Using peer outreach to actively link individuals to treatment with opioid use disorder medications
Medication for opioid use disorders (OUD) can be lifesaving, yet only some people with OUD receive these medications. One reason is that it can be difficult for individuals with OUD to access and remain engaged with medication-based treatments. In this study, researchers investigated the feasibility and initial results of using peer outreach workers to help connect individuals to treatment with OUD medications.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Medication for opioid use disorders (OUD), including the agonists methadone and buprenorphine (often prescribed in combination with naloxone, known by the brand name Suboxone), as well as the antagonist naltrexone, are empirically supported and often life-saving medications for individuals with OUD. Yet, fewer than 20% of people with OUD received one of these medications in the past year. Common reasons for not seeking treatment for substance-related problems include not knowing where or how to access treatment, not being ready for treatment, and not being able to afford treatment. Additional barriers may exist for medications for OUD specifically, such as negative attitudes about using another opioid (in the case of methadone or buprenorphine) to treat an opioid addiction. Even if individuals are able to access medications for OUD, retention in treatment remains a challenge, with many patients dropping out of treatment after just a few months. There is a need to develop innovative strategies that engage and retain individuals in medication treatment for OUD. This study examined the feasibility and initial outcomes of a peer outreach and treatment linkage intervention for individuals with OUD and explored predictors of successful engagement and retention in treatment.
HOW WAS THIS STUDY CONDUCTED?
This study was conducted in communities in Chicago, IL, that had high rates of opioid overdose deaths. In this study, the research team followed individuals through several phases of outreach and treatment. These included:
- Outreach: A team of trained peer outreach workers, who were individuals in sustained remission from substance use disorders (SUD), went to places in the community where individuals at high-risk for substance use problems were likely to be (for example, liquor stores, mini-marts, public transportation stations). Outreach workers introduced themselves to people and asked if they knew anyone who might be interested in treatment for heroin or opioid addiction. If individuals were interested, the outreach worker connected them by phone to project staff for a phone screen. If they knew someone who was interested, they were given a flyer with contact information for the project.
- Linkage Meeting: Individuals who were eligible (lived in the area, currently using heroin or other opioids, not currently in SUD treatment) were given transportation to the project office for a treatment linkage meeting. In the meeting, the linkage manager explored benefits of treatment, resolved barriers to treatment, and connected the individual to treatment (usually detoxification services or medication for OUD). Transportation to further treatment was provided and the linkage manager stayed in touch weekly with the participant.
- Medication Assisted Treatment (MAT): Participants who were interested were connected to medication-based treatments for OUD, with most (95%) receiving methadone and the remainder (5%) receiving naltrexone or buprenorphine. Participants were followed for 30 days after their intake into a treatment program.
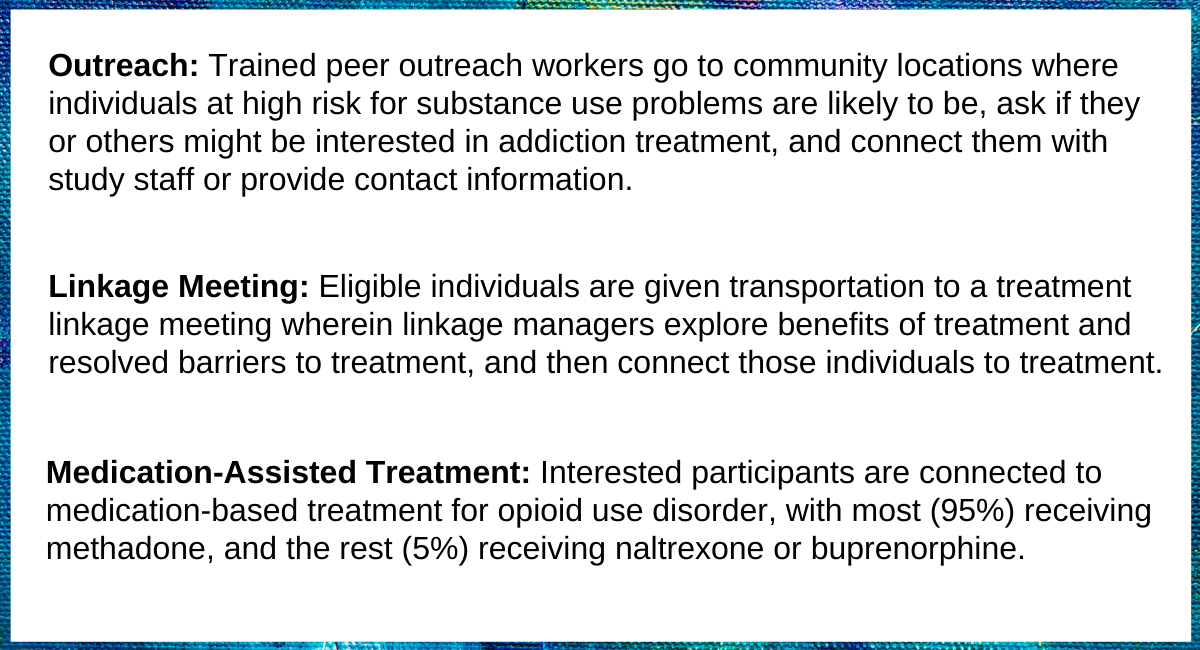
Figure 1.
Participants included 3308 individuals who were eligible at the outreach phase and 1638 who agreed to participate in the linkage meeting. Of those who agreed to participate in the linkage meeting, 27% were female, 85% were African American, and most were between the ages of 40 and 59 (75%). All participants were using opioids, with heroin being the most common (99%). About two-thirds (64%) had been in SUD treatment in the past, including 50% who had previously received medications for OUD. About half had received services at an emergency room in the past year, while half had also overdosed in the past (51%) and 70% had witnessed someone else overdose. Most participants (69%) reported having unstable housing, including living with someone else (52%), living in a shelter (7%), and being homeless without shelter (9%).
The research team first examined transitions across the phases of outreach and treatment descriptively. They then examined characteristics that made individuals more or less likely to move from one phase to the next, starting with the linkage meeting and ending 30 days after intake into a treatment program. These characteristics included gender, race, ethnicity, age, recent substance use, prior treatment, prior overdose, employment status, marital status, living situation/homelessness, health insurance, recent incarceration, and recent medical involvement.
WHAT DID THIS STUDY FIND?
Rates of dropout varied across phases of outreach and treatment.
As shown in the Figure, there was a high risk of dropout between agreeing to the linkage meeting during the outreach encounter and attending the linkage meeting, despite transportation being arranged by project staff. Only 59% of those who agreed to a treatment linkage meeting actually completed the meeting. Conversely, most people who completed a treatment linkage meeting also completed a treatment intake (78%), and most of those who completed a treatment intake received their first dose of medication (91%). Treatment retention rates were slightly lower, with 71% of those who received their first dose of medication for OUD still being in treatment 30 days later. Overall, only 30% of eligible participants who agreed to a linkage meeting were retained in treatment for 30 days.
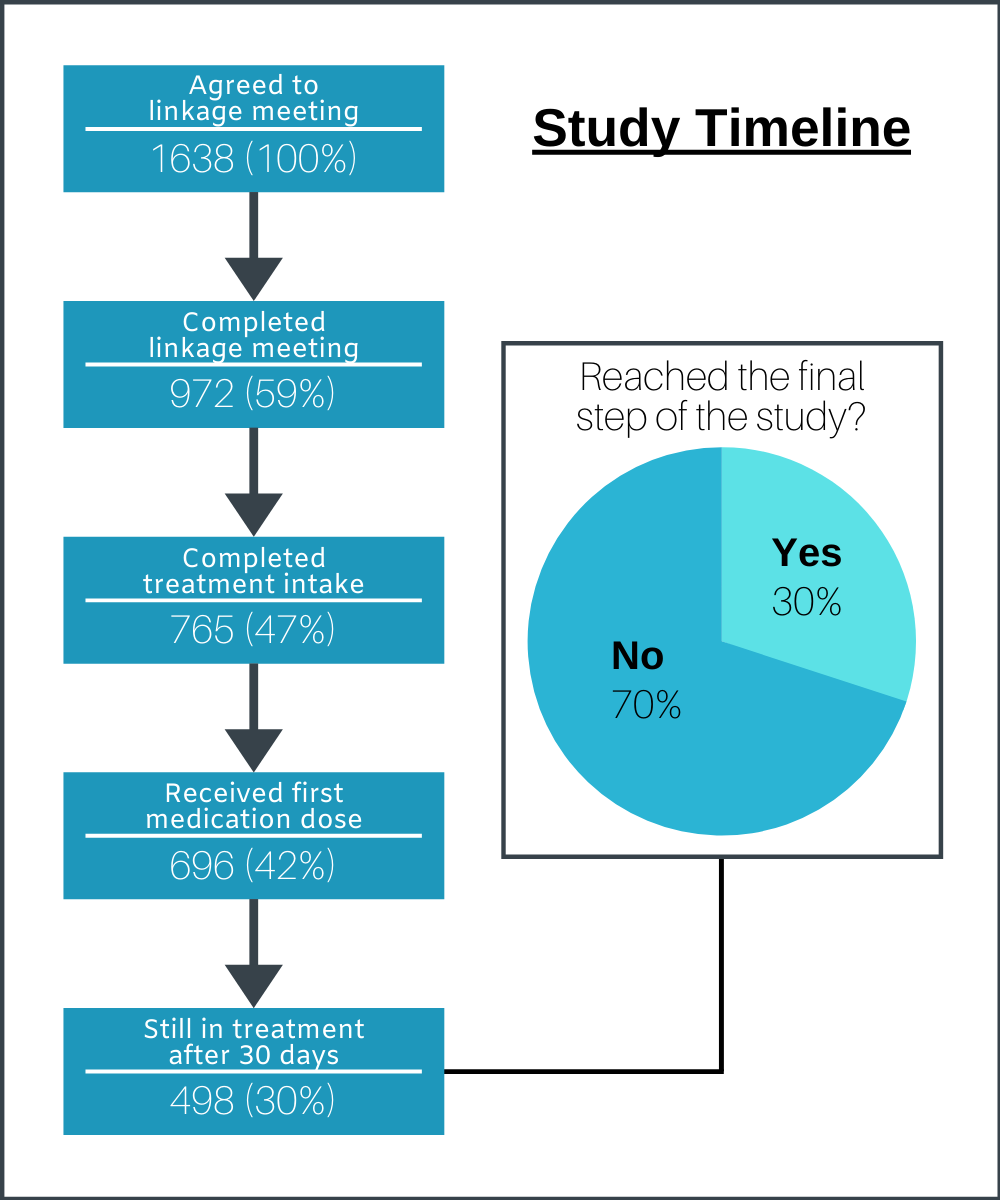
Figure 2.
Race and age made a difference in the likelihood of progressing through the treatment phases.
Compared to other races, African American individuals were 72% more likely to attend the linkage meeting following initial outreach and the subsequent MAT intake. In contrast, Caucasian individuals were less likely to attend the linkage meeting (34% less likely) and MAT intake (62% less likely), and Hispanic (38% less likely) and other races/ethnicities (48% less likely) were less likely to attend the linkage meeting. Older individuals (ages 50-59) were more likely than other age groups to attend the linkage meeting (24% more likely) and to still be in treatment 30 days after intake (39% more likely) but were no more or less likely to attend the MAT intake. In contrast, younger individuals (ages 19-29 and 30-39) were less likely to attend the linkage meeting (53%-63% less likely) and the MAT intake (52%-86% less likely), and individuals ages 30-39 were also less likely to remain in treatment after 30 days (53% less likely).
Prior experience with MAT and recent SUD treatment increased the likelihood of progressing through some of the treatment phases.
Individuals who had ever received medication for OUD (7% more likely) and those who had been in SUD treatment (2 times more likely) in the past 6 months were more likely to attend the linkage meeting following initial outreach. Neither of these variables predicted attendance at the MAT intake, however, and only prior MAT treatment increased the likelihood of remaining in treatment after 30 days (43% more likely). In contrast, ever receiving naloxone (a drug that is administered to reverse the effects of an opioid overdose), predicted a lower likelihood of attendance at the MAT intake and of remaining in treatment after 30 days (34%-36% less likely).
Individuals with stable housing were more likely to attend the MAT intake.
While housing and homelessness did not predict the likelihood of attending the linkage meeting or remaining in treatment after 30 days, these variables did impact the likelihood of attending the MAT intake session. Individuals who had their own housing (76% more likely) and those who had not spent the night on the street or in a shelter in the past year (75% more likely) were more likely than others to attend the MAT intake session. In contrast, individuals who were currently living on the street (67% less likely) and those who spent the night on the street or in a shelter more than 10 times in the past year (44% less likely) were less likely to attend this session.
Having Blue Cross Blue Shield insurance was the strongest predictor of remaining in treatment after 30 days.
Compared to those with other types of insurance and no insurance, individuals with Blue Cross Blue Shield insurance were three times as likely to remain in treatment after 30 days. Type of insurance did not affect the likelihood of attending the linkage session or the MAT intake.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study examined the use of peer outreach and treatment linkage interventions in helping individuals who were using opioids to connect with OUD medication treatment. The study targeted people living in communities that were heavily impacted by the opioid crisis, most of whom were African American, had unstable housing, and had experienced prior opioid overdoses. None of the study participants were in treatment at the time of initial outreach, but half of the sample had received OUD medications in the past year, highlighting the difficulty of retaining individuals even once medication treatment is initiated. Roughly half of the sample had also received treatment in an emergency department (ED) in the past year. Other research has highlighted the utility of connecting individuals with OUD medications while in the ED to improve treatment engagement.
Peer outreach workers were able to connect 59% of the individuals in this study to a treatment linkage meeting. Completion of the linkage meeting then led 47% of the initial sample to complete a treatment intake, 42% to receive the first dose of medication, and 30% to successfully complete 30 days of treatment. This successful linkage of high-risk individuals to treatment is consistent with research supporting the effectiveness of peer interventions in reducing substance use.
National data show that fewer than 20% of people with OUD received a medication to treat OUD in the past year, despite medication being recognized as an important component of treatment. Peer outreach workers and project staff in this study were able to connect 42% of the sample to an initial dose of OUD medication and 30% to 30 days of medication assisted treatment. This study did not include a control group, however, which prevents the determination of specific reasons for the higher rates of treatment engagement than those seen in national surveys. However, it is possible that the assertive outreach completed in this study helped individuals to overcome the frequently identified barrier of not knowing where or how to access treatment by directly connecting them to services. The linkage meeting, which used motivational interviewing techniques to help individuals increase their motivation for further treatment, may have helped individuals overcome the barrier of not being ready for treatment.
In addition to not being ready for treatment and not being sure where to get it, the cost of treatment is also a commonly cited barrier to treatment by individuals with SUD. In this study, having Blue Cross Blue Shield insurance was the strongest predictor of retention in treatment for 30 days. Other studies have found that having Medicaid coverage, in comparison to other types of insurance or no insurance, is a predictor of receiving medications for OUD. As treatment cost and lack of insurance coverage continues to be a barrier to treatment for one-fifth of individuals with SUD who believe they need treatment, identifying ways to reduce this barrier could allow thousands of Americans to access necessary treatment services. In the absence of a control group who did not receive the peer outreach or treatment linkage interventions, however, it is not possible to rule out other explanations for this finding (for example, that individuals who had Blue Cross Blue Shield insurance had more resources that could account for their greater likelihood of treatment retention).
This study found that African American individuals, who represented the majority of the sample (85%) were more likely to attend the linkage meeting and the MAT intake. In contrast, Caucasian individuals were less likely to attend the linkage meeting and MAT intake, and Hispanic and other races/ethnicities were less likely to attend the linkage meeting. While race and ethnicity did not impact retention in treatment in this study, prior research has found that African American individuals are less likely than White individuals to complete SUD treatment. Continued attention to differences in treatment engagement and retention across racial and ethnic groups, as well as close examination of the reasons for observed differences, will allow for equitable access to SUD treatment.
- LIMITATIONS
-
- This was a single group, observational study, meaning that there was no group of individuals who did not receive the intervention or received a different intervention to which those receiving the peer outreach could be compared. As such, it cannot be concluded with certainty that the benefits observed in this study are attributable to the intervention (and not something else).
- As initial outreach was conducted in informal, public settings, it was not possible to collect extensive data on the 3,308 encounters who were eligible for the study. Data were collected from, and analyses performed on, the 1,638 individuals who agreed to a linkage meeting, representing approximately half of the original sample. It is not known how these individuals compare to those who declined to participate in the linkage meeting.
- When conducting the primary analyses, the researchers did not control for other variables that could feasibly impact the outcome variables, such as greater recovery capital or higher socioeconomic status.
BOTTOM LINE
- For individuals and families seeking recovery: This study used a peer outreach and treatment linkage intervention to engage individuals with OUD in medication-based treatment. The study also explored predictors of successful engagement and retention in treatment. Findings showed that assertive outreach using peers in recovery was able to actively engage approximately 500 high-risk opioid-addicted individuals – who were not actively seeking treatment themselves at the time – into proven medication treatment for at least 30 days. The study also found that factors such as being African American and older, as well as having Blue Cross Blue Shield insurance, stable housing, and prior experience with OUD medications and SUD treatment, predicted further progression in treatment. Patients and families who maintain an awareness of the high risk of dropout from OUD treatment may be better able to anticipate and work through barriers to successful treatment retention. This study and related studies suggest that peer outreach and motivational treatment linkage interventions are likely to be helpful to individuals and families seeking recovery.
- For treatment professionals and treatment systems: This study examined the feasibility and outcomes of a peer outreach and treatment linkage intervention for individuals with OUD and explored predictors of successful engagement and retention in treatment. Findings showed that assertive outreach using peers in recovery was able to actively engage approximately 500 high-risk opioid-addicted individuals – who were not actively seeking treatment themselves at the time – into proven medication treatment for at least 30 days. The study also found that factors such as being African American and older, as well as having Blue Cross Blue Shield insurance, stable housing, and prior experience with OUD medications and SUD treatment, predicted further progression in treatment. If treatment professionals and treatment systems can prevent dropout from treatment by attending to factors that are associated with dropout, patient outcomes are likely to improve. This study and related studies suggest that peer outreach and motivational treatment linkage interventions are likely to be a helpful component of treatment, particularly in reaching individuals who are not already treatment-seeking.
- For scientists: This study examined the feasibility and outcomes of a peer outreach and treatment linkage intervention for individuals with OUD and explored predictors of successful engagement and retention in treatment. Findings showed that assertive outreach using peers in recovery was able to actively engage approximately 500 high-risk opioid-addicted individuals – who were not actively seeking treatment themselves at the time – into proven medication treatment for at least 30 days. The study also found that factors such as being African American and older, as well as having Blue Cross Blue Shield insurance, stable housing, and prior experience with OUD medications and SUD treatment, predicted further progression in treatment. Conclusions drawn from this study are limited by its observational nature and lack of a comparison condition that received no intervention or a different kind of intervention. Future research using experimental or rigorous quasi-experimental designs would allow for causal conclusions to be drawn about the efficacy of peer outreach and treatment linkage interventions in increasing engagement and retention in medication-based treatments for OUD.
- For policy makers: This study examined the feasibility and outcomes of a peer outreach and treatment linkage intervention for individuals with OUD and explored predictors of successful engagement and retention in treatment. Findings showed that assertive outreach using peers in recovery was able to actively engage approximately 500 high-risk opioid-addicted individuals – who were not actively seeking treatment themselves at the time – into proven medication treatment for at least 30 days. The study also found that factors such as being African American and older, as well as having Blue Cross Blue Shield insurance, stable housing, and prior experience with OUD medications and SUD treatment, predicted further progression in treatment. Having Blue Cross Blue Shield insurance was the strongest predictor of retention in treatment for 30 days, and having stable housing was a strong predictor of completing a MAT intake. Policy makers can assist individuals seeking recovery from SUD by advocating for policies that mandate full and long-term coverage of SUD treatment services by insurance companies, as well as policies that provide stable housing to all individuals.
CITATIONS
Scott, C. K., Dennis, M. L., Grella, C. E., Kurz, R., Sumpter, J., Nicholson, L., & Funk, R. R. (2020). A community outreach intervention to link individuals with opioid use disorders to medication-assisted treatment. Journal of Substance Abuse Treatment, 108, 75–81. doi: 10.1016/j.jsat.2019.07.001

