Racial & Ethnic Disparities in Outpatient Treatment Completion: The Role of Primary Substance
Certain racial and ethnic minority groups are over-represented in outpatient treatment for substance use disorder, yet they are less likely to complete treatment.
This study used national data to determine if the relationship between race and treatment completion was the same when the primary substance of choice was alcohol, cocaine, marijuana, heroin, or methamphetamine.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
People seeking treatment for substance use disorder are more likely to attend outpatient treatment compared to detoxification and residential programs. Ensuring that patients complete treatment is critical as it is associated with longer term abstinence, fewer relapses, fewer readmissions, higher levels of employment, less criminal involvement, and better overall health. However, not all racial/ethnic groups are equally as likely to complete outpatient treatment. This is particularly concerning given that some racial/ethnic groups (e.g., African Americans) are over-represented in outpatient treatment.
Of additional concern is the knowledge gap that exists at the intersection of race/ethnicity and choice of primary substance in studies of treatment completion. Ultimately, if we can identify who is most likely to not complete treatment, then we can conduct research as to the reasons why, and start to identify actionable targets to improve treatment retention.
HOW WAS THIS STUDY CONDUCTED?
The Treatment Episode Dataset-Discharge (TEDS-D; SAMHSA, 2013) is a system that includes records for approximately 1.5 million substance use disorder treatment admissions annually and is considered the gold standard for epidemiological research on US treatment programs. The TEDS dataset is comprised of a significant proportion of all admissions in the US and is of interest to stakeholders because many of the admissions are financed through public funds. Using the TEDS data set, this study analyzed 416,224 outpatient treatment completion episodes for adults in urban areas from the year 2011.
The Researchers Hypothesized:
- That African Americans and Hispanics have a lower likelihood of treatment episode completion as compared to Whites
- The probability of treatment completion is associated with primary substance. In this case, heroin (including other opiates), cocaine, marijuana, and methamphetamines were hypothesized to be associated with lower treatment completion as compared to alcohol as the primary substance
- Across different primary substances, the association between racial/ethnic group status and treatment completion will differ in strength. Analyses statistically adjusted (i.e., controlled for) for other sociodemographic factors such as age and sex to separate out the effects.
WHAT DID THIS STUDY FIND?
The first hypothesis was supported when they found that treatment episode completion varies substantially by racial/ethnic group membership.
White participants had the highest completion rate (50%) while Hispanic (47%) and African American participants were significantly lower (40%).
Regarding the second hypothesis, treatment completion was found to vary by primary substance.
Specifically, participants who used alcohol had the highest completion rate (57%), followed by methamphetamine (52%), marijuana (46%), cocaine/crack (39%), and heroin (30%).
The results supported the third hypothesis that the relationship between racial/ethnic group and treatment completion vary in strength across different primary substances.
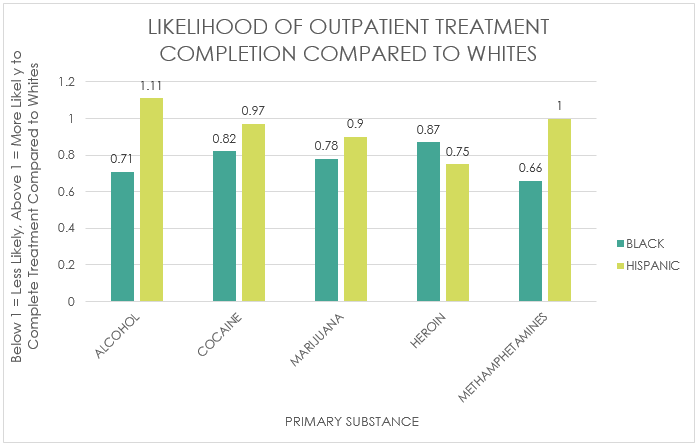
African American participants were significantly less likely than White participants to complete treatment across all types of substances (69% as likely after adjusting for demographics). The disparity in treatment completion between African American and White participants was significantly stronger when alcohol was the primary substance (i.e., African Americans 71% as likely to complete treatment) compared to when the primary substance was cocaine (82% as likely), marijuana (78% as likely), and heroin (87% as likely). African Americans were also 66% as likely than White participants to complete treatment when the primary substance was methamphetamines.
For Hispanic participants, the disparity is driven primarily by heroin use disorder, for which they are only 75% as likely as White participants to complete outpatient treatment. Interestingly, Hispanic participants whose primary substance was alcohol were significantly more likely to complete treatment than Whites; however, the effect size was negligible. For marijuana, being Hispanic as compared to being White is associated with lower treatment completion; however, the effect size was trivial whereas for cocaine and methamphetamine, being Hispanic (compared to White) had no significant effect on the likelihood of treatment completion. Although the effect size for Hispanic participants completing treatment for marijuana use disorder was trivial, its notable because a greater proportion of Hispanic patients enter outpatient treatment for marijuana use disorder compared to White patients (24% versus 15%) which means the effect impacts a greater share of the Hispanic population.
WHY IS THIS STUDY IMPORTANT
This is the first study that used national data to provide evidence that racial and ethnic disparities in urban outpatient substance use disorder treatment completion vary across primary substance.
For African American participants, the disparity observed in treatment completion when methamphetamines & possibly alcohol were the primary substance, may be related to social isolation.
African Americans were considerably less likely than Whites to be in treatment for methamphetamine use disorder (1% versus 8% respectively) or alcohol use disorder (32% versus 46% respectively) compared to other substances. If African Americans with an alcohol or methamphetamine use disorder are in a treatment environment where the majority of patients are from a different social, economic, or cultural backgrounds they may find it more difficult to feel connected and identify with other patients and thus feel more psychologically isolated. This could potentially decrease treatment retention.
For Hispanics participants, the disparity observed is driven largely by the fact that Hispanics are 75% as likely to complete outpatient treatment for heroin use disorder as compared to Whites.
The racial/ethnic disparity in treatment completion rates for heroin use disorder may reflect differences in other important determinants. The use of medication for the treatment of heroin use disorder has become more widely available. Racial/ethnic differences in the use of medication to treatment of heroin use disorder, however, may exist and be attributable to either patient preferences or discriminatory provider practices.
Provider differences in the likelihood of offering medication to various racial/ethnic groups with the same degree of heroin use disorder severity are unknown. Provider differences, however, have been well documented in opioid prescribing patterns to relieve pain for other conditions including those associated with drug-seeking behavior.
- LIMITATIONS
-
- This sample was limited to outpatient programs in urban areas of the US; therefore, it is unknown how the findings generalize to patient discharges from programs in rural areas or residential programs.
NEXT STEPS
This study, along with many other studies of treatment completion, rely on client level characteristics that were assessed at admission to explain outcomes. More research needs to take into account program level factors (e.g., availability of open slots, non-profit versus for-profit ownership status, etc.) and the interaction with client level factors (e.g., recovery motivation to improve our understanding of why various racial/ethnic groups drop-out or complete treatment for substance use disorder.
In addition, the degree to which Hispanic individuals had equivalent access or use of medication to support treatment completion is unknown in this study. The degree to which patient preferences or attitudes towards the use of medication to treat heroin use disorder vary according to race or ethnicity is not well understood and warrants further research.
BOTTOM LINE
- For individuals & families seeking recovery: This national study found that African Americans were less likely to complete treatment compared to Whites across all substances, but the disparity was strongest for alcohol and methamphetamine use disorders. Hispanic individuals were less likely to complete treatment compared to White individuals but the effect was driven by heroin use disorder. If you or a family member are in need of treatment for alcohol or other drug use, know that completing treatment is important as it is associated with long-term abstinence, fewer relapses, fewer readmissions, higher levels of employment, less criminal involvement, and better overall health. Finding ways to help keep your loved-one in outpatient treatment may improve your loved-one’s quality of life and help sustain long-term recovery.
- For scientists: This study showed that racial and ethnic disparities in treatment completion rates were dependent on primary substance. This highlights the importance of examining subgroup differences in future treatment completion research. In addition, the degree to which disparities in treatment completion place racial/ethnic minorities at a disadvantage for achieving long term sobriety and recovery (i.e., 5+ years) is unknown, but would need to be considered in the context of primary substance.
- For policy makers: This study showed that for African Americans, there is a disparity in outpatient treatment completion rates in urban areas for all primary substances, but is particularly strong for alcohol and methamphetamine use disorder. For Hispanics, the racial/ethnic disparity in treatment completion is driven by heroin use disorders. Considering that racial/ethnic minorities are over represented in outpatient treatment, this may contribute to short and long-term health disparities. Ultimately it could provide a public health benefit to use available resources to prioritize research, treatment, and policies to remedy racial and ethnic disparities in outpatient treatment completion rates.
- For treatment professionals and treatment systems: Not all racial/ethnic groups are equally as likely to complete outpatient treatment and the strength of this relationship varies according to primary substance. African Americans are less likely to complete treatment than Whites across all substances and Hispanics are less likely to complete treatment for heroin use disorder. Consider adopting more multicultural approaches to the treatment of substance use disorders in order to improve retention rates and long-term health equality in recovery. For example, hiring staff with similar backgrounds to clientele, using treatment methods that reflect culturally specific values, and performing cultural competence assessments are all methods used to improve treatment for diverse clientele.
CITATIONS
Mennis, J. & Stahler, G. J. (2016). Racial and ethnic disparities in outpatient substance use disorder treatment episode completion for different substances. Journal of Substance Abuse Treatment, 63, 25-33.

