Addiction treatment may protect against the risk of opioid use disorder on suicidal behavior
The presence of co-occurring mental health conditions such as depression is high among individuals with substance use disorders, specifically those with opioid use disorder. Co-occurring mental health conditions and opioid use disorder may both increase the risk of suicidal behaviors. This study examined whether opioid use disorder is associated with increased risk for suicide among US adults and if receiving addiction, mental health, or both types of treatment might buffer against any additional risk.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
There were 73,000 overdose deaths involving opioids in 2021 and 1.2 million adults attempting suicide in 2020. Theories about the brain and behavior suggest there may be a link between these two leading causes of death. Recent 2020 data, based on DSM-V diagnostic criteria, reveals that 6.7% (17 million) adults in the US had a co-occurring substance use disorder and mental illness in the past year. Those with an opioid use disorder may be more likely to have other mental health conditions. National survey results found that among individuals with opioid use disorder, 36% had a mild or moderate mental illness and 24% had a serious mental illness (any mental, behavioral, or emotional disorder that interfered with or limited one or more major life activities). However, the prevalence of suicidal behavior among individuals with opioid use disorder is unknown. Understanding the nature of co-occurring opioid use disorder and suicidal behavior may help improve our clinical and public health responses to these two preventable causes of death and their related harms.
Previous research has found that the presence of a substance use disorder is a risk factor for suicide. Furthermore, the frequency of opioid use is linked with suicidal behavior as well as other risk factors for suicide (e.g., depression). People who use opioids are approximately 14 times more likely to die by suicide compared to the general population. Unfortunately, millions of individuals do not receive behavioral health treatment for their substance use disorder or their mental health condition. The lack of services and/or linkage to services may contribute to the harms from opioid use disorder and suicidal behavior. Providing the appropriate behavioral health treatment, substance use treatment, mental health treatment, or both, may help support individuals with co-occurring opioid use disorder and mental health conditions and, in turn, reduce their risk for suicidal behaviors. This study conducted a cross-sectional analysis of nationally representative survey data to identify the prevalence of suicidal behavior among adults with an opioid use disorder and if different types of behavioral health treatment are associated with a reduced risk of suicidal behaviors.
HOW WAS THIS STUDY CONDUCTED?
This cross-sectional study combined results from 2015-2018 of the National Survey of Drug Use and Health (NSDUH) to identify the prevalence of suicidal behaviors among adults that meet criteria for opioid use disorder in the past year and if the prevalence differed among those that attended substance use treatment, mental health treatment, both, or no treatment (N = 156,000).
The National Survey on Drug Use and Health is a nationally representative survey of the general, non-institutionalized, population in the United States conducted annually by the Substance Abuse and Mental Health Service Administration (SAMHSA). This survey collects detailed information on drug use, mental health, treatment utilization, and a range of other health-related issues. The primary outcome drawn from the NSDUH for the present study is suicidal behavior. Participants that reported thoughts ending their life, made a plan to kill themselves, or attempted to kill themselves in the last 12 months were categorized as having suicidal behavior. The key independent variable used is whether an individual meets criteria for an opioid use disorder or not. The receipt of behavioral health treatment was classified into four mutually exclusive categories: substance use disorder treatment only, mental health treatment only, both substance use disorder and mental health treatment, and no substance use disorder or mental health treatment in the past 12 months. Substance use disorder treatment could be inpatient or outpatient and includes services received at a mental health center, hospital, rehab facility, physician’s office, or a substance related emergency room visit. Of note, treatment did not include community-based mutual-help or other recovery support service attendance. Mental health treatment includes inpatient and outpatient services as well as the use of psychotropic medication. The researchers also included whether an individual experienced a major depressive episode in the past 12 months. Substance use disorder and mental health condition criteria were based on DSM-IV diagnostic criteria.
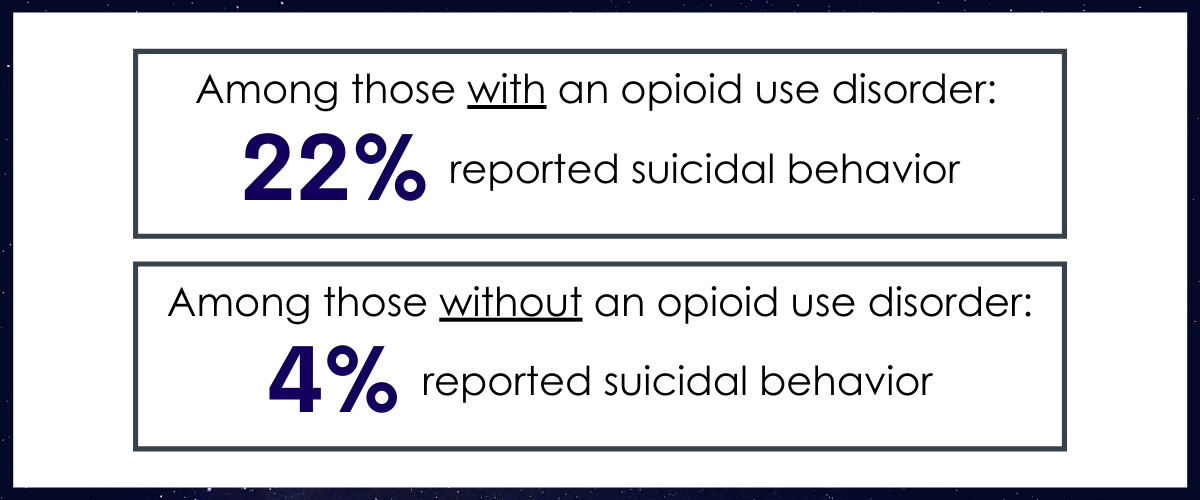
The National Survey of Drug Use and Health is nationally representative, so the demographics overall and specific to opioid use disorder reflect the demographics in the US population. Among individuals with an opioid use disorder, 22% reported suicidal behavior compared to 4% of those without an opioid use disorder. Similarly, 27% of those with an opioid use disorder had a major depressive episode in the last 12 months while only 6% of those without an opioid use disorder did. A larger proportion of people with an opioid use disorder reported attending both substance use disorder and mental health treatment compared to people without an opioid use disorder. Compared to those without an opioid use disorder, a larger proportion of individuals with an opioid use disorder were white (71% vs 63%), male (56% vs 48%), unemployed (13% vs 5%), and uninsured (19% vs 11%). A larger proportion of adults with an opioid use disorder also reported having fair or poor health compared to those without an opioid use disorder (30% vs 13%).
WHAT DID THIS STUDY FIND?
Adults with opioid use disorder have higher odds of suicidal behavior.
After controlling for risk and protective factors, adults with opioid use disorder had odds of suicidal behavior 2.90 times that of adults without opioid use disorder. Controlling for factors such as major depressive disorder, gender, age, race, education, family income, and self-rated health allowed the researchers to better isolate the association between opioid use disorder and suicidal behavior. For example, these high odds of suicidal behavior take into consideration the strong link between major depressive episode and suicide. Those with a major depressive episode had odds of suicidal behavior nearly 13 times that of those that did not experience a major depressive episode.
Substance use disorder treatment was associated with stronger reductions in suicide risk than mental health treatment.
Among the 47% of adults with an opioid use disorder that received some form of treatment in the past 12 months, all had lower odds of reporting suicidal behavior compared to receiving no treatment. Out of the 47% adults that had treatment, 28% had only mental health treatment; 11% had only substance use disorder treatment; and 18% had both mental health and substance use disorder treatment. Receiving mental health treatment was associated with 5% lower odds; receiving substance use disorder treatment was associated with 49% lower odds; and receiving both mental health and substance use disorder treatment was associated with 28% lower odds. Overall, then, those that received substance use disorder treatment were the least likely to report suicidal behavior in the last 12 months.
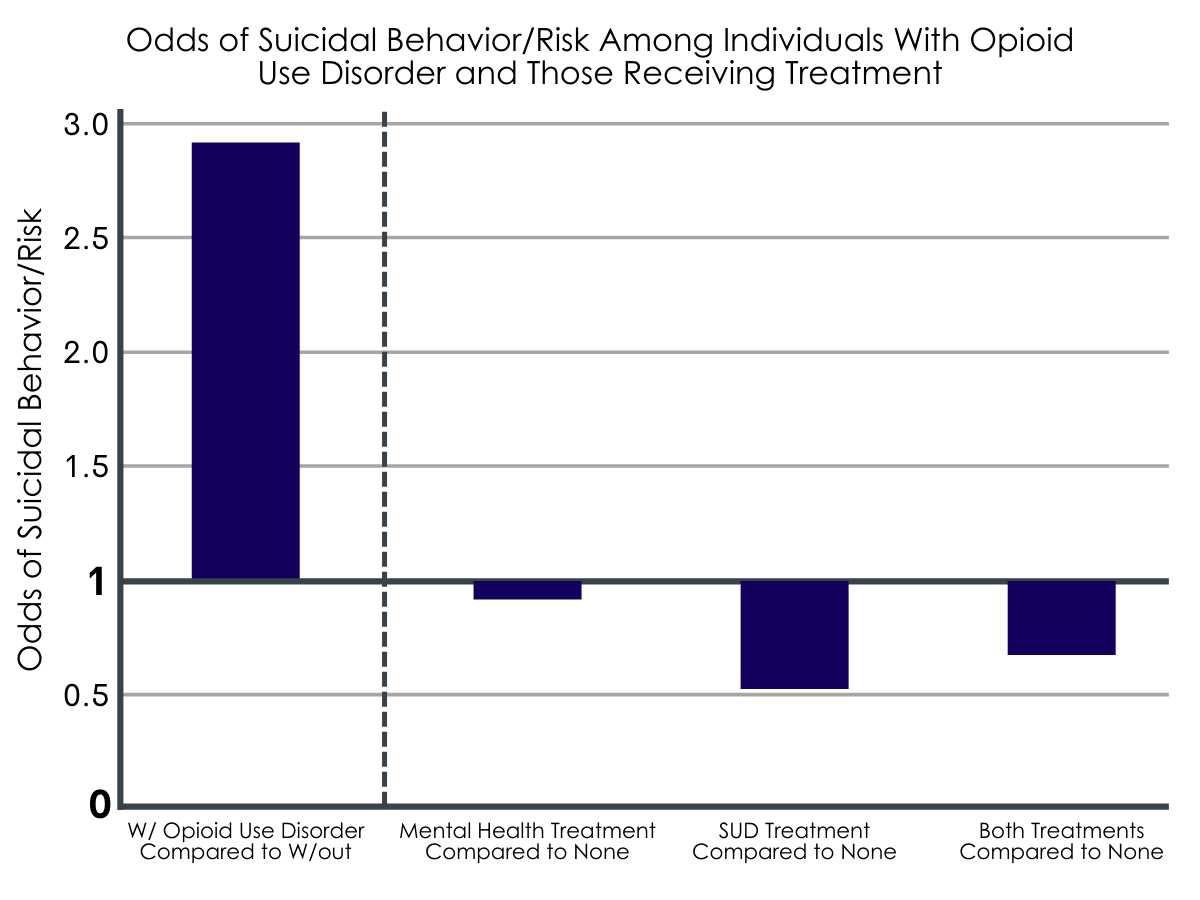
Odds of suicidal behavior/risk. Individuals who had opioid use disorder had higher odds of suicidal behavior compared to those without opioid use disorder, but among those with opioid use disorder, individuals receiving all forms of treatment had lower odds of suicidal risk compared to those not receiving treatment. In this instance, odds above 1 indicate increased risk, while odds below 1 indicate decreased risk, while any odds of 1 would indicate no change.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
Drug-related overdose and suicide are leading causes of death in the United States. In 2020, the National Survey of Drug Use and Health identified over 3 million adults meeting criteria for opioid use disorder and over 12 million adults that had thoughts of suicide. Understanding the connection between opioid use disorder and suicide may help reduce harm and prevent unnecessary death. Although prior literature has identified a link between opioid use and suicidal behaviors, less is known about the relationship between suicidal behavior and opioid use disorder specifically. Researchers in this study found that adults with opioid use disorder were much more likely to report suicidal behaviors in the past year. With odds of suicidal behavior approximately 3 times that of adults without opioid use disorder, those with opioid use disorder appear to be at a heightened risk. It may also be that those with mental health conditions, including suicidal behaviors, may be self-medicating and in need of additional tools to address their mental health. Creating protocols that couple opioid use disorder and suicidal behavior screenings may help identify the large subset of adults with co-occurring opioid use disorder and suicidal behaviors.
Although there is a high prevalence of co-occurring substance use and mental health conditions, only a fraction of adults receive any behavioral health treatment. This study found that 47% of adults with opioid use disorder received substance use disorder treatment, mental health treatment, or both in the last year. Furthermore, the researchers found that those who received substance use disorder treatment were much less likely to report suicidal behaviors. Compared to receiving no treatment, adults that receive substance use disorder treatment had 49% lower odds of reporting suicidal behaviors; adults that received mental health treatment or both mental health and substance use disorder treatment had 5% and 28% lower odds respectively compared to no treatment. Substance use disorder treatment may help reduce suicidal behavior by first focusing more on opioid use, which might facilitate the skill development and biophysiological recovery needed to then reduce suicidal thoughts and behaviors. It is possible also that the suicidal behavior may be a natural consequence of an individual’s impaired ability to control the opioid use increasing hopelessness, thus, directly treating the opioid use disorder would naturally increase hope and optimism and decrease suicidal ideation.
To the extent that suicidal behavior and substance use disorder are somewhat independent entities, substance use disorder treatment might be used also to directly address both substance use and mental health. For example, such treatment may target suicidal thoughts independently, as these may be a trigger for opioid use. Mental health treatment, however, may prioritize suicidal behavior to the exclusion of opioid use, rendering it less protective overall if the opioid use disorder is the main driver of the suicidal thoughts and behavior. However, because the data reflect only a snapshot in time, we cannot determine if the opioid use disorder or suicidal behavior came first, the extent to which each exist independently of the other, or if receiving substance use disorder treatment itself is actually responsible for causing a reduction in suicidal behavior. It may be that those who are more likely to report suicidal behavior are less likely to attend substance use treatment. That said, because receiving treatment overall was associated with reduced suicidal behavior in those with opioid use disorder, it is unlikely that the research team found a stronger effect of substance use disorder treatment simply because the least severe individuals chose to attend addiction instead of mental health treatment. Whatever the case, careful ongoing assessment of the dynamic nature of the interplay between suicidal behaviors, other mental health symptoms, and opioid and other substance use is critical in clinical settings to understand more fully the patterns, drivers, and consequences, of all such symptoms and behaviors. Such careful assessment can then help inform which of these aspects in the clinical presentation need to be addressed with specific and independently focused treatments and which are likely to dissipate without independent focus (e.g., suicidal thoughts and impulses may fade quickly once the opioid use disorder is successfully treated).
- LIMITATIONS
-
- The study was cross-sectional and, therefore, any causal inferences should not be inferred without future longitudinal investigations.
- The study does not include completed suicide attempts, which likely produces conservative estimates of the association between opioid use disorder and suicidal behaviors.
- The NSDUH data used for this study does not include individuals currently institutionalized (in medical or justice-related institutions), which may also produce conservative estimates of the relationships found. Excluding institutionalized individuals might reduce the number of individuals with more severe behavioral health needs, which could alter the relationship found between opioid use disorder and suicidal behavior.
BOTTOM LINE
Researchers in this study found that adults in the United States with opioid use disorder were more likely to report suicidal behaviors compared to adults without an opioid use disorder. Additionally, they found that, when examining only adults with opioid use disorder, participants who attended substance use disorder treatment were much less likely to report suicidal behaviors compared to those that received mental health treatment, both mental health and substance use disorder treatment, and no treatment. Although the researchers present strong evidence of a link between opioid use disorder, suicidal behaviors, and substance use disorder treatment, the data is only a snapshot of the last 12 months. Future research is needed to determine how opioid use disorder and suicidal behaviors may be related. Additional research is also needed to explore how different types of behavioral health treatments can protect against any risk of opioid use on suicidal behavior as well as any risk of suicidal behavior on opioid use.
- For individuals and families seeking recovery: This study found a moderately strong relationship between opioid use disorder and suicidal behaviors. They also explored if the type of behavioral health treatment (substance use disorder, mental health, or both) changed this relationship. The researchers found that adults with opioid use disorder who received substance use disorder treatment only were least likely to report suicidal behaviors. If you or a loved one is experiencing substance use or mental health issues, it is likely beneficial to be screened for both. Similarly, receiving substance disorder treatment is unlikely to worsen mental health conditions and may help both opioid use disorder and suicidal behavior. Substance use disorder treatment often incorporates mental health difficulties, but mental health treatment does not always integrate substance use difficulties.
- For treatment professionals and treatment systems: Substance use and mental health screening are often part of routine care. This study found a relationship between opioid use disorder and suicidal behavior. It is very likely to help and unlikely to hurt if adults who screen positive for either opioid use disorder or suicidal behavior to be given additional screenings for either opioid use disorder or suicidal behavior. Additionally, the researchers found that substance use disorder treatment may be associated with reduced suicidal behaviors. which is consistent with other research showing substantial improvements in mental health functioning with SUD treatment.
- For scientists: This study conducted secondary data analyses of NSDUH 2015-2018 data to explore the relationship between opioid use disorder and suicidal behaviors and if behavioral health treatment modifies this association. Adults in the US with opioid use disorder had odds of suicidal behavior 2.90 times that of adults without opioid use disorder and that substance use disorder treatment alone was linked with the lowest prevalence of suicidal behavior. However, these findings were based on pooled, cross-sectional survey results. Future studies might also consider the severity of the opioid use disorder and suicidal behavior, length of treatment time, and treatment program characteristics.
- For policy makers: More research is needed to establish the exact nature of the connection between opioid use disorder and suicidal behavior as well as the role of behavioral health treatments. However, this study presents preliminary evidence of co-occurrence of opioid use disorder and suicidal behavior and that substance use treatment may be helpful for those individuals. Supporting research programs that explore substance use disorder and mental health condition co-occurrence is likely to further inform and enhance behavioral health treatments that in turn will improve health and functioning as well as reduce deaths in the United States.
CITATIONS
Ali, M. M. & Dubenitz, J. (2021). Suicidal behavior, opioid use disorder, and behavioral health treatment: Prevalence and correlates among adults in the United States 2015–2018. Journal of Substance Abuse Treatment, 130, 108413. doi: 10.1016/j.jsat.2021.108413

