Do Drug Dependent Patients in Alcoholics Anonymous (rather than Narcotics Anonymous) Do As Well?
Mutual-help organizations (MHOs) such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA), are commonly sought resources to help people recover for substance use disorder (SUD) in the U.S.
AA was the first 12-step MHO and it focuses specifically on recovery from alcohol dependence, whereas NA focuses primarily on recovery from other substances including opiates, stimulants, or cannabis, although does address alcohol as well.
The reason why NA emerged in the 1950’s was to provide a more suitable fit for those suffering from drug problems (other than alcohol) and thereby enhance the chances of recovery.
Narcotics Anonymous (NA) has only about one third the number of meetings that Alcohol Anonymous (AA) does in the U.S. and therefore smaller communities may not offer NA meetings. An ongoing clinical question has been whether treatment programs should refer patients with primary drug problems to AA, when NA is less accessible or not accessible at all in individuals’ home communities.
If primary drug patients are referred to AA rather than the more fitting NA fellowship, such a “mismatch” could result in a lowered sense of identification, belonging, and cohesion, and lead to more mismatched patients discontinuing sooner or deriving less benefit from participation.
This potential mismatching problem may be particularly important for young adults since they are more likely to report a substance other than alcohol as their primary drug. Because this question had seldom been investigated, Kelly and colleagues conducted a longitudinal clinical study of young adults treated for a variety of substance use disorders.
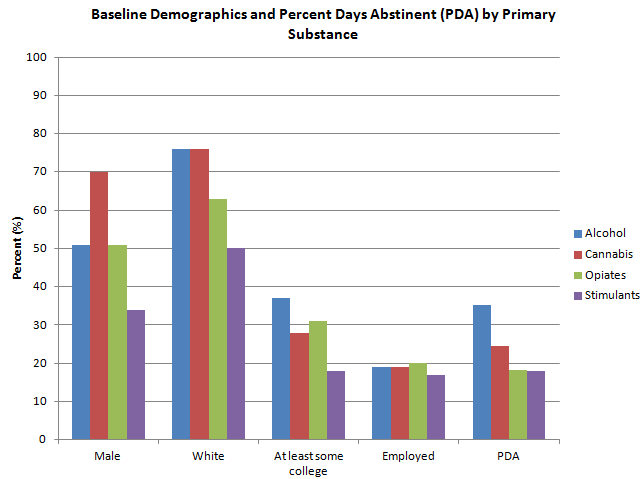
The investigators examined whether young adults (N=279) who reported cannabis (n=81), opioids (n=65), or stimulants (n=52) as their primary substance at residential treatment entry (i.e., were “primary drug” patients; 198/279; the number of primary alcohol patients was =81) – and who attended proportionality more AA than NA meetings in the first 3 months following discharge (i.e., were “mismatched”) derived less recovery benefit and were more likely subsequently to discontinue 12-step participation at 6- and 12-months after discharge.
On average, participants were 20.4 years old (18-24), 95.0% Caucasian, and 73.4% male. Abstinence from alcohol and other drugs was verified through saliva tests of individuals who lived within 50 miles of the treatment center and who completed the follow-up assessments in person.
When comparing the primary drug to the primary alcohol patients, the authors found that the proportion of meetings that were AA (i.e., were “mismatched”) ranged from an average of 69.9% at baseline to 79.4% at 6 months.
When the investigators tested whether a fellowship mismatch among primary drug patients during the first 3 months after treatment resulted in less future 12-step attendance, 12-step involvement, or lower percent days abstinent at 6- and 12-month follow-ups, the authors found no relationship.
Results suggested that, contrary to expectations, going to either AA or NA fellowship meetings following treatment may work equally well for young adults.
IN CONTEXT
Narcotics Anonymous (NA) has grown substantially over the past 50 years. Despite this growth, it remains less available than its predecessor, Alcoholic Anonymous (AA); for example, there are 20,000 NA groups in the U.S., compared to 60,000 for AA.
In that context, these findings are good news because health professionals might more confidently refer their drug-dependent patients to AA groups if they are easier for patients to access and attend than NA.
Kelly and colleagues found that all of the primary drug patients had a history of heavy alcohol use and about two thirds also met criteria for an alcohol use disorder in addition to their drug diagnosis.
Thus, while on the surface, the primary drug emphases and experiences may be different between AA and NA, there may be enough similarities in the addiction and recovery experiences among young adults with primary drug or primary alcohol problems for them to identify with other AA members and to find a pathway that can work for them too. This finding that young adults with primary drug problems may benefit from attending AA as much as NA, could be key for individuals where NA meetings are less available than AA meetings.
CITATIONS
Kelly, J. F., Greene, M. C., & Bergman, B. G. (2014). Do drug-dependent patients attending Alcoholics Anonymous rather than Narcotics Anonymous do as well? A prospective, lagged, matching analysis. Alcohol and alcoholism, 49(6), 645-653.
**Note: One or more authors of this study were Recovery Research Institute Staff, including the director and/or other research scientists. As with all summaries, staff made the greatest possible effort to recognize and account for any potential biases in the review of this article.

