Strength in numbers: Brief, group-delivered motivational interviewing shows promise among veterans in outpatient substance use disorder treatment
Motivational interviewing is an effective intervention to promote behavior change and help individuals reach their substance use goals. Research examining the effectiveness of motivational interviewing delivered via group therapy, a popular addiction format, could improve the reach and accessibility of this empirically-supported approach. In this study, researchers developed a 4-session, group-delivered motivational interviewing intervention for veterans who also had co-occurring psychiatric disorders and found that it outperformed their active treatment comparison on measures of alcohol use and treatment attendance.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Motivational interviewing is an evidence-based treatment for substance use disorder but has been understudied as a group-delivered intervention, and among veterans with co-occurring psychiatric disorders, or as a clinician-delivered intervention in the context of real-world clinical practice. Developing and testing group-based treatments may be especially useful to informing addiction treatment best practices, given how commonly addiction treatment programs use group formats to deliver services. Also, individuals with co-occurring substance use and psychiatric disorders, especially those with more psychosocial challenges (e.g., more mental health difficulties, worse functioning, etc.), may also benefit from treatments that can integrate both substance use and mental health goals, yoking individuals’ motivation for substance use change to their mental health concerns. Researchers developed a brief, 4-session motivational interviewing intervention for veterans with co-occurring substance use and psychiatric disorders that they delivered in an outpatient group format. The researchers not only describe the process of their real-world implementation strategy, but they also evaluate clinicians’ fidelity to the protocol and motivational interviewing principles and provide 1- and 3-month outcome data to highlight improved substance use outcomes as well as treatment and mutual-help attendance and mutual-help participation following the intervention.
HOW WAS THIS STUDY CONDUCTED?
The researchers conducted a randomized controlled trial to evaluate the effectiveness of their group-delivered motivational interviewing intervention, as implemented within a VA outpatient clinic under real-world conditions and compared outcomes to an active treatment control condition. The researchers included 118 veterans with substance use disorder in their study. Recruitment took place between May 2010 and November 2012. Inclusion criteria specified that participants have an active substance use disorder in their medical record and report use of substances within the last 30 days. Participants’ charts were also reviewed for evidence of co-occurring psychiatric disorders, and researchers also performed diagnostic interviewing to supplement data regarding substance use disorder status (Structured Clinical Interview for DSM-IV) and other co-occurring psychiatric diagnoses at baseline (MINI-International Neuropsychiatric Interview).
Participants began their assigned intervention an average of one week after study enrollment and baseline assessment. The intervention lasted 4 sessions carried out over 4 consecutive days. Participants then completed follow up self-report treatment attendance and substance use measures at 1 and 3 month follow up, as well as corroborating breathalyzers and urine toxicology screens. The primary outcomes of the study were treatment session and 12-step mutual-help group attendance and alcohol use, as measured by alcohol using days, binge drinking days, and standard drinks consumed at 1- and 3-month follow-up. The researchers secondarily examined use of illicit drugs at 1 and 3 months and evaluated the fidelity of clinicians’ delivery of both the group-based motivational interviewing intervention and the active control treatment.
The primary intervention tested was a group-delivered and manualized treatment, consisting of 4 group sessions, and based on motivational interviewing. The goal of the treatment is to engage patients in a collaborative conversation, focused on substance use and behavior change, to evoke change talk, reduce ambivalence about change, and to initiate plans to reduce or abstain from substance use. This manualized treatment was developed to be inclusive of and effectively target co-occurring psychiatric disorders as well. The comparison treatment, like the motivational interviewing intervention, was also an active treatment condition that was designed also to be therapeutic for patients and thus not easy to beat. In fact, this comparison treatment included cognitive behavioral therapy/relapse prevention, 12-step facilitation, and psychoeducation. Both treatments were delivered upon entry into outpatient care at a VA clinic, and were provided by clinic staff.
The study included 118 veterans, evenly split across treatment conditions. Just over half of the sample was black (58%), and a substantial minority were white (41%), with a very small number of “other” (<1%). The average participant was over 50 years old and a substantial majority were male (92%). Two-thirds overall had annual incomes below $20,000. Every participant had an alcohol use disorder and nearly 41% had a co-occurring drug use disorder, the most common of which were cocaine and cannabis use disorder. Of note, one individual in the motivational interviewing condition, and three in the active comparison group had an opioid use disorder. Overall, 87% had a current co-occurring psychiatric disorder, the most common of which were depressive and anxiety disorders. Of note very few (e.g., two in the motivational interviewing condition) were diagnosed with a psychotic disorder like schizophrenia.
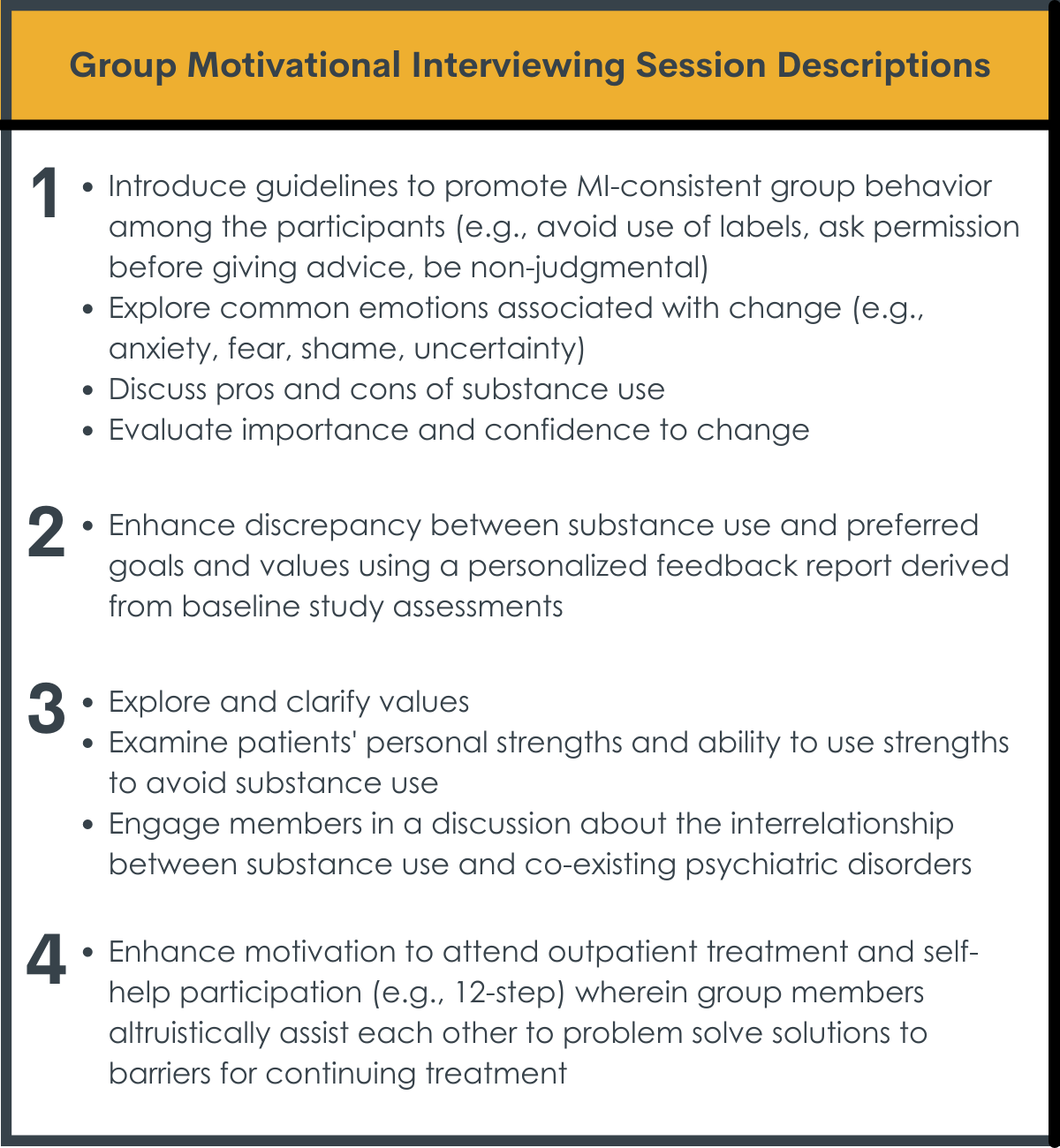
Group motivational interviewing session descriptions.
WHAT DID THIS STUDY FIND?
Group-delivered motivational interviewing outperformed active control condition.
The researchers found that group-delivered motivational interviewing outperformed the active treatment control condition on measures of binge drinking at 1- and 3-month follow up, and the number of drinking days, standard drinks consumed, treatment sessions attended, and 12-step groups attended at 3-month follow up. Participants in both groups improved on drug use outcomes, with no differences between treatments. Interestingly, the researchers found that participants’ self-reported substance use results were consistent with their urinalysis and breathalyzer results, with the exception of 5 faulty urinalyses resulting in false negatives, meaning the individual reporting substance use that was not detected by the drug screen.
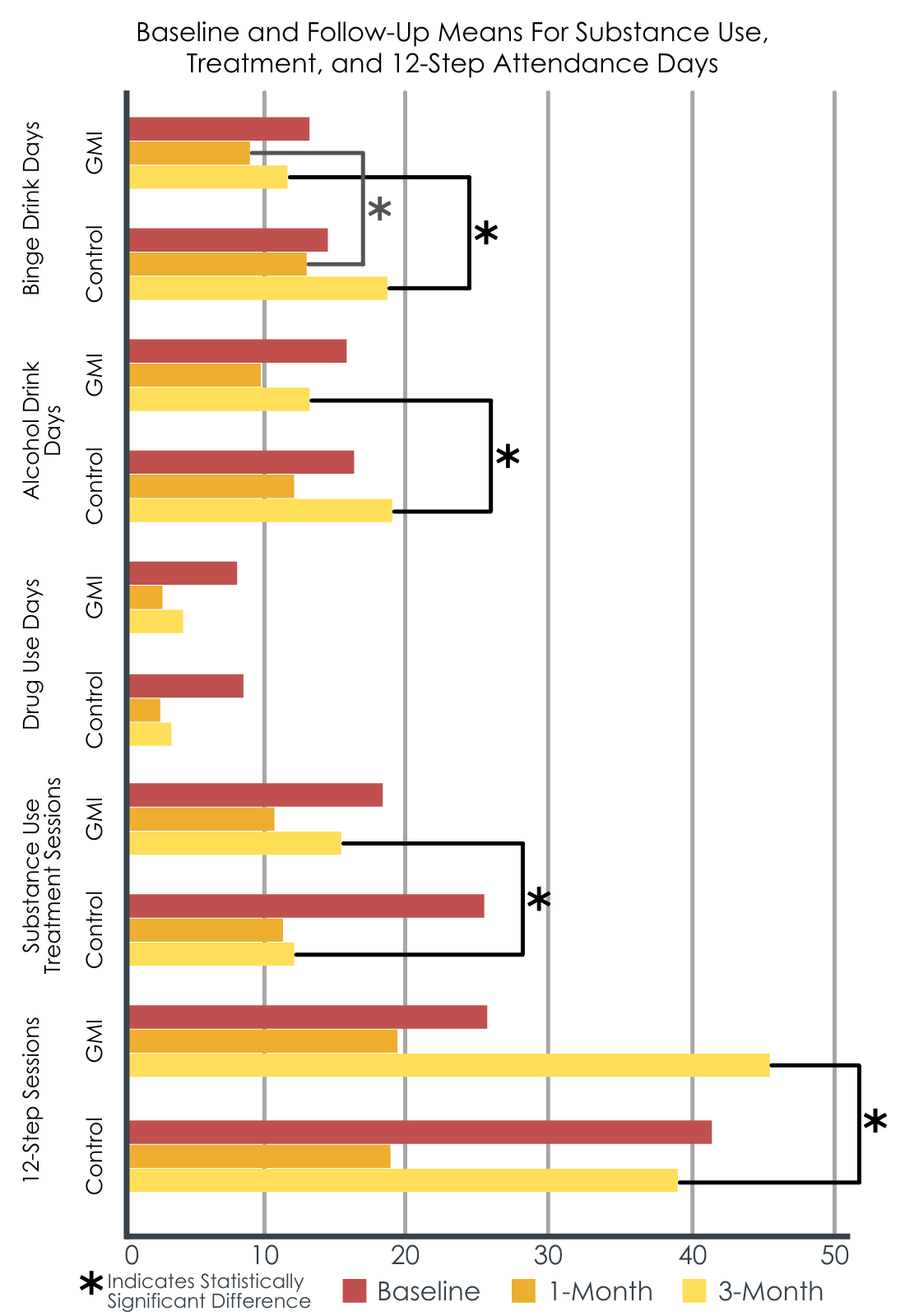
Baseline and follow-up means for substance use, treatment, and 12-step attendance days.
Session attendance was similar between groups.
The researchers did not find that the number of assigned treatment sessions attended differed between groups, nor the proportion of participants completing their assigned treatment.
Group-delivered motivational interviewing was delivered with high fidelity.
The researchers conducted fidelity ratings of the clinicians delivering both treatments and found that fidelity ratings were higher and delivery more consistent among the trained clinicians providing group-based motivational interviewing than the active comparison.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Motivational interviewing is a versatile treatment, often individually delivered, that promotes treatment engagement and improved substance use often as well as, but no better than, other active interventions. This study is among the few to evaluate a group-delivered motivational interviewing intervention, which has the potential to expand the reach of motivational interviewing to a larger number of patients without necessarily increasing clinician or administrative burden. They found individuals receiving group motivational interviewing, on average, had better treatment and mutual-help attendance, as well as improved alcohol use – but not other drug use – outcomes in the short-term. It is possible that the motivational interviewing intervention was more effective because it was better at getting people to engage with services than the comparison treatment, though this cannot be determined from the study summarize here and should be tested in future work. Interestingly, these findings run contrary to studies where more directive 12-step facilitation outperformed motivational interviewing-based 12-step facilitation and where motivational interviewing did no better than direct brief advice to attend groups. It is possible that motivational approaches could work better to promote 12-step mutual-help when delivered in group formats (where experienced members might help promote motivation to attend for those with less experience). This possibility explaining the findings here and why they differ from other similar work needs to be tested empirically. It should be remembered also that this group of VA patients studied also had additional concurrent psychiatric disorders and this style of intervention may work particularly well for this type of comorbid patient. It may also be true that the effectiveness of group-delivered motivational interviewing in this study, relative to individually-delivered motivational interviewing, is accounted for by synergistic group member influences, such as social support and vicarious learning.
It is important to note that researchers evaluated the effectiveness of group-delivered motivational interviewing, as delivered in a real-world VA outpatient clinic, and compared to an active control condition that included evidence-based cognitive-behavioral and relapse prevention interventions. Finding benefits related to this group-delivered motivational interviewing when measured against such a high-bar intervention as the researchers did in this study, further supports its potential utility.
Importantly, as alluded to above, these researchers conducted their study with a sample of veterans, the majority of whom met criteria for co-occurring drug use disorder, in addition to alcohol use disorder, as well as other psychiatric diagnoses. As such, the outcomes of this study may be more generalizable to patients in the real-world, and more inclusive to a broad range of psychiatric distress and impairment.
The researchers observed a high level of fidelity among the clinicians trained to provide group-delivered motivational interviewing, which also supports the effectiveness of their clinician training procedures. The group-based delivery and brief 4-session/4-day day delivery format support the feasibility of group-based motivational interviewing in real-world clinics.
- LIMITATIONS
-
- The study was conducted using an entirely veteran-based sample. While veterans and non-veterans with substance use disorder share many of the same concerns, there may be distinguishing characteristics that limit generalizability of the current results to non-veteran or non-VA treatment seeking individuals.
- The sample was nearly all male. Different results may occur among women veterans and should be studied.
- The sample was roughly half black and half white, which was a strength, but it is unclear the extent to which findings may generalize to other populations with different racial/ethnic compositions.
- The researchers’ heavily reliance on veterans’ electronic health record data for information regarding co-occurring psychiatric disorders could have been limited as well, as some diagnoses might not be recorded, others may have been recorded but remain unclear how accurately and systematically they were derived, and others might be outdated.
BOTTOM LINE
Group-delivered motivational interviewing appeared to be feasible to be delivered within a real-world VA substance use outpatient clinic with high fidelity. After comparing group-delivered motivational interviewing to a strong active control treatment that included several known evidence-based interventions (e.g., cognitive behavioral interventions and relapse prevention), the researchers found that their intervention outperformed the control condition on several measures of alcohol use, outpatient treatment engagement, and mutual help group attendance over 3 months.
- For individuals and families seeking recovery: Motivational interviewing is a strategy for promoting motivation for behavior change and recovery among individuals with substance use concerns, and can provide an excellent jump-start to treatment. The outcomes of this study were promising and suggest that group-based motivational interviewing might be a useful treatment to consider for individuals concerned about their substance use, or those who are beginning to contemplate reducing or abstaining from substance use altogether.
- For treatment professionals and treatment systems: The fact that participants who received group-delivered motivational interviewing also evidenced greater total outpatient session attendance and mutual help group attendance speaks to its potential to support recovery both directly through the observed alcohol use improvements, and indirectly through increased treatment and mutual help group engagement. Further, while these findings need to be replicated in other samples, the results of this study support the implementation of brief, 4-session, group-based motivational interviewing within the first week of outpatient treatment and demonstrates its potential to facilitate positive treatment outcomes. The brief format, delivered consecutively over 4 days, could help jump-start treatment in the early stages, and may be a feasible and cost-effective alternative to individually-based care.
- For scientists: These researchers observed significant improvements regarding alcohol consumption, outpatient session attendance, and mutual help group attendance among participants who received group-delivered motivational interviewing, with effect sizes ranging from small to medium. These findings are noteworthy given the fact that the study was conducted in a real-world clinic and delivered by staff clinicians, and that the motivational interviewing intervention was compared to a strong active control group that included evidence-base intervention as well. While the outcomes observed extended to the 1- and 3-month follow up assessments, follow up research that extends the observation period to at least 6 months or longer would provide novel insight into the duration the observed treatment effects. It might also be beneficial to consider other settings in which this intervention might be effective, such as inpatient detoxification units or residential treatment clinics, given the ongoing need for interventions that quickly target and improve substance use outcomes and treatment engagement.
- For policy makers: Brief therapies that can be implemented in a variety of clinics and under varying circumstances, such as the brief group-delivered motivational interviewing treatment evaluated here are particularly promising. The finding that group-delivered motivational interviewing was not only associated with improved substance use outcomes but also treatment engagement is significant as well, particularly as a means to address high rates of dropout from substance use disorder clinics. Given the ongoing need for novel intervention strategies that more quickly and effectively improve substance use outcomes and treatment engagement among individuals with substance use disorder, it is recommended that stakeholders support replication and extension of similar research, and prioritize novel implementation in novel settings to further extend the reach of group-delivered motivational interviewing.
CITATIONS
Santa Ana, E. J., LaRowe, S. D., Gebregziabher, M., Morgan-Lopez, A. A., Lamb, K., Beavis, K. A., . . . & Martino, S. (2021). Randomized controlled trial of group motivational interviewing for veterans with substance use disorders. Drug and Alcohol Dependence, 223, 108716. DOI: 10.1016/j.drugalcdep.2021.108716

