Impact of Motivation on Alcohol Treatment Outcomes
In substance use disorder treatment, there are key thoughts, feelings, and behaviors that warrant more attention than others, because research has shown that an increase (or decrease) in these variables predict increased likelihood of abstinence and addiction remission.
Among the most important is motivation, or readiness, to change one’s drinking, including both abstinence and low-risk drinking (sometimes called “harm reduction” or “moderation”).
WHAT PROBLEM DOES THIS STUDY ADDRESS?
There are dozens of studies showing the degree to which someone is motivated to change their drinking and other drug use upon entering treatment provides key information regarding how well they will engage with treatment, and how good their outcomes will be.
Although it is assumed that pre-treatment motivation ultimately impacts post-treatment motivation, and this post-treatment motivation influences later outcomes, research investigating the effect of post-treatment motivation on longer-term treatment outcomes (i.e., several months after treatment has ended) is less common than research on pre-treatment motivation.
Few studies that investigate what processes during treatment help explain this relationship between pre-treatment motivation, post-treatment motivation, and treatment outcomes.
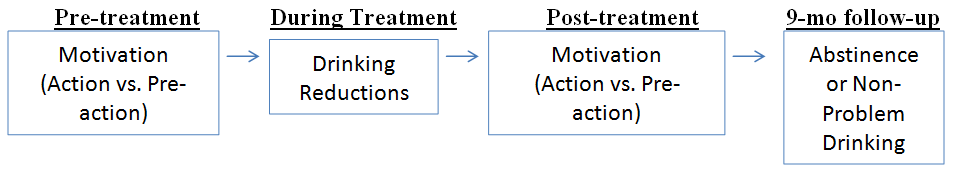
In this study, Cook, Heather, and McCambridge, analyzed whether motivation impacts outcomes through their hypothesized model (pre-treatment motivation to during-treatment improvement to post-treatment motivation to longer-term improvement; see figure below).
HOW WAS THIS STUDY CONDUCTED?
Cook and colleagues conducted a secondary data analysis of the United Kingdom Alcohol Treatment Trial (UKATT), a multi-site randomized controlled trial, which showed that motivational enhancement therapy (MET) – the primary goal of which is to resolve individuals’ ambivalence about change – and social behavior and network therapy (SBNT), which includes an individual’s close family and/or friends in treatment to increase social support for abstinence, had similar alcohol outcomes.
The authors performed structural equation modeling using data from the UKATT study, a technique that provides insight into the pathways from a predictor variable (e.g., motivation for reducing or quitting drinking at pre-treatment) to an outcome (e.g., abstinence).
The study authors hypothesized, specifically, that the influence of pre-treatment motivation on alcohol outcomes at 9-month follow-up would occur first through reductions in drinking during treatment, and then increased motivation measured at the end of treatment.
They focused on 5 outcomes in 392 individuals with primary alcohol use disorder:
- Abstinence or drinking but with zero alcohol problems, measured by the Alcohol Problems Questionnaire (yes/no)
- Abstinence or drinking but with at least 2/3 reduction in alcohol problems (yes/no)
- Abstinence or drinking but with at least 1/3 reduction in alcohol problems (yes/no)
- Drinks per drinking day (DDD)
- Percent days abstinent (PDA)
They measured motivation with the 12 question Readiness to Change Questionnaire.
Authors used the information from this questionnaire to categorize individuals into different stages of change/motivation;
one stage, for instance, was the “action stage”, meaning they were currently making changes to support reduced drinking or abstinence, or “preaction” (either “contemplative” or “precontemplative”), meaning they were thinking about change or not sure they had a problem worth changing.
In the analyses the authors controlled statistically for pre-treatment levels of drinking severity, drinking-related problems, and demographic characteristics (e.g., age, gender, and education), as well as the site at which individuals received the treatment as part of the multisite study.
WHAT DID THIS STUDY FIND?
For each of the first three outcomes listed above:
- Abstinence or drinking but with zero alcohol problems, measured by the Alcohol Problems Questionnaire (yes/no)
- Abstinence or drinking but with at least 2/3 reduction in alcohol problems (yes/no)
- Abstinence or drinking but with at least 1/3 reduction in alcohol problems (yes/no)
Researchers found that there was no effect of pre-treatment motivation on 9-month alcohol outcomes using their structural equation model.
There was an effect of post-treatment motivation on alcohol outcomes; and an effect of pre-treatment motivation on drinking during treatment, which, in turn, was associated with post-treatment motivation. Specifically, individuals in the action stage at post-treatment were about 3 times more likely to be abstinent or drinking with no problems.
Cook and colleagues’ study adds to research showing that discharge motivation to reduce or quit drinking (or continue meeting these goals if already doing so) is important in predicting positive treatment outcome.
In another study of 18-24 year olds in residential treatment, for example, both abstinence motivation at discharge, and one’s increase in abstinence motivation during treatment, predicted total abstinence 3 months after discharge (see here).
One new and interesting finding authors highlight is that, at least for outpatients, a treatment that helps a person increase their social network support for abstinence, like social behavior and network therapy (SBNT), could be a more effective way to increase motivation to change than one that simply discusses motivation from the perspective of thoughts and feelings, like motivational enhancement therapy (MET).
One speculation based on social-cognitive theory is that social support increases motivation through positive social responses to abstinence and recovery behaviors (e.g., social reinforcement).
WHY IS THIS STUDY IMPORTANT
This study builds on research investigating the impact of motivation on treatment outcomes, to look specifically at the pathway through which it has impact.
This type of information will help inform treatment providers and programs about how best to target motivation, because pre-treatment motivation – which has been analyzed more often than motivation during and after treatment – is an individual factor that, by definition, cannot be influenced by treatment.
There are a range of studies showing that therapies that help modify patients’ social networks promote better abstinence rates, such as “network support”, which, unlike social behavior and network therapy (SBNT), explicitly encouraged attendance at 12-step mutual-help meetings to facilitate these network changes
- LIMITATIONS
-
- One important limitation is that the study sample of 392 only included individuals that attended at least 1 treatment session in the randomized controlled trial and who also completed pre-treatment, post-treatment, and 9-month follow-up; these individuals were more educated and were less severe and problematic drinkers at baseline than the original randomized controlled trial sample of 742. This may be one reason why researchers found an advantage for social behavior and network therapy (SBNT) (i.e., it works better than MET in patients with less severe problems) even though the treatments had similar outcomes in the main randomized controlled trial with the full sample. Therefore, caution should be taken in applying these results to all individuals with alcohol use disorder (AUD).
NEXT STEPS
One possible next step would be to investigate further why there was an advantage for social behavior and network therapy (SBNT) in this study, but not the main randomized controlled trial, because of the important implications for treatment programs and recovery support services.
BOTTOM LINE
- For individuals & families seeking recovery: For those with an alcohol use disorder considering or seeking treatment, motivation to change alcohol consumption when you enter treatment seems not to matter as much as your motivation to change drinking at treatment completion. Consider working with a therapist on what life changes or treatment strategies would help increase motivation for abstinence or lower-risk drinking.
- For scientists: Structural equation modeling provided a solid analytic framework to investigate how, and through what processes, motivation measured at different time points influences better treatment outcomes. One limitation was that the sub-sample analyzed had lower alcohol severity and fewer problems than the full sample, suggesting more research is needed to test this model in other samples with more severe problems, and for individuals with other substance use disorders (SUDs) or addictions in addition to alcohol use disorder (AUD).
- For policy makers: This study provided more fine grained information about what thoughts, feelings, and behaviors programs might target explicitly during treatment for individuals with alcohol use disorder. Strongly consider continued funding for research on mechanisms of behavior change in alcohol and other drug treatment.
- For treatment professionals and treatment systems: Early gains in treatment are important in helping patients increase their motivation for abstinence or lower-risk drinking, which in turn, predicts better treatment outcomes. Thorough assessments and treatment plans that attend to patients’ individuals life contexts (e.g., the degree of social support they have for drinking versus social support for abstinence when they enter treatment) as soon as feasible may help with these gains during treatment, which appear to be key in ultimately promoting better outcomes.
CITATIONS
Cook, S., Heather, N., & McCambridge, J. (2015). Posttreatment motivation and alcohol treatment outcome 9 months later: findings from structural equation modeling. J Consult Clin Psychol, 83(1), 232-237. doi: 10.1037/a0037981

