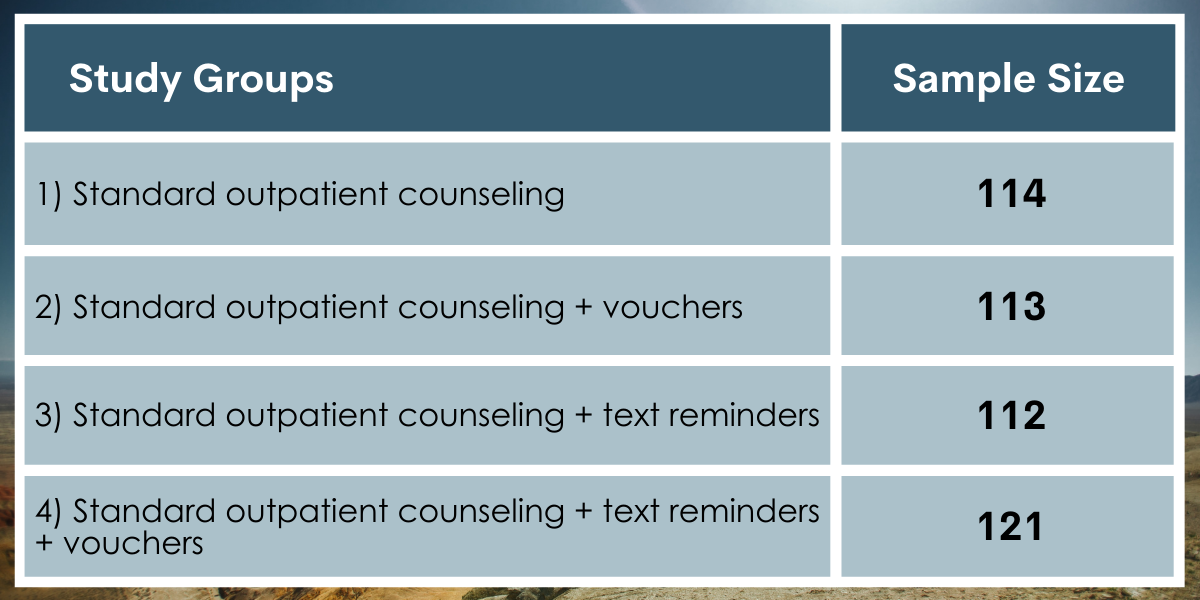
Figure 1.
The study collected a “YouthMap” questionnaire at the baseline visit. The YouthMap is a Danish assessment tool for youth in substance use disorder treatment that collects information about demographics, current substance use, past and present behavioral problems and mental illness, trauma, and peer and family relations. The study examined treatment attendance by analyzing the number of treatment sessions attended and the number of no-shows (without cancellation) and whether or not participants attended all 12 sessions (treatment completion).
This study’s sample was comprised of 460 youth (15-25 year olds) from 9 treatment centers in Denmark. Most of the sample was male (77%) and 18 years or older (87%). About half were enrolled in an education program and 12% were living with their parents.
WHAT DID THIS STUDY FIND?
More than one-third attended all 12 sessions.
More than one-third of participants (38%) attended all 12 sessions. Nearly 10% of the sample did not attend any treatment session after the first (baseline) session.
The group receiving both reminders and vouchers had the best treatment completion.
Individuals in the standard outpatient counseling + text message reminders + voucher group were most likely to complete treatment compared to every other group. This group was nearly twice as likely to complete treatment (49%) when compared to standard treatment without additional vouchers/reminders (25%) and fared better than either text message or vouchers alone (39% and 46%, respectively).
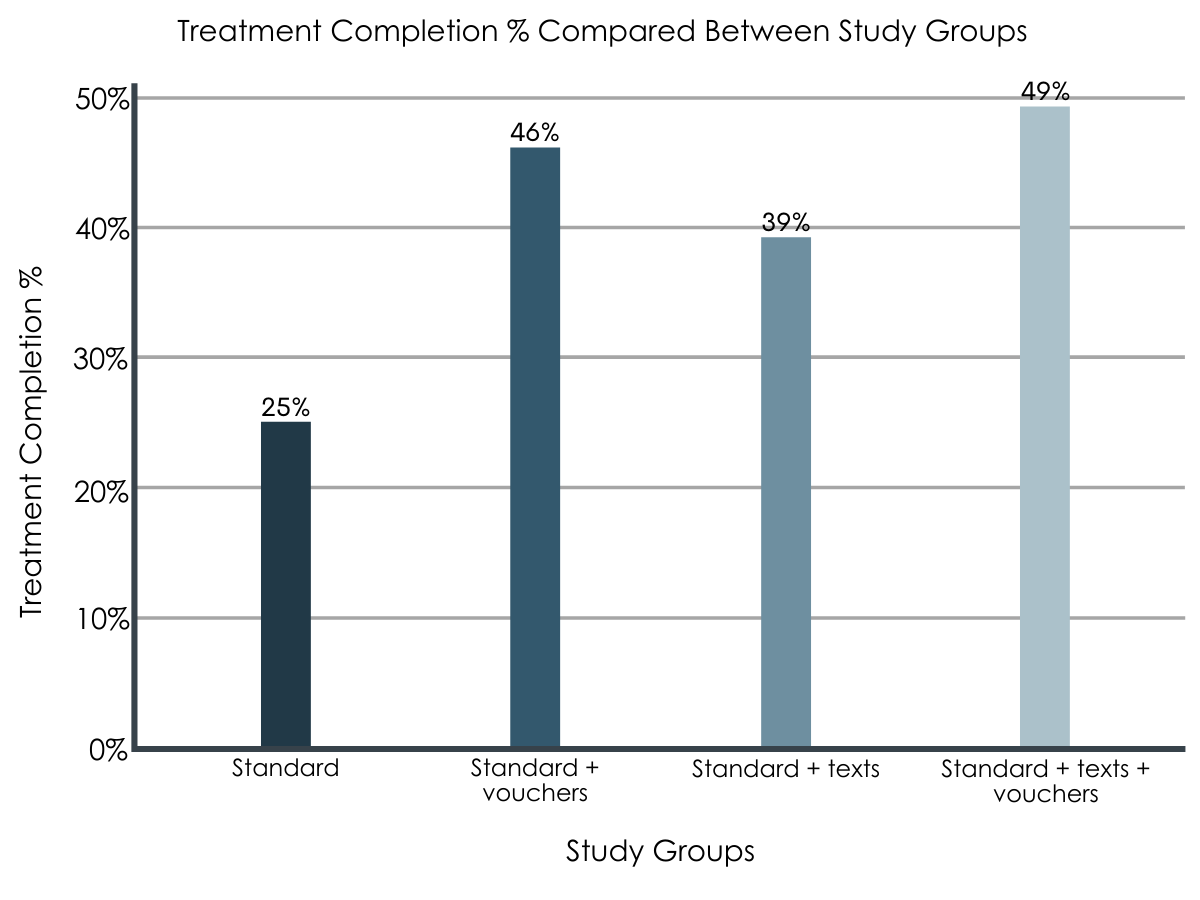
Figure 2.
Members of the lower intensity groups were most likely to miss an appointment without cancelling it (no-shows).
Participants in the standard outpatient counseling + text message reminders + voucher group were the least likely to miss an appointment without calling (“no-shows”) than both the standard outpatient counseling + text reminders or the standard outpatient counseling + vouchers groups. Participants in the standard outpatient counseling + text message reminders + voucher group were also least likely to have at least one no-show compared to the other groups.
Groups without text message reminders and vouchers were likely to drop out of treatment earlier.
Participants in the standard outpatient counseling group without any of the additional study features were more likely to drop out of treatment earlier than the other three conditions; their median time in treatment was 136 days compared to 168-194 days in the other conditions.
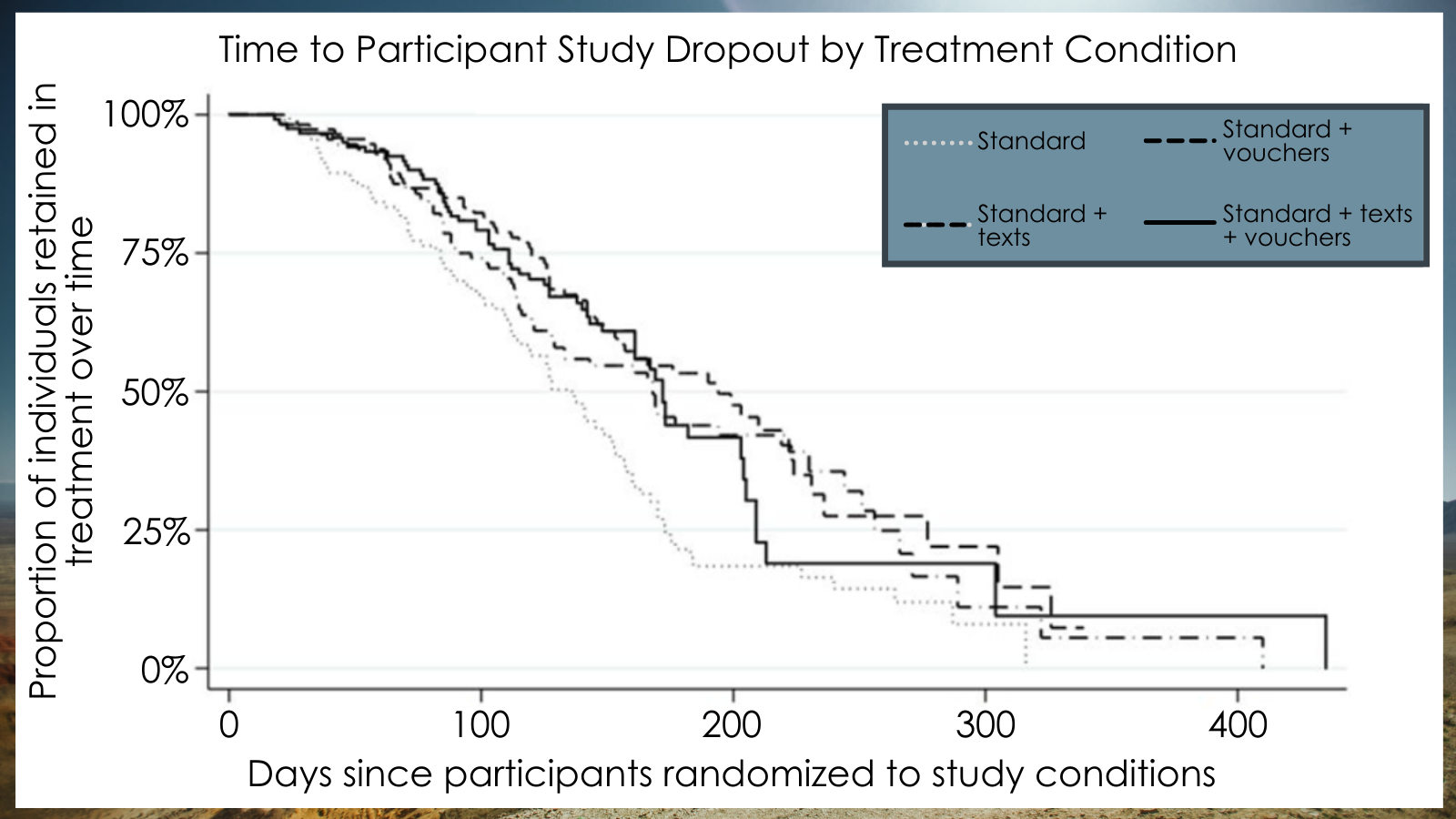
Figure 3. This figure uses what’s called a “survival estimate”; in this case, the lines illustrate how long a participant stays enrolled in treatment, that is, how long they “last in treatment” in each study condition. As time passes, the number of participants who remain in treatment goes down, represented by the percentages lowering. In a similar way to treatment completion, participants receiving both texts and vouchers in addition to standard treatment were less likely to drop out of treatment as the other groups. This figure was adapted from Figure 2, p. 7, in Pederson et al., 2021.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study examined the differential effectiveness of standard treatment and standard treatment with several small additions, such as text message reminders and/or vouchers and found that individuals in the groups with either of these additions had better outcomes in terms of treatment attendance and completion than individuals just receiving standard treatment; yet those with both additions to the standard of care did the best overall.
At the very least, this study provides additional support for introducing simple text message reminders to youth clients for all their treatment appointments to ensure treatment attendance and completion; text messages may also assist in other recovery-related behaviors. The exact mechanism the reminders serve is unclear and warrants future investigation. Because the text message reminders were sent from clinicians, in addition to serving as a behavioral reminder, they could also be viewed by participants as a positive relationship or connection with their clinician. These findings also suggest that the use of vouchers to improve treatment adherence may be a worthwhile approach, if there are funds to do so; notably, the modified approach used in this study (voucher provided every other session) was effective among youth indicating that vouchers may provide a high return on the investment.
However, the findings also raise questions about what treatment outcomes are important to focus on in youth treatment; that is, whether success is determined by the length of treatment or completion of treatment. In this study, the authors found that the majority of youth had treatment lasting longer than 12 weeks as a result of cancellations and rescheduling. Other research has suggested that keeping adolescents engaged for a longer period of time, as this study has done, results in better treatment outcomes; but as this study focused on treatment attendance and completion, they did not provide substance use related outcomes. As well, some research suggests that adolescents who have more days between a treatment session or who take longer to complete treatment have worse treatment outcomes than those who do not.
- LIMITATIONS
-
- The study had to pause participant enrollment several times during peak treatment periods to accommodate all clients. This action could have resulted in a biased sample of participants.
- There was some staff turnover during the study and this study was conducted across 9 treatment sites. Thus, there may have been differences between the staff or sites that were not accounted for in the analysis but that would be important to understanding the youth outcomes.
- Some clients allocated to the non-text message reminder groups could receive text message reminders if they asked, resulting in potential treatment contamination. According to the authors, however, few youths requested this accommodation.
- There may be specific characteristics of the Danish system, where public alcohol/drug treatment is free and must be initiated within 14 days of first contact, which might not translate to other contexts, such as the United States.
- There were several additional potential mediators of the treatment including contracts between clients and staff (signed treatment plans) and status letters (provided every 4 weeks) that could have influenced the success of treatment adherence and completion.
BOTTOM LINE
This study used a controlled intervention trial design and found that standard treatment that also included text message appointment reminders and vouchers increased youth treatment attendance and completion. That is, participants receiving both the reminders and the vouchers were nearly twice as likely to complete treatment as participants in the standard treatment condition. As well, participants in the standard treatment condition were likely to drop out much earlier than participants in the other conditions (by about 30 days), indicating that even the simple tool of text message reminders may be worthwhile to implement if contingency management approaches are not an option.
- For individuals and families seeking recovery: It is often difficult to make sure that youth attend and complete treatment, but this study offers some simple tools that may assist families with this process. First, discussing with youth potential barriers to treatment and ways they and/or the family can navigate them may help with treatment attendance. One such problem may be a simple one of forgetting a treatment appointment; asking for text message reminders could help to solve that problem and is easily implemented and non-invasive. Alternatively, if the treatment center does not provide reminders, individuals could program reminders into their phone or other electronic device. As well, identifying ways to increase motivation for treatment, or by initially providing motivation in the form of contingency management to create youth buy-in, may also help youth continue to attend treatment sessions.
- For treatment professionals and treatment systems: One simple solution to youth missing treatment appointments may be to implement a reminder system using the medium they are most comfortable with: text messages. It may also be necessary to ask them if they would like these reminders as this may not be something they would consider on their own. Working with patients to educate them on how to set up their own reminders (e.g., smartphone calendar apps) may also be a way to improve patient self-confidence and agency. In addition, identifying ways to increase motivation for treatment, or by initially providing motivation in the form of contingency management to create youth buy-in, may also help youth continue to attend treatment sessions. Working with parents to educate them on how they may help remove these barriers or increase youth motivation may also help engage youth in treatment.
- For scientists: Although this study highlights the potential of text message reminders and vouchers for treatment attendance and completion, future work should address substance use outcomes in addition to these clinical indicators of success as well as varying effectiveness for different types of substances. As well, future research which examines the exact mechanisms by which these tools operate, i.e., by examining different types of text messages and levels of vouchers or payment type or schedule may further identify specific pathways of how these treatment add-ons work to influence treatment success.
- For policy makers: Reducing barriers to substance use disorder treatment attendance is likely to result in better attendance and completion among youth, and ultimately, improved substance use outcomes. Policies that offer funding to enable treatment centers to provide reminders and rewards as well as education for parents in supporting their youth may yield improved benefits.
CITATIONS
Pedersen, M. U., Hesse, M., Thylstrup, B., Jones, S., Pedersen, M. M., & Frederiksen, K. S. (2020). Vouchers versus reminders to prevent dropout: Findings from the randomized youth drug abuse treatment project (youthDAT project). Drug and alcohol dependence, 218, 108363. Doi: 10.1016/j.drugalcdep.2020.108363

