Evidence for Alcoholics Anonymous effectiveness and cost-effectiveness
Alcoholics Anonymous (AA) is the world’s largest recovery support service and has helped countless tens of millions of individuals recover from addiction. This recently released comprehensive report systematically reviews the science to date on AA, and used rigorous meta-analytic techniques to weigh the evidence on its effectiveness and cost-effectiveness.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Alcoholics Anonymous (AA) has several million members in 180 countries, has continuously operated for almost a century, and is the world’s most widely available and widely used mutual-help organization. Yet since AA started to be formally studied by clinical scientists in the late 20th Century, scholars have debated its effectiveness. Though many early studies showed benefits of AA, the rigor and methodology of much of this research was questioned, and up until the late 1980s, there were few gold-standard randomized controlled trials or rigorous quasi-experimental studies. In the early 1990s, however, the United States National Institute of Alcohol Abuse and Alcoholism (NIAAA) called for more rigorous investigation of AA, and its mechanisms. Researchers responded in kind, developing increasingly sophisticated methods for evaluating AA, and developing and testing clinical interventions that provide systematic clinical linkages to AA, comparing such interventions to empirically-supported treatments, such as commonly used cognitive-behavioral therapy (CBT). This systematic review and meta-analysis was conducted through the Cochrane Library of systematic reviews – the recognized gold standard in scientific rigor for medical research. This Cochrane report on AA thus represents the most comprehensive and up to date review and analysis of the scientific literature on AA. A succinct summary of the Cochrane report findings was subsequently published in Alcohol & Alcoholism and is available here.
HOW WAS THIS STUDY CONDUCTED?
This was a systematic review and meta-analysis of 27 clinical trials of AA and a clinical intervention known as Twelve-Step Facilitation (a clinical protocol for linking patients to 12-step programs like AA), containing a total of 10,565 participants, that sought to determine the net effect of AA participation. This report was commissioned and published by the Cochrane Library, a United Kingdom-based international charitable organization formed to organize medical research findings to facilitate evidence-based choices about health interventions. Cochrane reports are written to highly specified protocols using exacting methods. It is considered the gold standard in medical research and is the international ‘go to’ source for national treatment systems and government clinical decision makers.
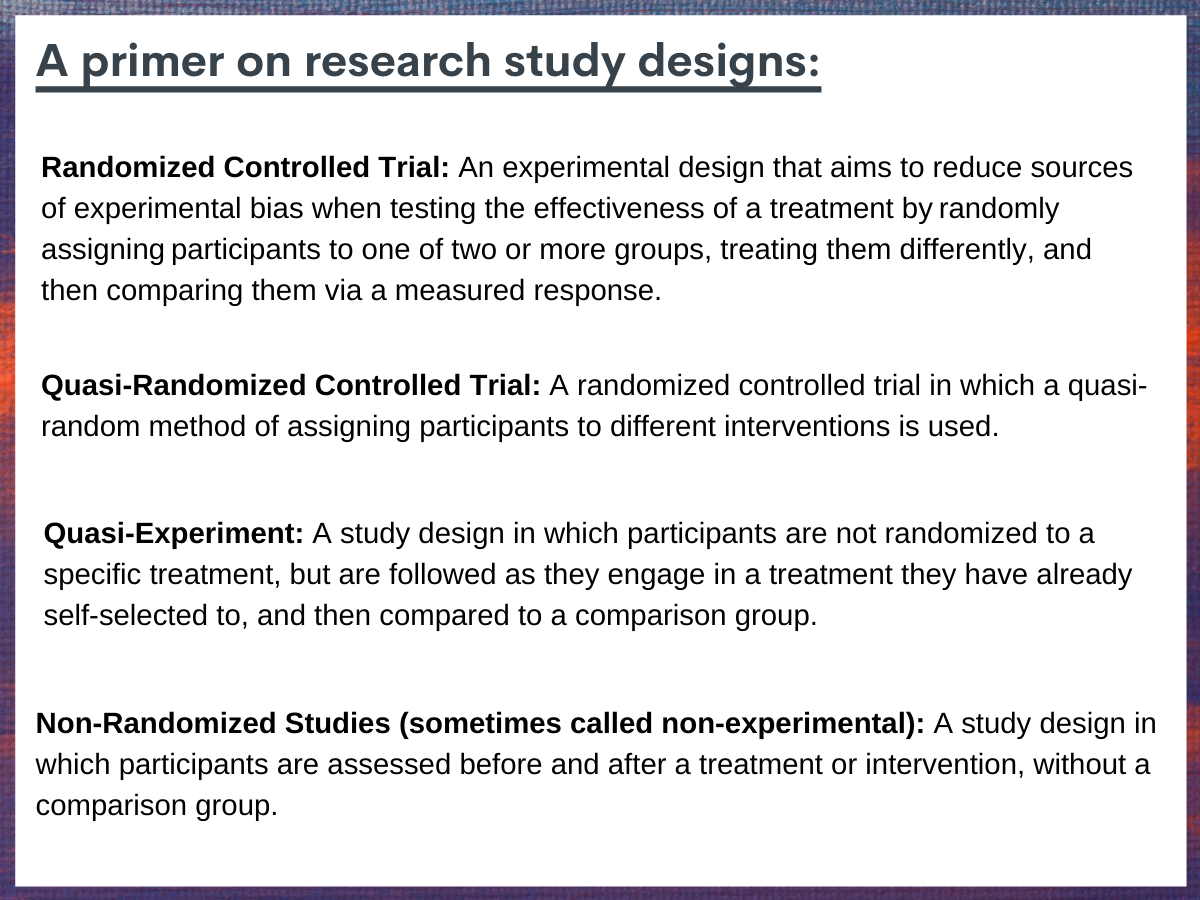
Figure 1.
For this report, per Cochrane protocol, research papers were identified through searches of 6 widely used bibliographic databases and 2 clinical trial registries with no restrictions on language or publication year. Two review authors independently scanned paper abstracts, title or both of every record to determine which studies should be considered for inclusion. Authors were contacted for clarification or additional study details when necessary. Studies were evaluated using the rigorous Cochrane Risk of Bias criteria. Studies about the economic impact of AA were evaluated separately for quality using the Evers checklist for economic evaluations.
The papers included in this review and meta-analysis examined a number of different alcohol use outcomes (e.g., abstinence, measured as the proportion of individuals continuously abstinent; percent days abstinent; longest period of abstinence; drinking intensity, measured as drinks consumed per drinking day; percentage of days heavy drinking or grams of pure alcohol consumed) and several time points (e.g., post-treatment as well as 3 months, 6 months, 12 months, and 36 months after receiving treatment). Studies also measures alcohol-related consequences, measured as physical, social and psychological sequalae resulting from alcohol. Secondary outcomes included healthcare cost offsets (e.g., mental health-related service utilization, related monetary impacts) assessed by inspection of healthcare utilization databases. Quality of life and functioning outcomes were included as possible outcomes to be included, but no studies measured these outcomes.
Twenty-one of the 27 studies that met review inclusion criteria were randomized controlled trials or quasi-experiments. Twenty-six of these primary studies contributed to the estimate of the effect of AA/Twelve-Step Facilitation and 1 contributed purely to the report’s analyses of AA’s economic impact.
Across the 27 included studies, all participants were diagnosed with AUD. The proportion of female participants ranged from 0% to 49.1%, the average sample age ranged from 34.2 to 51.0 years, and the racial composition ranged from 7.3% racial and ethnic minority participants to 76.9%.
WHAT DID THIS STUDY FIND?
AA produces rates of alcohol abstinence and alcohol use comparable to first-line clinical interventions, and outperforms them over follow-up.
In terms of alcohol abstinence, among the 27 studies reviewed, AA/Twelve-Step Facilitation generally performed as well as first-line clinical interventions at the end of treatment, and in the majority of studies performed better over follow-up (e.g., at 6, 12, 24, and 36 months after treatment).
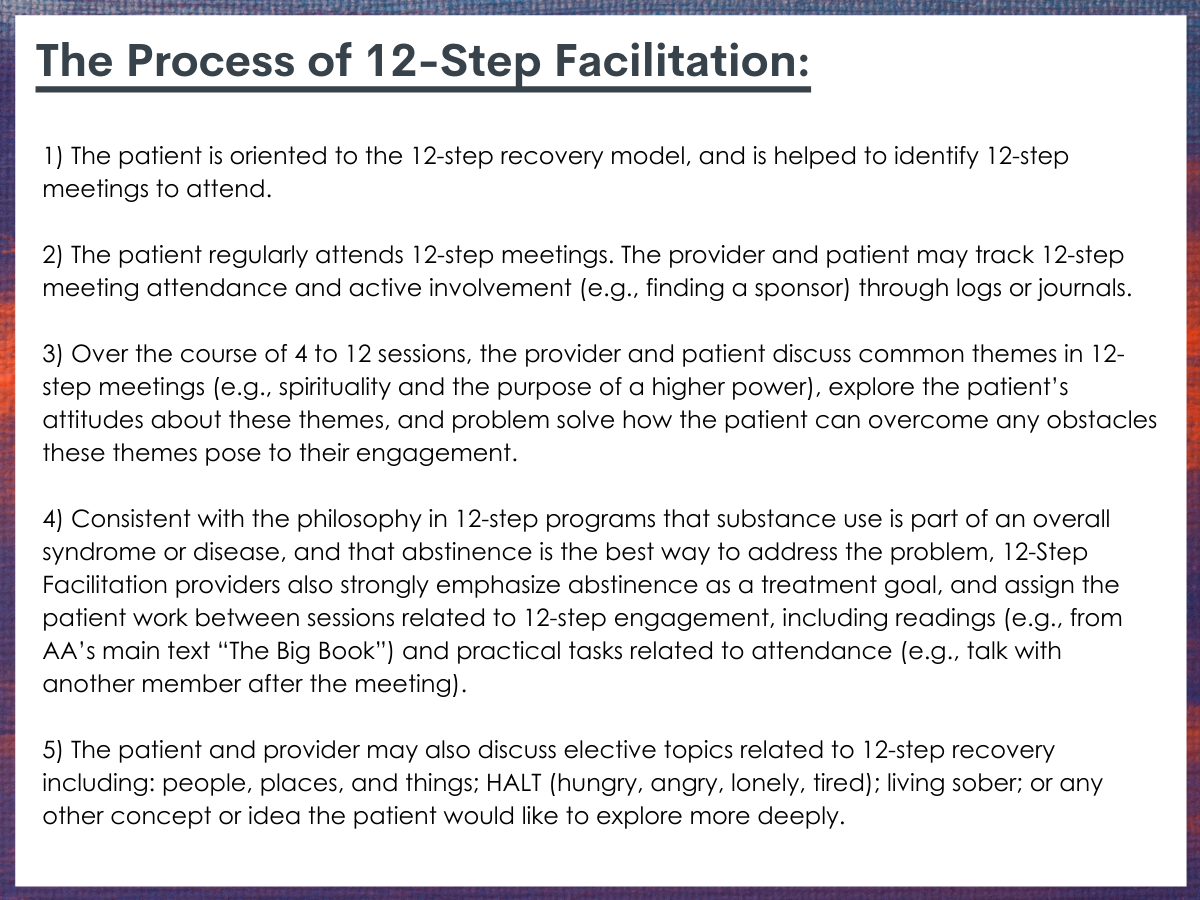
Figure 2.
For the most rigorous studies that employed a randomized controlled trial/quasi-randomized controlled trial design with manualized AA/Twelve-Step Facilitation compared to a treatment with a different theoretical orientation like Cognitive Behavioral Therapy (number of studies = 6; number of articles = 9), no difference was found for AA/Twelve-Step Facilitation at the end of treatment on abstinence measures, but there were advantages for AA/Twelve-Step Facilitation at all of the other follow-up time points (i.e., at 6, 12, 24 and 36 months) ranging from a 21% lower risk of return to alcohol use among those going to AA compared to those receiving other clinical interventions at 12-month follow-up, to a 66% lower risk of return to alcohol use among those going to AA versus those receiving clinical interventions at 6-month follow-up. 9 of these studies also assessed percent days abstinent from alcohol (versus simply measuring abstinence as yes or no). AA/Twelve-Step Facilitation showed a small to moderate advantage in terms of percent days abstinent, but only at the 24-month (Mean Difference = 12.1% days) and 36-month time points (Mean Difference = 6.6% days). AA/Twelve-Step Facilitation performed as well as comparisons interventions at other follow-up time points.
Similarly, among studies that employed a non-randomized design with at least one non-manualized treatment condition, and where AA/Twelve-Step Facilitation was compared to a different theoretical treatment orientation such as Cognitive Behavioral Therapy, all studies favored the AA/Twelve-Step Facilitation intervention at all three follow-up times: 6 months (50% lower risk of return to alcohol use), 12 months (25% lower risk of return to alcohol use), and 24 months (34% lower risk of return to alcohol use). Additionally, at the 9-month follow-up, one study showed a higher percentage days abstinent for AA/Twelve-Step Facilitation than the comparison (Mean Difference = 3.0 days), another found a slight advantage at 2 months post-treatment (p= 0.03) that favored AA/Twelve-Step Facilitation, but between 2 and 18 months, the difference between groups was not statistically significant (p= 0.05).
In terms of studies that employed a randomized controlled trial/quasi-randomized controlled trial design where at least one comparison treatment was non-manualized, and AA/Twelve-Step Facilitation was compared to a different type of Twelve-Step Facilitation (i.e., varying in Twelve-Step Facilitation style or intensity), one paper found that the more intensive AA/Twelve-Step Facilitation intervention had a 15% higher proportion of participants abstinent at the 12-month follow-up compared to the less intensive AA/Twelve-Step Facilitation intervention. Two studies also reported data for percent days abstinent, one finding no difference, and one finding an advantage for AA/Twelve-Step Facilitation compared to the comparison at 12-month follow-up (Mean Difference = 16.40). Two studies reported on days of alcohol use at the 6-month follow- up (Timko et al., 2011; Vederhus et al., 2014) and found no difference.
For studies that employed a non-randomized design with at least one non-manualized treatment condition and where AA/Twelve-Step Facilitation was compared to a different Twelve-Step Facilitation variant (i.e., in varying in Twelve-Step Facilitation style or intensity) (number studies = 2), at a 6-month follow-up one study found no difference, and at the 12-month follow-up one study found a 24% advantage for the more intensive 12-step treatment in terms of return to alcohol use rate.
AA is associated with large economic savings.
Four studies (1 randomized controlled trial/quasi-randomized controlled trial, 3 non-randomized; n = 2,657; number reports = 5) assessed AA/Twelve-Step Facilitation health care cost offsets. Three studies (4 out of 5 reports) found a healthcare cost saving in favor of AA/Twelve-Step Facilitation. Specifically, across a 3-year follow-up, one study found AA participants with severe AUD had alcohol-related outcomes similar to outpatients receiving clinical addiction treatment, yet the alcohol related health care costs associated with AA participation were 45% lower (US$2856, saved per person). They also found that compared with inpatients in AA/Twelve-Step Facilitation programs, those initially treated in Cognitive Behavioral Therapy programs had 64% higher annual healthcare costs (US$7128 per person). Despite this lower costs, AA/Twelve-Step Facilitation participants had higher abstinence rates (45.7% AA/Twelve-Step Facilitation versus 36.2% Cognitive Behavioral Therapy) and performed just as well as CBT interventions on mental health outcomes.
In a long-term study of adolescents, an analysis of two-year outcomes and healthcare costs found that participants treated in AA/Twelve-Step Facilitation programs had 30% lower costs compared with Cognitive Behavioral Therapy (US$3678 lower), and that for each additional 12-step meeting attended, there was a medical cost reduction of 4.7% during the 7-year follow-up with cost savings of US$145 for each meeting attended per year.
Using data from the Project MATCH study, another analysis identified medical cost savings during treatment and across follow-up with better cost savings associated with Cognitive Behavioral Therapy or Twelve-Step Facilitation, or both, compared to Motivational Enhancement Therapy for participants with poor prognostic characteristics (i.e., greater alcohol addiction severity, psychiatric severity and/or social network favoring alcohol use).
The rigor of included studies was generally high, though some evidence of research bias was noted.
In research, bias is a systematic distortion of the relationship between a treatment, risk factor or exposure, and clinical outcomes. Though researchers usually seek to minimize bias in their studies, even very well-designed studies often include some potential for bias. In this report, 11 of the 27 studies were rated as potentially high risk for selection bias because they either used alternation group assignment versus true randomization (6 studies), or were non-randomized (5 studies). Additionally, attrition bias, in which results are potentially influenced by failing to statically account for participants who dropped out of the study, was unclear in approximately half (14) of the studies, high in 9 studies (largely due to moderate [≥ 20%] attrition rates) and low in the remaining studies. On the whole though, the studies included in this review and meta-analysis were of high quality, and their findings can be considered valid.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Despite AA’s long-standing international popularity, there has been debate about its clinical and public health utility. Addressing this gap in knowledge was the rationale for this 2020 Cochrane Library report. The research team found that AA/Twelve-Step Facilitation was overall better than other empirically-supported treatments in facilitating continuous abstinence and remission and was at least as effective as other well-established treatments in reducing intensity of drinking, alcohol-related consequences and severity of alcohol addiction. This pattern of relative advantage for AA/Twelve-Step Facilitation interventions appeared to be consistent across both randomized controlled trials/quasi-experimental and non-randomized studies. AA/Twelve-Step Facilitation also reduced healthcare costs substantially more than other types of treatments. Furthermore, this report highlighted the large range of populations for which AA’s benefit has been demonstrated—young and old, racial and ethnic minorities, women and men, religious and nonreligious, people in different settings and across many different nations.
This report summarized studies that included Twelve-Step Facilitation, in addition to AA. It is possible that Twelve-Step Facilitation, in and of itself, could be conferring benefits as a clinical intervention. Said another way, Twelve-Step Facilitation could somehow be helping patients independently of any benefits derived from actual AA participation. However, analyses across studies included in this report indicate that the reason for Twelve-Step Facilitation’s benefit is its ability to increase AA participation (see here and here as examples). In other words, it is AA participation itself that seems to benefit individuals, and not interacting with a referring clinician, per se. That said, a clinician can powerfully influence the likelihood of an AUD patient’s participation in AA, hence the demonstrated benefits of TSF clinical interventions.
There is clear benefit associated with Twelve-Step Facilitation because it helps engage individuals with AA. It is important to note that Twelve-Step Facilitation is an active intervention, and is qualitatively very different to more passive referrals to AA. So, while the majority or treatment programs in the United States recommend 12-step participation to their patients, it is unlikely this has a large impact on the number of individuals who end up actively engaging with AA. Perhaps not surprisingly, because Twelve-Step Facilitation is an active approach that involves concrete steps that help connect individuals to AA and other 12-step programs, it has shown superiority over passive referral to AA in terms of engagement in AA.
Rigorous reviews of the research on the mechanisms of behavior change through which AA enhances recovery have found that AA typically confers benefits by simultaneously harnessing multiple therapeutic factors. This includes facilitating participant social network change, increasing recovery motivation, coping skills, abstinence self-efficacy, and psychological well-being, as well as by reducing craving and impulsivity. As noted by the researchers, it is possible that AA/Twelve-Step Facilitation commonly outperforms other treatments at a lower cost because it successfully links people to a free and easily accessible, long-term recovery support option that activates other therapeutic mechanisms similar to those activated by professional treatment, while also facilitating positive changes in people’s social networks.
While for many people AA feels like a good fit, for some the spiritual emphasis of this and other 12-step programs is not desirable. For such individuals other mutual-help programs like Self-Management and Recovery Training (SMART), and LifeRing, which are not spiritually oriented, may feel like a better fit. Though, less well studied, these programs likely confer similar benefits to 12-step programs.
In response to the COVID-19 pandemic, mutual-help groups and recovery community organizations have increased access to online recovery support meetings. However, rigorous studies examining online recovery support meeting participation to inform best practices have not yet been conducted. While the benefits likely outweigh risks, online AA participation requires formal investigation.
- LIMITATIONS
-
- This report focused on alcohol use as the primary substance use outcome, but findings may generalize to other 12-step programs like Narcotics Anonymous, which cater to individuals with other kinds of substance use disorders. Additionally, though AA focuses on alcohol use and AUD, it espouses abstinence from all drugs, and many individuals for whom a drug other than alcohol is primary attend and benefit from AA.
- Most papers reviewed in this report did not include functional outcomes like quality of life and well-being, generally considered key outcomes of AUD recovery.
- The majority of papers reviewed in this report were randomized controlled trials, which though methodologically rigorous, can have limited generalizability to the real world.
BOTTOM LINE
Evidence suggests that compared to other well-established treatments like Cognitive Behavioral Therapy, AA participation, as well as clinical linkage to AA using well-articulated Twelve-Step Facilitation manualized interventions leads to comparable alcohol abstinence outcomes at end of treatment, and enhanced abstinence outcomes over following months and years. Findings also indicate that AA/Twelve-Step Facilitation may perform as well as other clinical interventions for reducing drinking intensity outcomes (e.g., heavy drinking). Economic analyses indicate that substantial healthcare cost savings can be obtained when treatment programs proactively and systematically link people with AUD to AA using Twelve-Step Facilitation strategies. Thus, a relatively brief clinical intervention (Twelve-Step Facilitation) can help people with AUD to become engaged in a long-term, freely available, community-based, recovery support resource that can help sustain ongoing remission.
- For individuals and families seeking recovery: This report shows AA produces comparable results to first-line, clinical AUD treatments in the short-term, and outperforms these treatments in the long-term, while conferring significant cost savings. If opposed to attending AA, despite the strong evidence for its potential to aid recovery, individuals might consider alternative mutual-help organizations as they may confer benefits at similar levels of engagement. It is plausible, for example that other AUD recovery-supportive, mutual-help organizations, such as Self-Management and Recovery Training (SMART), LifeRing, Refuge Recovery, and Women for Sobriety, may confer similar benefits. Although these organizations may espouse different theoretical orientations and variations in their approaches to help people attain and maintain recovery from AUD, there may be more similarity than differences in the therapeutic dynamics operating within these groups.
- For treatment professionals and treatment systems: This report shows AA produces comparable results to first-line, clinical AUD treatments in the short-term, and outperforms these treatments in the long-term, while conferring significant cost savings. If people with AUD are opposed to attending AA, despite the strong evidence for its potential to aid recovery, providers might consider linkage to alternative mutual-help organizations as they may confer benefits at similar levels of engagement. It is plausible, for example that other AUD recovery-supportive mutual-help organizations, such as Self-Management and Recovery Training (SMART), LifeRing, Refuge Recovery, and Women for Sobriety, may confer similar benefits. Although these organizations may espouse different theoretical orientations and variations in their approaches to help people attain and maintain recovery from AUD, there may be more similarity than differences in the therapeutic dynamics operating within these groups. Importantly, simply referring patients to 12-step meetings is likely to be less successful than Twelve-Step Facilitation in terms of patients engaging in 12-step programs.
- For scientists: Because AUD tends to be highly heterogeneous in its clinical course and impact, and those suffering can often have different preferences as to the kinds of recovery pathways they wish to follow, more research is needed to study AA and other mutual-help programs. This research should explore mental health and functional outcomes (e.g., employment), as well as perceived well-being (e.g., happiness, quality of life) in addition to commonly studied alcohol/substance use outcomes. Additionally, though a substantial body of work has investigated AA’s mechanisms of behavior change, more research is needed in this domain to better understand how AA confers benefit. Given the benefits and cost-savings of AA, it will also be important to learn how to tap into its mechanisms of behavior change (e.g., motivation, social network changes, coping, etc.) for those who would prefer mutual-help groups with a different theoretical orientation.
- For policy makers: AA is an exemplar of community recovery support services that can help people recover from addiction and save healthcare systems economically. This is likely to be true across other mutual-help groups like Self-Management and Recovery Training (SMART), LifeRing, Refuge Recovery, and Women for Sobriety. Supporting addiction recovery community centers is a great way to indirectly support 12-step programs, as these venues offer meeting space and resources for meeting attendees. Additionally, though there is clear evidence of AA’s effectiveness, supporting research on AA’s mechanisms of behavior change will improve our understanding of how AA, and other mutual-help programs confer their benefits.
CITATIONS
Kelly, J. F., Humphreys, K., & Ferri, M. (2020). Alcoholics Anonymous and other 12‐step programs for alcohol use disorder. Cochrane Database of Systematic Reviews, 2020(3). doi:10.1002/14651858.CD012880.pub2
*Research features RRI personnel but was reviewed independently for this Bulletin

