Similarities and differences of abstinent versus non-abstinent alcohol use disorder remission
A relatively small proportion of people with alcohol use disorder seek specialty treatment and studies are needed to identify the various other ways people resolve alcohol problems. One strength of using general population samples, such as the one used in this study, is that they capture remission among people with and without a history of treatment. This can be helpful in understanding who is more likely to achieve abstinent remission, who may be able to achieve non-abstinent remission, and the role that treatment might play in each of these pathways.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
By studying alcohol use disorder (AUD) in the general population, as opposed to treatment samples alone, it is possible to identify more pathways to remission and the factors that may promote or impede the process. Some people achieve alcohol use disorder remission with low levels of alcohol use; however, abstinent based remission appears to be the most stable form of remission when using longitudinal studies that look at consumption and AUD symptomology. There are several trajectories that people follow with some getting worse and some improving but little is known about the factors involved in persistent versus remitting AUD. The goal of this study was to document past year drinking and symptomology status among those with a history of AUD. Although many comparisons were made, in this summary we focus on factors that differentiate persistent AUD and abstinent based remission or asymptomatic low risk drinking remission and describe the role of treatment in those trajectories. By using updated DSM 5 medical criteria this nationally representative study sought to inform policies and practices that could enhance and support alcohol related public health.
HOW WAS THIS STUDY CONDUCTED?
The authors conducted a nationally representative cross-sectional study of 7,785 people with a history of AUD (i.e., prior to the past year) and categorized the status of their drinking in the past year along with several correlates. Correlates included sociodemographic characteristics, age of onset, duration of AUD, treatment history, family history of alcohol problems, average daily alcohol intake, number of lifetime symptoms of AUD, lifetime use of any nicotine, lifetime DSM-5 illicit drug use or drug use disorder, and lifetime DSM-5 mood, anxiety, or personality disorder.
The goal of the study was to identify typologies of past year status (i.e., among people who met criteria for an AUD prior to the past year) based on 2 dimensions: symptomology (asymptomatic vs. symptomatic) according to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5), and consumption (high vs. low) according to guidelines from the National Institute of Alcohol Abuse and Alcoholism (NIAAA). High risk drinking among men was defined as drinking more than 14 drinks per week, on average, or drinking 5 or more drinks in a single day one or more times during the last 12 months. High-risk drinking among women was considered drinking more than 7 drinks per week, on average, or if they drank 4 or more drinks in a single day one or more times during the last 12 months. All other respondents who drank in the last 12 months were considered low risk drinkers. The analysis estimated the odds of past year drinking status according to 6 categories while adjusting for correlates (i.e., equating the groups on other factors).

Figure 1.
WHAT DID THIS STUDY FIND?
Among these individuals with a history of AUD, 1 year later about 1/3 were abstainers or asymptomatic low-risk drinkers (i.e., in remission), about 1/3 were high-risk drinkers or symptomatic, and about 1/3 had persistent alcohol use disorder (see Figure 2).
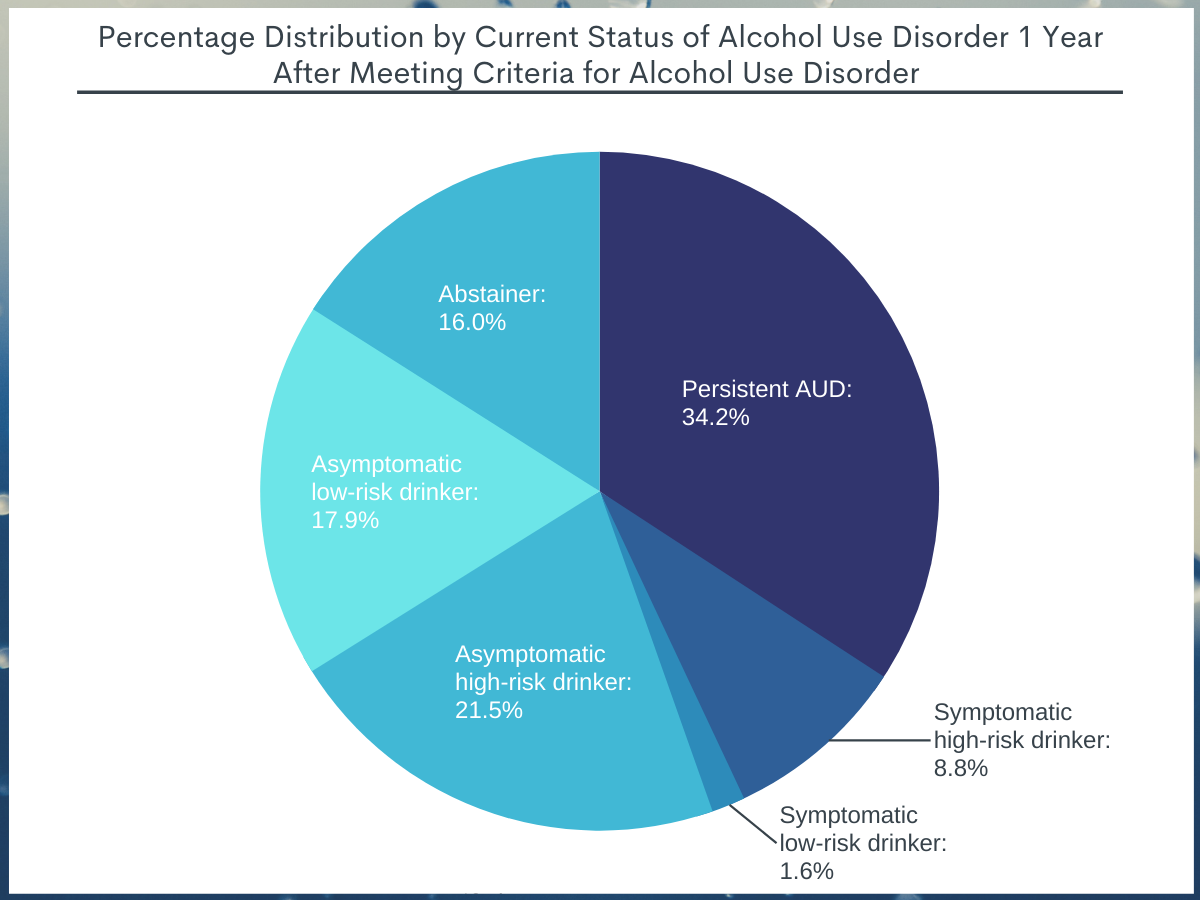
Figure 2.
Compared to persistent AUD, the following groups were more likely to be in remission and abstinent:
- Individuals who do not identify as Black were 43% more likely.
- Females were 149% more likely.
- Age 65 and over were 423% more likely.
- Those who do not have a drug use disorder were 36% more likely.
- People who use illicit drugs were 39% more likely.
- Individuals with more years since onset of AUD are 363% more likely.
- Among those who received treatment:
- Married individuals were 167% more likely.
- Individuals without a family history of AUD were 65% more likely.
- Individuals with more AUD symptoms over the course of their life were 309% more likely.
- Individuals without a personality disorder were 51% more likely.
- Among those who did not receive treatment:
- Individuals who did not attend/complete college were 54% more likely.
- Individuals with fewer AUD symptoms over the course of their life were 43% more likely.
Compared to persistent AUD, the following groups were more likely to be in remission with low-risk drinking:
- People who do not identify as Black were 42% more likely.
- Females were 130% more likely.
- Married individuals were 162% more likely.
- Individuals who do not have a mood/anxiety disorder in their lifetime were 147% more likely.
- Those who do not have a drug use disorder were 26% more likely.
- People who do not use illicit drugs were 30% more likely.
- Individuals with more years since onset of AUD are 368% more likely.
- Those with more alcohol use were 26% more likely.
- People with fewer AUD symptoms in their lifetime were 76% more likely.
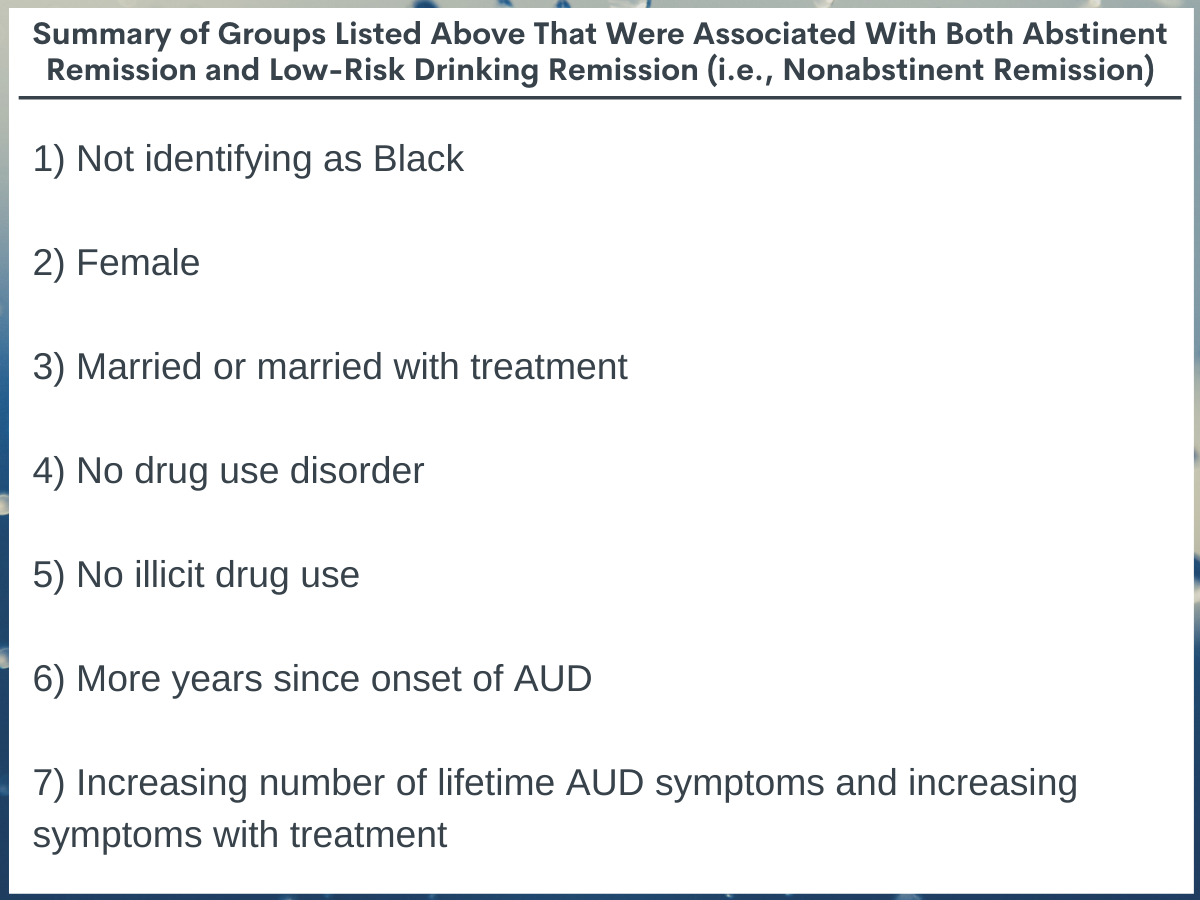
Figure 3.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Individuals who identify as Black were less likely than their White counterparts to achieve remission compared to persistent AUD. Racial identity is a social construct and when used in the context of addiction science, it may reflect social processes such as racism or discrimination as opposed to biological differences. This finding mirrors previous research that found individuals who identify as Black with less than a high school education are more likely to have a chronic and persistent course of illness compared to their White counterparts. This disparity in AUD remission rates highlights the need to identify and target risk factors to which Black individuals may be disproportionately exposed. These may include poorer quality of health care, homelessness, unemployment, poverty, incarceration, and recovery related discrimination which may present barriers to them stabilizing and decrease the likelihood of remission.
The finding that women were more likely than men to achieve abstinence or asymptomatic low-risk drinking is similar to other studies that found a lower prevalence of AUD among women. It is unclear why this is the case as little has been done investigating sex differences in recovery – an important area for future research. It may be a result of both biological differences and cultural differences like increased stigma or childcare responsibilities that increases the likelihood that women seek to stop/reduce alcohol use more quickly and more often than men (see here for more information on women in recovery).
Those who were married were more likely to achieve abstinence or asymptomatic low-risk drinking compared to persistence. Marriage can often (but not always) serve as a form of close social support and it appears the effects could be magnified in the context of treatment.
Any illicit drug use or a drug use disorder was associated with lower odds of achieving abstinence or asymptomatic low risk drinking remission. One theory around how illicit drug use may be detrimental to remission from AUD is that drug use could reduce inhibitions and trigger familiar feelings of reward associated with alcohol use which may in turn increase craving for alcohol. It could also be a marker of greater global addiction severity.
With increasing number of lifetime AUD symptoms people had a better chance at remission if they had treatment. Although treatment rates are generally low, individuals with more severe alcohol use disorders are the ones who seek professional treatment. Pharmaceutical and behavioral treatments may assist patients in reducing alcohol use or facilitating alcohol abstinence.
Prior U.S. population-based research has indicated that approximately 70% of people who have resolved a problem with alcohol or other drugs have done so without treatment. In the case here of DSM-5 AUD, about one quarter achieved remission without treatment. Many individuals, especially those with milder forms of AUD may eventually moderate or stop alcohol use on their own (commonly referred to as “natural recovery” or “unassisted recovery”). This becomes less likely, however, with increasing severity, indicated by how long someone has endured AUD and how many symptoms they experience.
- LIMITATIONS
-
- This data was collected at one time point using retrospective reports. A longitudinal design would reduce recall bias and improve accuracy.
- This study does not include institutionalized populations (e.g., incarcerated individuals, individuals currently in inpatient treatment) so it is unknown the degree to which the results generalize.
- This study includes adults only and may not generalize to adolescents.
- The research team talk about “past year recovery” but really are assessing DSM 5 remission status. “Recovery” can mean different things to different stakeholders but typically is associated with additional improvements beyond purely the absence of AUD symptoms/remission (e.g., improvements in quality of life, meaning and purpose, and functioning).
BOTTOM LINE
- For individuals and families seeking recovery: This study used nationally representative data of people in the United States and found diversity among the typologies that emerged 1 year after a AUD. Remission from AUD is achievable and only 1/3 had persistent AUD the following year. Treatment makes remission more likely, particularly among those with a more severe AUD or co-occurring drug use. Seeking treatment early and often is likely to yield improved functioning and quality of life and save lives.
- For treatment professionals and treatment systems: This was a cross-sectional analysis of a nationally representative sample of people with a history of AUD. One-quarter of individuals achieved abstinence or asymptomatic low-risk drinking in the past year without the benefit of treatment. A greater percentage of individuals achieving abstinence (43.2%) reported receiving treatment relative to those with asymptomatic low-risk drinking (12.3%). This may reflect the role of providers in guiding patients to an abstinence-based goal. Research has shown that while there are many pathways to AUD remission, abstinence-based remission is more stable over time.
- For scientists: Data from a large representative sample of the United States was used to examine correlates of past-year drinking status among individuals with prior-to-past-year AUD. Remission was less likely among individuals who identify as Black and those with a history of drug use or drug use disorder. As was done with prior versions of the NESARC using DSM-IV criteria, prospective study over a period of 3 years using these more recent DSM-5 criteria would further elucidate the course of AUD, the role and timing of the correlational effects, and other factors that support or impede remission.
- For policy makers: This study found diversity in drinking status 1 year after meeting clinical criteria for AUD. About 1/3 were abstainers or asymptomatic low-risk drinkers (both are types of remission), about 1/3 were high-risk drinkers or symptomatic, and about 1/3 had persistent AUD. While individuals with severe AUD may experience a chronic course, AUD overall is generally considered to have a good prognosis. That is, the majority of individuals will eventually achieve a symptom free life (i.e., sustained remission). Importantly, one-quarter of individuals achieved remission in the past year without the use of any treatment – a more achievable pathway for those with less severe forms of AUD. That is, these individuals have fewer symptoms and have been living for fewer years with the disorder.
CITATIONS
Fan, A.Z., Chou, S.P., Zhang, H., Jung, J. & Grant, B.F. (2019). Prevalence and correlates of past-year recovery from DSM-5 alcohol use disorder: Results from National Epidemiology Survey on Alcohol and Related Conditions-III. Alcoholism: Clinical and Experimental Research, 43(11), 2406-2420. doi:10.1111/acer.14192.

