Helping to secure stable housing first among homeless individuals can improve mental health and quality of life
Homelessness remains a pervasive public health issue in Western countries, particularly among adults with a serious mental illness, many of whom have co-occurring substance use disorders. In the absence of stable housing, which is regarded as a fundamental human need, overall health and recovery outcomes are compromised. In this randomized controlled trial of a “housing first” intervention, researchers provide evidence of the significant benefits of providing housing and housing assistance to individuals with serious mental illness.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Homelessness remains a significant public health issue in Western countries. Individuals with mental illness are far more likely to experience homelessness, and homelessness, in turn, can significantly undermine recovery. The majority of existing housing programs require mental health or substance use treatment and stabilization as a precondition to receipt and maintenance of housing. The authors of this study conducted a randomized controlled trial of a Housing First intervention, coupled with Assertive Community Treatment, to evaluate the effect of this intervention on housing rates, health, and quality of life among individuals with serious mental illness and high rates of substance use.
HOW WAS THIS STUDY CONDUCTED?
For this study, the authors conducted a randomized controlled trial, comparing Housing First plus Assertive Community Treatment versus treatment as usual (TAU), among 201 Canadian residents of a rural city with serious mental illness determined by a brief DSM-IV diagnostic screening interview (i.e., major depressive disorder, manic or hypomanic episode, posttraumatic stress disorder, psychotic disorder). Participants completed follow-up questionnaires and interviews with study staff at baseline and after three, nine, 15, and 21/24 months (select participants interviewed at month 21 instead of 24 due to scheduling and resource conflicts). Self-report outcome measures included housing stability (in the past three months), perceived housing quality, community functioning, self-rated health status, mental health symptoms and severity, substance use problems, quality of life, physical integration (i.e., community involvement and participation activities), and psychological integration (i.e., degree of integration and sense of belonging with their community). The primary outcomes of interest to these researchers were the percentage of time spent stably housed, number of moves, proportion of individuals stably housed for six months or longer, housing quality, and community functioning following receipt of intervention. The remaining outcomes were considered secondary. Of note, authors analyzed differences in “recovery,” meaning increased confidence and hope, ability and willingness to ask for help from others, goal setting and orientation toward the future, healthy reliance on others, and not being “dominated” by mental health symptoms.
The researchers were specifically interested in evaluating the effects of their combined Housing First plus Assertive Community Treatment approach. Housing First entails helping individuals secure housing, move in as soon as possible, and providing renting supplements – so that individuals are not paying more than 30% of their income toward rent – to allow them to compete for private market housing options. Housing First also includes support for moving in to and furnishing the home, with no preconditions that individuals seek treatment or demonstrate stability prior to securing housing. Housing First includes intensive support from an Assertive Community Treatment team and Intensive Case Management to support harm reduction, recovery, and empowerment. With this approach, housing and treatment services are provided by separate agencies (to ensure privacy and autonomy), 24/7 access to treatment and related services, but no requirement of treatment or medication use. The Assertive Community Treatment philosophy also embodies a person-centered approach that emphasizes increasing individual autonomy; self-efficacy (to meet their basic needs); and enhance their social skills, employability and occupational skills, and quality of life. This treatment was compared to TAU, which in this study included access to “existing health and social services” in the region; however, the region did not have access to Housing First or other supportive housing services prior to this intervention.
The sample in this study was 18 and older, predominantly male (65%), White/Caucasian (80%), single (unmarried; 66%), and homeless (56%) or “precariously housed” (44%). Educational status was variable, with the average having completed some high school or completing high school. Further, 71% screened positive for major depressive disorder, 17% with a manic or hypomanic episode, 45% with PTSD, 28% with panic disorder, 13% with a mood disorder (with psychotic features), 23% with a psychotic disorder (e.g., schizophrenia), 16% with an alcohol use disorder, and 53% with some other substance use disorder. The vast majority also had one or more co-occurring health condition(s).
WHAT DID THIS STUDY FIND?
Individuals receiving Housing First plus Assertive Community Treatment were able to secure stable housing more quickly, sustain housing for longer periods of time, and provided higher housing quality ratings. Individuals who received Housing First plus Assertive Community Treatment also reported higher quality of life, perceived recovery, and feelings of belongingness and integration with their communities.
Contrary to expectation, the researchers did not find a difference between treatment groups on outcomes of mental health severity, substance use, or overall health status; rather, both groups improved similarly over time. This may point to the need for intervention refinement, which may include greater integration of evidence-based mental health and substance use treatment services as a complement, but not a precondition, to stable housing.
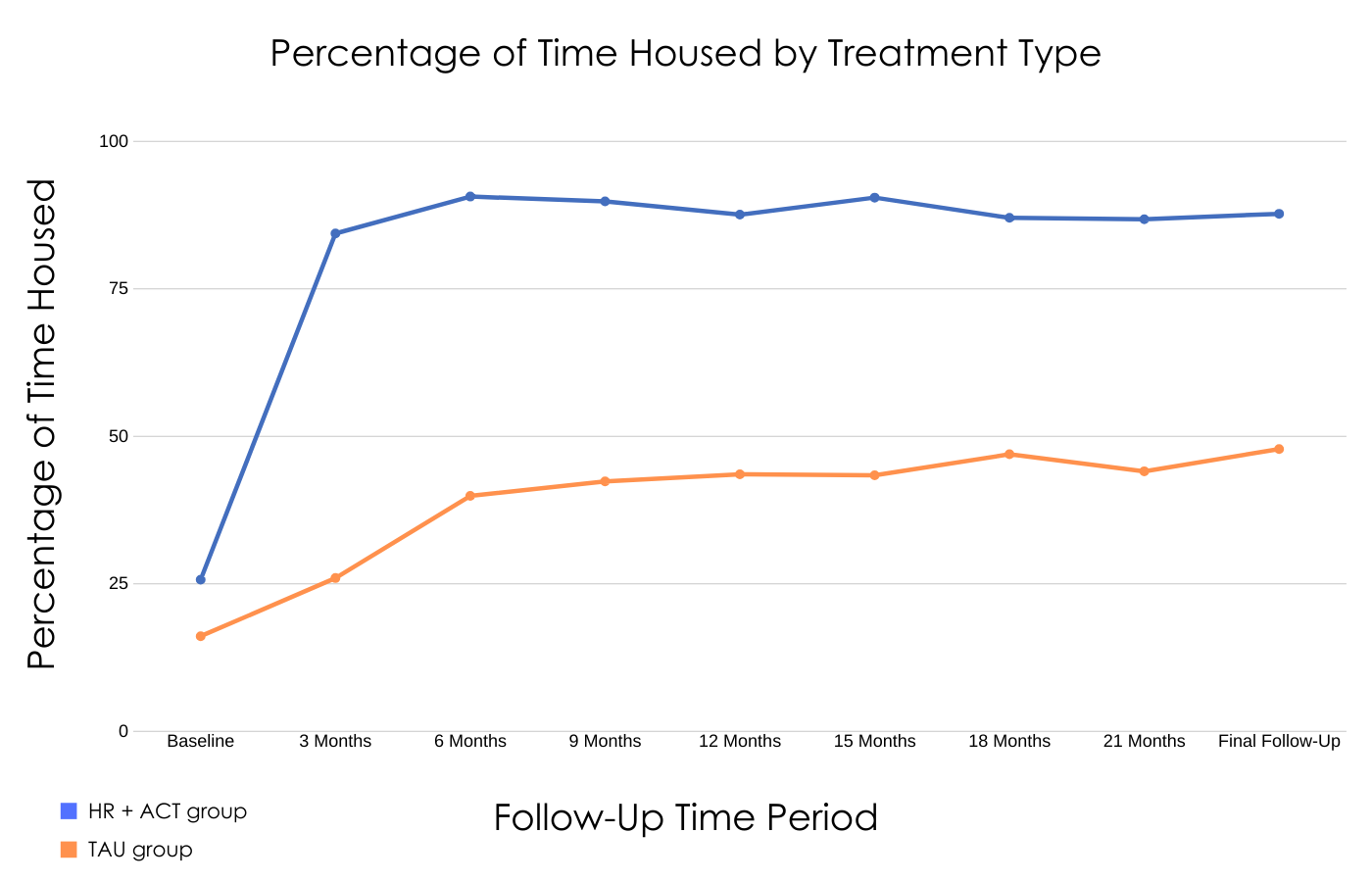
Figure 1. Depiction of the percentage of time housed in the last three months among individuals with serious mental illness and who were experiencing homelessness at the start of the study.
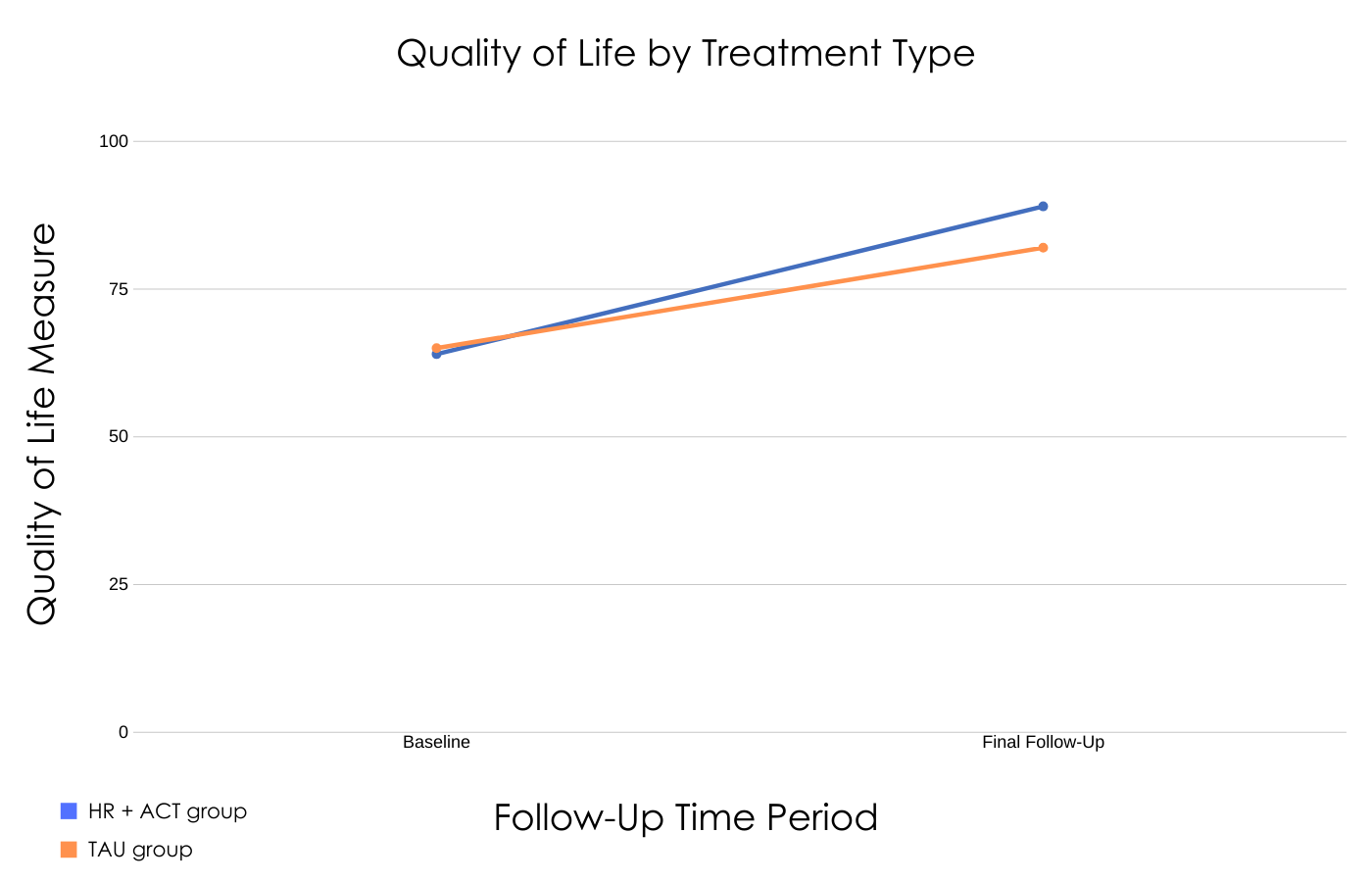
Figure 2. Depiction of the Quality of Life at baseline and final follow-up for individuals who received Housing First plus Assertive Community Treatment versus those who received treatment as usual.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study is important because it demonstrated that Housing First and Assertive Community Treatment improved individuals’ housing quality, stability, and community involvement and sense of belonging over time. The significant increase in stable housing by three months among individuals receiving Housing First plus Assertive Community Treatment is particularly noteworthy. Earlier receipt of housing confers an added advantage to these individuals, who, once housed, have an increased ability to seek and benefit from additional treatment to promote long-term mental health recovery. Although the researchers did not find that Housing First plus Assertive Community Treatment produced better mental and physical health outcomes directly relative to the comparison condition, receipt of stable housing and increased quality of life may promote overall health and wellbeing over time, and certainly promote a foundation upon which further recovery is possible.
Consistent with previous Housing First initiatives, and in light of residual mental health, substance use, and physical health concerns among the participants in this study, future work should incorporate evidence-based medical and mental health services as well, which have been shown to be effective among individuals experiencing homelessness. These interventions could include specific substance use and harm reduction strategies and utilization of resources and support offered through peer-led Recovery Community Centers to reduce rates of substance use, which remain prevalent among this vulnerable population. In addition, given the lack of awareness of these services and practical barriers to seeking or benefitting from them, additional research and development is needed to promote linkage to these services from established medical services (e.g., primary care, inpatient hospitals).
- LIMITATIONS
-
- The authors inability to “blind” participants to the different study conditions.
- Higher rates of participant dropout from the TAU condition (75% completion vs. 89% in the Housing First and Assertive Community Treatment condition).
BOTTOM LINE
- For individuals and families seeking recovery: Stable housing is an important factor in terms of individuals’ sense of safety, security, quality of life, and overall mental and physical health. In this study, researchers studied the practice of Housing First plus added Assertive Community Treatment, which emphasizes finding safe housing as the priority, without requiring concurrent treatment or that individuals demonstrate stable mental and physical health to maintain their housing. Individuals are encouraged to speak with their providers about housing resources if needed, and consider seeking out mental health and substance use treatment services to complement stable housing and promote long-term recovery. Housing alone may not be sufficient to address the range of concerns that individuals experiencing homelessness may face; individuals with serious mental illness would still likely benefit from additional evidence-based mental health and substance use treatment. Interventions like Cognitive Behavioral Therapy and Contingency Management have been shown to be effective for individuals with mental and substance use disorders and can be flexibly applied across a variety of clinical settings to meet the needs of diverse patient populations. Additional support options include peer-operated Recovery Community Centers, which serve as local and community-based recovery support to help individuals build a recovery community, gain information, and receive help in accessing services.
- For treatment professionals and treatment systems: Housing First plus Assertive Community Treatment is an intervention that provides housing support and financial assistance to individuals with serious mental illness. In this study, individuals who received Housing First plus Assertive Community Treatment were more likely to secure stable housing and reported significant improvements in their sense of community belonging, perceived recovery, and quality of life. Although individuals who received Housing First plus Assertive Community Treatment did not differ from individuals in the TAU condition regarding mental and physical health or substance use severity, receipt of housing could promote treatment seeking for these concerns. This suggests that additional work is needed to integrate mental health and substance use treatment services with housing interventions. In the meantime, providers should consider referring patients to these services as a complement to receipt of stable housing to promote long-term recovery. Unfortunately, local resources vary considerably across cities, states, and countries, and access to affordable housing may or may not be readily available to individuals with serious mental illness. It is recommended that additional resources be made available to patients, and/or information about how these individuals can get in touch with agencies that can help them secure stable housing, as well as mental health and substance use treatment services if needed.
- For scientists: Individuals who benefitted from Housing First plus Assertive Community Treatment were able to secure housing quicker, maintain stable housing for longer periods of time, and reported greater quality of life and perceived recovery. The fact that the researchers did not find differences between treatment groups regarding physical and mental health or substance use outcomes indicates the need for follow-up research and intervention development. Intuitive options for Housing First intervention refinement would include increasing access to integrated and evidence-based mental health and substance use treatment services. That is, while housing represents one important aspect of recovery for homeless individuals with serious mental illness, additional intervention support may be needed to address the secondary outcomes measured but not improved by the Housing First intervention implemented in this study. It is also possible that longer follow-up periods would allow researchers to observe differences that take longer to manifest, or that medical and mental health treatments ought to be incorporated or made available in addition to Housing First plus Assertive Community Treatment. Recent research has demonstrated that even brief interventions can be highly effective for individuals experiencing homelessness. The brief format of such interventions makes it possible to integrate these treatments across a variety of existing services or settings. Therefore, research that examines whether active linkages to empirically supported substance use and mental health services provide additional benefit relative only to service access, as was the case in this study. Cost effectiveness studies, if in support of Housing First initiatives, may also help make the case to policy makers that funding for such initiatives pays off in the long run. From a methodological perspective, it should work to bolster follow-up among vulnerable populations, such as those experiencing homelessness. Future research would also benefit from more objective measures of housing attainment, stability, and other physical and mental and substance use outcomes (e.g., diagnostic interviews, urinalysis).
- For policy makers: Housing First initiatives are associated with receipt and maintenance of stable housing and can be extremely beneficial to recipients and their families. In contrast to other housing initiatives, there were no preconditions associated with receipt of housing with Housing First plus Assertive Community Treatment (e.g., no treatment or symptom stabilization requirement). Such preconditions may not be necessary to maintain stable housing, and receipt of housing may itself promote stabilization among recipients. At the same time, secondary mental health and substance use outcomes were not positively impacted directly by this intervention, suggesting that additional policy action, funding, and intervention development are needed. Stable housing represents a basic need that, if secured, provides individuals with opportunities to pursue other recovery-oriented services, such as medical and mental health treatment. It is also true that while beneficial, housing first interventions alone may not be sufficient. Increasing funding and support for research and development that combines housing assistance with evidence-based mental health and substance use treatment could significantly improve outcomes and recovery potential among individuals with serious mental illness who also experience homelessness.
CITATIONS
Aubry, T., Bourque, J., Goering, P., Crouse, S., Veldhuizen, S., LeBlanc, S., . . . Bradshaw, C. (2019). A randomized controlled trial of the effectiveness of Housing First in a small Canadian city. BMC Public Health, 19, 1154-1168. doi: 10.1186/s12889-019-7492-8

