Juice worth the squeeze? Cost-benefit analysis of contingency management
Contingency management strategies, such as providing rewards for maintaining abstinence measured by negative toxicology screens, are among the most empirically supported treatments for substance use disorders and stimulant use disorders, in particular. They also save money.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
While effective, little is known about whether this treatment is also cost-effective, producing a clinical benefit at a reasonable and feasible cost.
HOW WAS THIS STUDY CONDUCTED?
The current study was a secondary analysis of a randomized controlled trial in a community mental health center (see here). The study sought to determine the cost-effectiveness of adding contingency management to typical outpatient substance use disorder (“treatment-as-usual”) compared only to treatment-as-usual among 176 individuals with co-occurring stimulant use disorder and severe mental illness (either schizophrenia, schizoaffective disorder, biploar I or II disorders, and recurrent major depressive disorder).
The primary outcomes were group differences in health care dollars spent as a function of:
- quality adjusted life years (QALYs), a measure of the length of time lived at varying levels of health
- stimulant free years, measured by negative urine toxicology screens. Health care spending was measured by costs of the index treatment episode from the provider perspective (e.g., staff salaries and money needed for rewards for the CM intervention). Payer costs included spending needed for the index treatment episode as well as non-study outpatient mental health and substance use disorder (SUD) services, inpatient psychiatric and SUD treatment, and detoxification and emergency department visits. Outcomes were measured at the end of treatment (12 weeks after intake) and at 12-week follow-up (24 weeks after intake).
WHAT DID THIS STUDY FIND?
From the program perspective, providing contingency management did not increase program costs significantly ($62,670 vs. $60,018), but it did result in significantly more stimulant free years at end-treatment (0.85 versus 0.61).
Conclusions about total costs from the payer’s perspective were not possible because the variability in costs per person was rather large (standard error of $250,000 relative to costs of approximately $60,000 at end-treatment). Descriptively, however, costs for patients in the contingency management (CM) condition were about $2,500 more, on average, at end-treatment, and $125 less at 12-week follow-up. As with end of-treatment, those receiving CM had significantly more stimulant free years at 12-week follow-up.
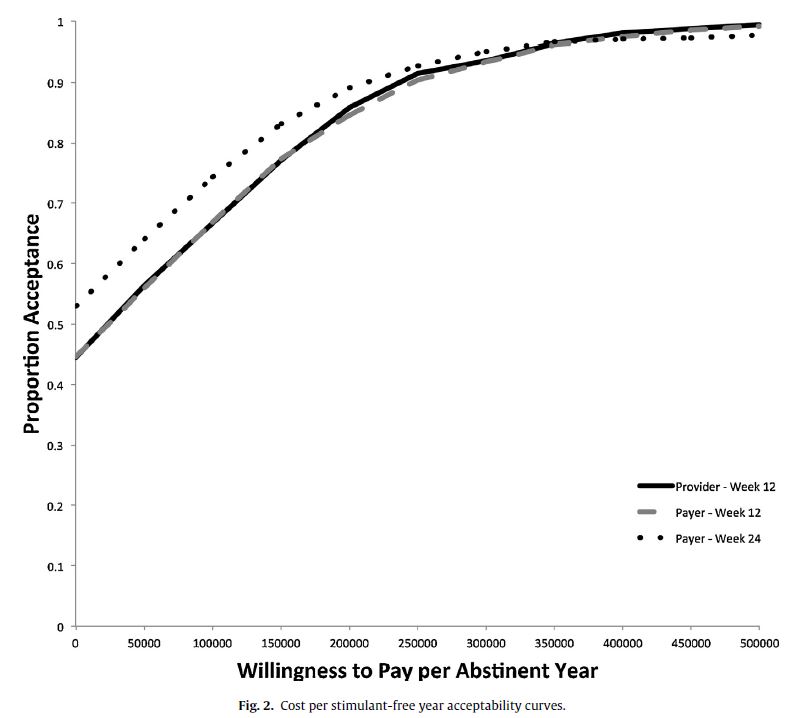
The cost-benefit analysis showed that at a willingness-to-pay threshold of $200,000 per stimulant-free year, contingency management when added to treatment-as-usual has an 85% chance of being deemed cost-effective (i.e., is “a good value”) at end-treatment for both the provider and payer, and 89% chance at 12-week follow-up for the payer. Whether or not patients received contingency management did not impact their quality adjusted life years (QALYs) at either end-treatment or 12-week follow-up.
This study suggests that contingency management may be a cost-effective clinical strategy to reduce stimulant use among individuals with stimulant use disorders and serious mental illness, a challenging population.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Contingency management may be a cost-effective way to boost substance use disorder outcomes in a community health center-based outpatient program.
Greater understanding of treatment cost-effectiveness can inform decision making regarding the adoption of these treatments for providers and regarding the reimbursement of these services for payers (e.g., insurance companies).
- LIMITATIONS
-
- Health care costs for non-psychiatric and substance use disorder (SUD) services were not included in the study’s analyses (e.g., visits to primary care doctors).
- Quality adjusted life years (QALYs)were based on a measure validated among patients with schizophrenia, though in the current study 61% had mental illness not on the schizophrenia spectrum. Since contingency management promoted more abstinence from stimulants and abstinence might positively impact patients’ quality of life, it might be expected that contingency management would also promote improved quality of life. However, this was not the case. One reason may be that 24 weeks (a 12-week treatment with 12-week follow-up) may not be enough time to parlay abstinence into improved quality of life in other areas.
NEXT STEPS
In light of its broad and supportive empirical base, the cost-effectiveness of contingency management should be tested across a range of settings, populations, and substance use disorders.
BOTTOM LINE
- For individuals and families seeking recovery: Contingency management can help improve recovery outcomes for individuals with stimulant use disorders and other psychiatric disorders.
- For scientists: Although more research is needed to establish the cost-effectiveness of contingency management (CM) and other substance use disorder (SUD) treatment approaches, this study suggests CM is a cost-efficient addition to SUD treatment and warrants similar studies across a range of settings, populations, and SUDs. Because the positive benefits of CM often decay with removal of the contingency, finding a way to keep some kind of contingency in place over the long term is likely to help prevent further use.
- For policy makers: Although more research is needed to establish the cost-effectiveness of contingency management (CM), this study suggests third-party payers should strongly consider reimbursement for costs of CM. Addition of this approach to standard, existing outpatient treatments may boost outcomes while costing about the same overall as treatment without CM.
- For treatment professionals and treatment systems: Although more research is needed to establish the cost-effectiveness of contingency management (CM), this study suggests treatment programs should strongly consider implementing CM. Addition of this approach to standard, existing outpatient treatments may boost outcomes without adding significant financial burden to program costs.
CITATIONS
Murphy, S. M., McDonell, M. G., McPherson, S., Srebnik, D., Angelo, F., Roll, J. M., & Ries, R. K. (2015). An economic evaluation of a contingency-management intervention for stimulant use among community mental health patients with serious mental illness. Drug Alcohol Depend. doi: 10.1016/j.drugalcdep.2015.05.004

