What factors influence retention in buprenorphine and methadone treatment?
Medication treatments for opioid use disorder are effective lifesaving therapies, and studies suggest that longer treatment durations result in better patient outcomes (e.g., reduced overdose death risk, less use of ambulatory care services). Identifying the factors that best predict retention can ultimately help us develop and roll out strategies to enhance retention. In this study, the researchers examined which factors were the strongest predictors of medication retention in an Australian sample.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Medication treatments for opioid use disorder, including opioid agonist treatments like methadone and buprenorphine (also known by the brand name, Suboxone), are effective lifesaving therapies that reduce overdose risk and help facilitate successful treatment and recovery. Despite the efficacy of these medications, retention in treatment is an ongoing issue.
These medications are most effective when taken over the long term, with research suggesting that treatment durations longer than 6 months can significantly reduce risk of overdose and hospitalization. Many individuals who start medication treatment for opioid use disorder are not retained beyond 12 months. However, retention rates vary from ~20-80%, suggesting a need to identify the factors that can influence treatment retention. Studies have started to reveal some of these influential factors, including patient and treatment characteristics, such as better retention in women, in older adults, and with higher doses of buprenorphine and methadone. However, additional research is needed to replicate these findings and to identify other influential factors, as it could ultimately help better identify and address barriers to opioid use disorder treatment retention. This study examined treatment retention in patients starting buprenorphine or methadone treatment, as well as the influence of patient, treatment, and prescriber characteristics on treatment retention.
HOW WAS THIS STUDY CONDUCTED?
This study was a retrospective longitudinal investigation of a population-based cohort of patients starting buprenorphine or methadone treatment for opioid use disorder in Australia, which examined treatment retention in the first 150 months of a treatment episode, and its relationship to individual characteristics of the patient, prescriber, and treatment regimen.
The researchers obtained data from five linked state-wide datasets (New South Wales, Australia) that contained information on opioid agonist treatment episodes (start/end dates, place medication is dispensed, etc.), criminal records, hospitalizations, mental health diagnoses, and mortality. These datasets include records from New South Wales, which houses Australia’s largest opioid agonist treatment program and provides buprenorphine and methadone treatment to more than 40% of Australia’s opioid agonist treated patients.
Using this data, the researchers examined a cohort of 22,577 patients who started their first opioid agonist treatment episode between 2001 (when buprenorphine was first available for the treatment of opioid use disorder in Australia) and 2015 and were followed up through 2017. An opioid agonist treatment episode was defined as continuous treatment with no more than a 6-day break in treatment at any given time. Patients with no recorded treatment end date were assumed to still be in treatment at the time of follow-up (2017).
As part of the treatment intake, all patients completed a biopsychosocial assessment, were provided information on treatment options, and developed a treatment plan with treatment intake staff. Standard protocols within these opioid treatment programs included the dispensing of medications at treatment clinics and at community pharmacies, and the delivery of medical, social and psychological treatments alongside medication. All prescribers were required to obtain accreditation to prescribe opioid agonist treatments.
The majority of patients were men (69%) living in a major city (70%), who had no criminal history in the year prior to starting treatment (69%). The percentage of patients starting a new methadone treatment episode declined from 74% in 2001 to 38% in 2015, reflecting the introduction of buprenorphine as an approved treatment for opioid use disorder in Australia in 2001. On average, patients were followed up for 9 years and 6.9% of the patient cohort died at some time during the study period. Among the 22,577 patients who started opioid agonist treatment for the first time, a total of 65,371 treatment episodes were initiated between 2001 and 2015, and 56,411 episodes were ended during the follow-up period, meaning some patients stopped and re-initiated medication treatment one or more times after their first episode.
WHAT DID THIS STUDY FIND?
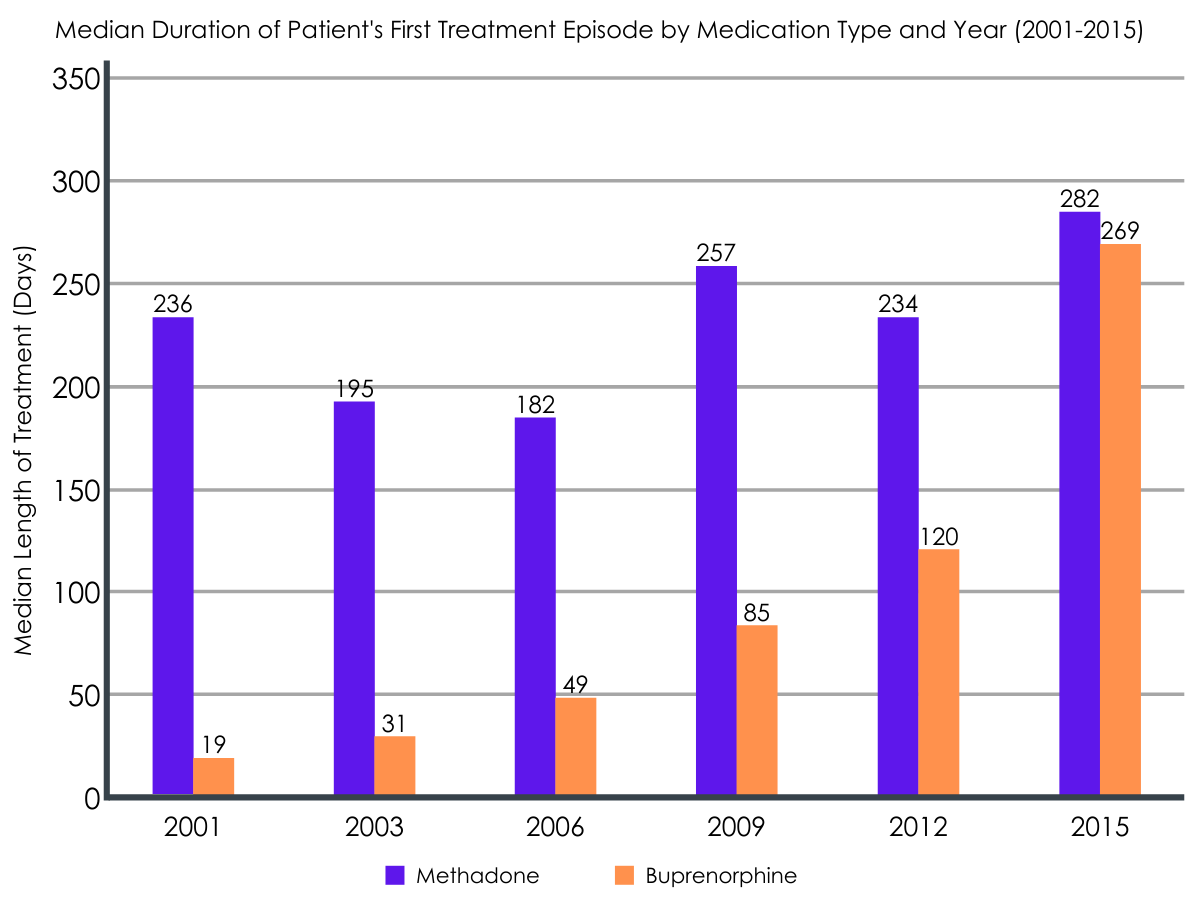
The duration of patients’ first opioid agonist treatment episode was about 131 days, with duration of the first buprenorphine treatment episode increasing since its introduction in 2001.
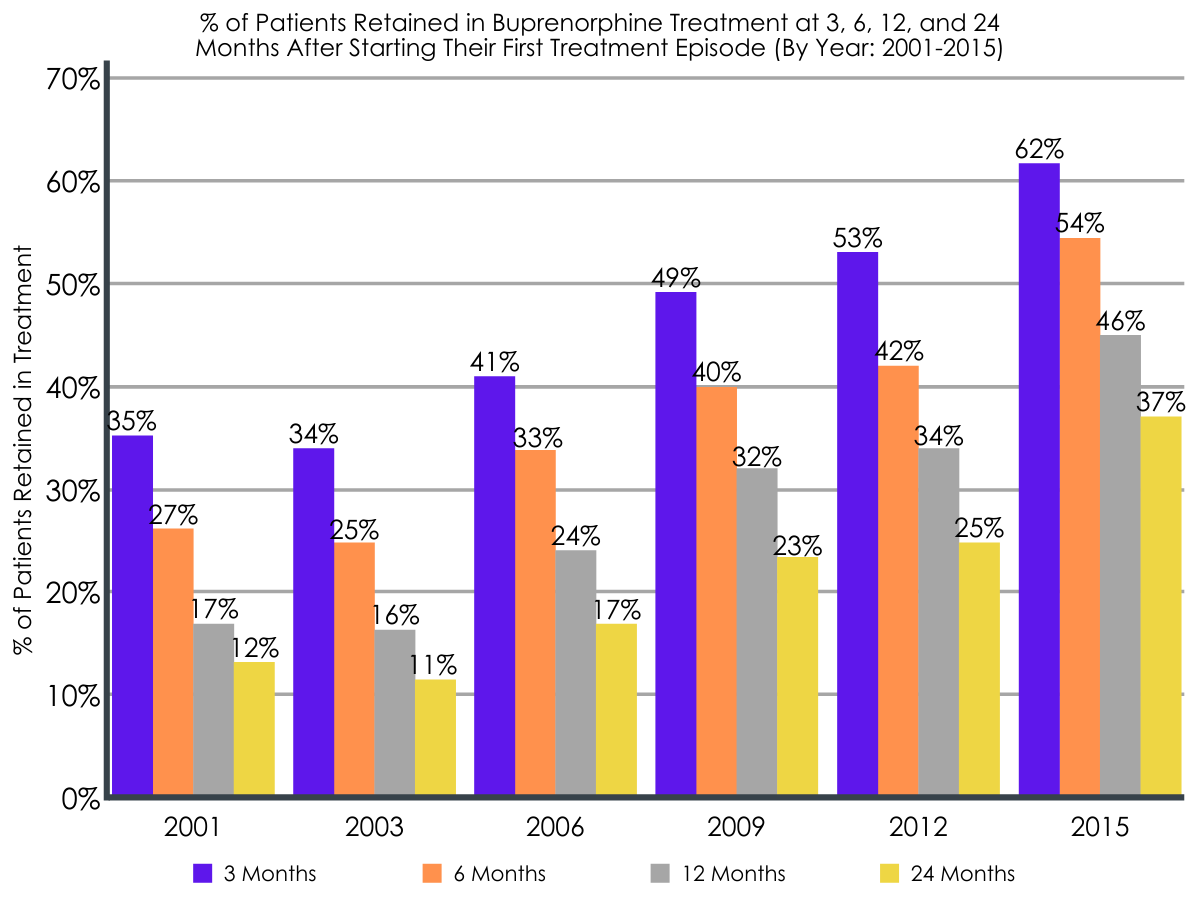
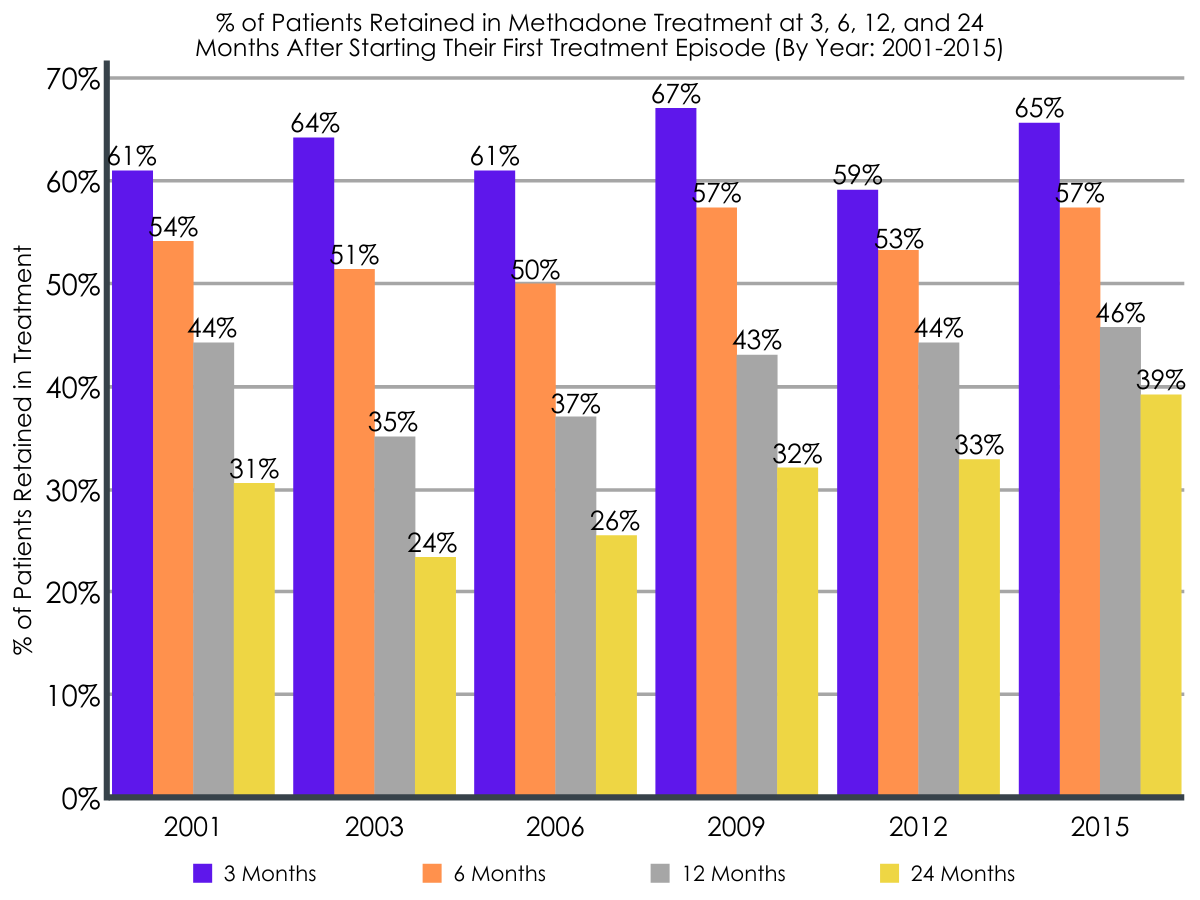
The median duration of patient’s first methadone treatment episode remained relatively stable from 2001-2015, at ~226 days. The percentage of patients retained in methadone treatment at 3, 6, 12, and 24 months also remained consistent from 2001 to 2015 (e.g., 12-month retention = 44% in 2001 vs. 46% in 2015). On the other hand, buprenorphine treatment duration increased over time, with median treatment duration increasing from 19 days in 2001 to 269 days in 2015. Similarly, the percentage of patients retained in buprenorphine treatment at 3, 6, 12, and 24 months also increased from 2001 to 2015 (e.g., 12-month retention = 17% in 2001 vs. 46% in 2016).
The type of medication was related to longer treatment retention.
Better treatment retention was seen among patients receiving methadone and patients receiving treatment in criminal justice systems. Across the entire study timeframe, patients receiving buprenorphine were 1.6 times more likely to drop out of treatment than patients receiving methadone. In any given three-year period (i.e. 2001-2003, 2004-2006, 2007-2009, 2010-2012, 2013-2015), and controlling for patient and prescriber characteristics, patients starting buprenorphine for the first time were 1.2 to 1.7 times more likely to discontinue treatment than patients starting methadone. However, this difference reduced over time, with odds of discontinuation for buprenorphine patients being 1.6 times higher between 2001 and 2003, and 1.2 times higher between 2013 and 2015, relative to methadone patients. Individuals who received treatment in a public health setting were also 1.7 times more likely to discontinue treatment than patients receiving medication in criminal justice settings (e.g., prison).
At the medication prescriber level, more experience mattered.
Better treatment retention was seen among patients whose prescribers had more experience with prescribing opioid agonist treatment. Controlling for other patient and treatment variables, patients whose prescribers had less experience prescribing opioid agonist treatment were more likely to discontinue treatment. For example, prescribers with 5 years of experience reduced the odds of treatment drop out by 12% when they were compared to those with less than 1 year of experience. A smaller difference was observed when prescribers with more years of experience were compared (e.g., 3% reduced odds with 14 years vs. 9 years of prescriber experience).
Certain Patient characteristics were associated with longer treatment retention.
Older patients, patients without a past-year psychotic disorder or criminal offences, and those with a past-year mood or comorbid substance use disorder were more likely to be retained in treatment. Odds of treatment discontinuation were significantly (~1.1 times) higher in younger patients (ages 29 and younger), those with a past year psychotic disorder, and patients with 4 or more criminal offences in the year prior to starting their first treatment episode, relative to patients aged 35 years and older, patients without a psychotic disorder, and patients without recent criminal offences, respectively. Individuals with a past-year mood disorder or a comorbid substance use disorder (in addition to opioids) were also 9% and 5% less likely to drop out of treatment than those without these disorders, respectively.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study helps us better understand the effects of integrating buprenorphine into treatment options at opioid treatment programs, as well as the factors that influence treatment retention versus drop out.
Consistent with prior research conducted in Australia and findings from systematic reviews, the current study revealed that treatment retention was lower for buprenorphine than methadone among first time patients, but this was largely due to the new implementation of buprenorphine in these Australian treatment programs in 2001. More specifically, by 2015, rates of retention were generally similar for methadone and buprenorphine (e.g., 24-month retention in 2015 was 39% for methadone and 37% for buprenorphine). This could be explained by a change in buprenorphine treatment approaches over time, shifting from a focus on detoxification or short-term management, as opposed to long-term treatment, or by the fact that prescribing guidelines concerning effective doses of buprenorphine have improved over time. Indeed, systematic reviews have shown that retention in treatment is similar with methadone and buprenorphine at adequately high doses. Prescribers’ experience with buprenorphine after its initial release in Australia in 2001 may have also increased over time, resulting in improved patient experience and retention.
Importantly, prescribers who have more experience in treating patients with these agonist medications were more likely to have patients who were retained in treatment. Thus, to the extent that greater experience is indicative of a greater understanding of the medication and best practices to retain patients in such treatments such experience may well influence a patient’s decision to continue or discontinue medication treatment. Prescriber mentoring and education might help bring new prescribers up to speed and help them adapt to individual patient needs, which could ultimately enhance patient satisfaction and treatment retention.
With respect to individual patient characteristics, poorer retention was seen among patients who were younger, with a past-year psychotic disorder, and with more pronounced criminal offence histories just prior to treatment.
Findings concerning the influence of age are commonly observed and prior research suggests emerging adults are more likely to drop out of treatment than older adults, perhaps reflecting a greater commitment to treatment among older adults. Increased maturity with age, an enhanced desire to finally be done with battling a life-long substance use disorder, and the incompatibility of the substance-use lifestyle with older age could all contribute to the enhanced motivation to commit to change among older adults. Consistent with the current outcomes, psychosis is known to have a negative impact on multiple treatments, including substance use disorder treatment. The complicating factors of psychotic thought disorder as well as potentially anti-psychotic medication use could interact with and impede retention in medication treatment for opioid use disorder. This is an important population that requires greater attention to improve outcomes and quality of life. Interestingly, individuals with past-year mood disorders were more likely to remain in treatment relative to those without mood disorders. This could be a result of the psychological benefits seen in patients undergoing agonist treatments. For example, although psychiatric disorders can negatively impact opioid use disorder, mood disorder symptoms are shown to have limited to no impact on retention in opioid agonist treatment, and psychiatric symptoms are shown to improve during the course of medication treatment. At least some of these mood disorder symptoms also are induced by or are a part of the opioid use disorder. Thus, perhaps the improvement in mood disorder symptoms as individuals engage with medications for opioid use disorder further encourages patients to remain on the medication, or maybe the additional clinical attention allows patients to get the other treatments they need to manage their mood disorders alongside addiction treatment.
While the exact reasons for this finding are uncertain, psychiatric comorbidities commonly occur with opioid use disorder. This study further suggests that individuals with these comorbidities can be retained in treatment just as well as those without psychiatric comorbidities, with the exception of psychosis, which might introduce additional complications that require greater effort from the treatment provider, family, and friends to help the patient remain in treatment.
Moreover, comorbid substance use disorders were associated with better treatment retention, which could suggest enhanced treatment motivation among patients with more severe psychiatric histories. The improved retention in opioid agonist treatment seen among those in criminal justice settings is likely a result of medication delivery in a controlled environment, and further highlights the many benefits of providing opioid agonist treatments in correctional facilities, which are seen in other studies.
- LIMITATIONS
-
- This study was conducted in Australia and additional research is needed to determine if these findings are replicable in other countries with different healthcare systems and cultural/professional/personal attitudes toward medication treatments for opioid use disorder. In addition, this study is retrospective and relies on state records. Therefore, additional prospective research is needed to better understand the factors influencing treatment retention.
- All participants had started treatment for the first time at the start of the study timeframe. Additional research is needed to examine retention rates and factors influencing them among patients who have more extensive treatment histories and multiple failed treatment attempts.
- The medication dose of opioid agonist treatments was not available in these data. Given the importance of dose on treatment retention, additional research is needed. The extent to which financial and logistical barriers influence retention was not examined in this study and requires additional research.
- There is an assumption that MAT discontinuation in this study was a negative outcome when it is possible that medication discontinuation could have been due to patients doing well – potentially in full sustained remission and functioning at a high level. There could have been patient-centered negotiated discussions with providers regarding clinically supported medication discontinuation. Further research is needed to clarify this possibility.
BOTTOM LINE
Buprenorphine retention was lower than methadone retention at the time of buprenorphine’s introduction in Australian opioid treatment programs, though buprenorphine retention increased in the years since it was introduced and ultimately looked similar to methadone retention by 2015. Thus, facilities looking to start buprenorphine prescribing may need additional guidance at the time of program startup to ensure best practices for retaining patients in treatment. The results of this study also reveal several factors related to unsuccessful retention in opioid agonist treatment, including patient (younger age, not having a mood disorder or comorbid substance use disorder, having a psychotic disorder, presence of past-year criminal offences), treatment setting (receipt of treatment in public health settings, as opposed to criminal justice settings), and prescriber (having a provider with fewer years of prescribing experience) characteristics. These outcomes complement and extend previous research, identifying potential barriers to treatment retention that can be addressed to better ensure the successful treatment of patients engaging in opioid agonist treatment.
- For individuals and families seeking recovery: Early discontinuation of opioid use disorder medication treatment can put patients at risk of relapse and overdose. Identifying the factors that influence patient’s retention in treatment can better inform best practices for improving patient success. This study suggests better retention in treatment among patients whose providers have more years of prescribing experience. Patients who have an increased risk of dropping out of treatment might consider finding a more experienced prescriber. According to this study, patients may be at increased risk of drop out if they are younger, have a psychotic disorder, have been charged with a criminal offense in the past year, or if they do not have a co-occurring mood or substance use disorder. Interested individuals should speak to their healthcare providers to learn more about these medications and determine which one might be best for them and enhance their chances of retention.
- For treatment professionals and treatment systems: Low retention rates in buprenorphine and methadone treatment are an ongoing issue. This study suggests that patient, treatment, and prescriber characteristics can influence retention. More specifically, prescribers with more experience prescribing opioid agonist treatments appear to be better at retaining patients in treatment. Peer mentoring and guidance of newer prescribers by more experienced ones may help to enhance patient outcomes. Patients who are younger, patients who have a psychotic disorder, patients who have been charged with a criminal offense in the past year, and patients who do not have a co-occurring mood or substance use disorder may be at increased risk of treatment drop out, suggesting patients with any one of these characteristics may need more support to remain in treatment and reap the benefits of these lifesaving medications. Given that this study was conducted in Australia, additional research will help inform whether these predictors of treatment retention are consistent across different countries. Also, it is unclear whether there was successful discontinuation of a medication due to patient preference after demonstrating longer term successful full sustained remission and psychosocial stability. It is possible that at least some of these patients who discontinued were doing well and, in consultation with their provider, were able to successfully transition to non-medication use.
- For scientists: Additional research is needed to replicate and extend these findings in different countries, and to identify additional predictors of retention across various populations and in various treatment settings. Investigation of all available medications (including antagonists and extended-release versions of these medications) could help further our understanding of the factors influencing treatment drop out and help address ongoing difficulties retaining patients in opioid agonist treatment programs. Prospective investigation of present-day patients with longer follow-up periods will also inform the relationship between treatment duration and long-term recovery outcomes. Also, it is unclear whether there was successful discontinuation of a medication due to patient preference after demonstrating longer term successful full sustained remission and psychosocial stability. It is possible that at least some of these patients who discontinued were doing well and, in consultation with their provider, were able to successfully transition to non-medication use.
- For policy makers: There are many factors that have the potential to impact patient retention in opioid use disorder medication treatment. This study reveals a number of patient, treatment, and prescriber characteristics associated with retention, that can be leveraged to improve retention rates in opioid treatment programs. More specifically, this study further highlights the benefits of providing medication treatment in correctional facilities. It also suggests enhanced retention with more experienced prescribers, revealing a need to support and guide less experienced providers. Patient characteristics (e.g., mental health, age, etc.) also appeared to influence retention in medication treatment and additional prospective studies are needed in other countries to better characterize predictors of treatment retention, as well as other treatment and recovery outcomes. Doing so can help guide clinical practice and address ongoing issues surrounding uptake of and retention in medication treatment.
CITATIONS
Bharat, C., Larney, S., Barbieri, S., Dobbins, T., Jones, N. R., Hickman, M., . . . Degenhardt, L. (2021). The effect of person, treatment and prescriber characteristics on retention in opioid agonist treatment: a 15‐year retrospective cohort study. Addiction, 116(11), 3139-3152. doi: 10.1111/add.15514

