Will Providing Housing for Homeless People With Mental Illness Reduce Daily Substance Use?
As the most prevalent psychiatric conditions among homeless individuals, substance use disorders can present as either a cause or an effect of chronic homelessness.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Homeless individuals with substance use issues and a co-occurring mental health disorder face additional obstacles when attempting the break the cycle of homelessness and addiction. While recovery is possible, effective interventions designed with this specific population in mind are needed.
One such approach, Housing First (HF), was created with the idea that housing in and of itself will dissuade people from continuing to use substances. This study evaluated the effectiveness of Housing First interventions for reducing substance use in Vancouver, Canada.
HOW WAS THIS STUDY CONDUCTED?
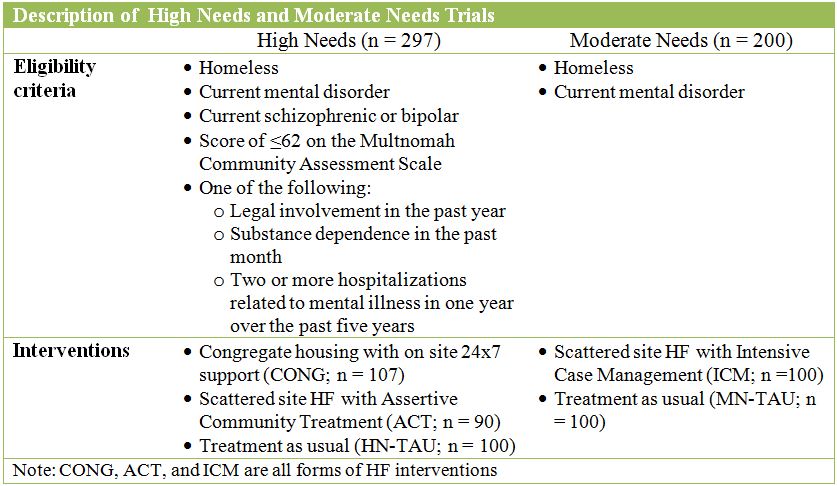
This study conducted two randomized controlled trials (RCTs) to investigate the impact of Housing First (HF) on daily substance use in 497 homeless individuals with at least one current mental health disorder. Homelessness was defined as absolute (i.e., having no place to live for more than a week) or having precarious housing (i.e., residing in marginal accommodation and having two or more periods of absolute homelessness). The trials were based on the needs of participants with 297 designated as high needs (HN) and 200 as moderate needs (MN) described in the table below. Interviews were conducted at baseline and every six months over the course of 24 months.
The interventions used the Housing First (HF) approach described here. Scattered site interventions (ACT and ICM) included an inventory of apartments from which participants could choose units. Participants in these conditions received in-home support and were required to meet with program staff weekly. The CONG condition was in a single building with 100 occupants in units without individual kitchens. The building offered amenities including a central kitchen, medical examination room, and recreation areas. Occupants could work part-time in the building (e.g., meal preparation) or in the community. Participants in ACT, ICM, and CONG were not required to comply with specific addiction treatment in order to maintain housing.
WHAT DID THIS STUDY FIND?
Describing patient characteristics at baseline, in the MN trial, prevalence of substance dependence varied from 51- 54%, and from 61-63% in the HN trial. Alcohol dependence varied from 24-25% and 21-26% for MN and HN, respectively. Daily substance use among participants in both trials ranged from 20-38%.
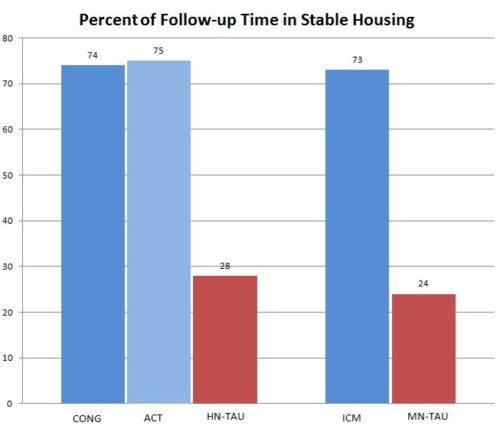
The results showed no significant differences between Housing First (HF) (i.e., CONG, ACT, and ICM) and Treatment-as-usual in both trials in terms of prevalence of less than daily substance use at 24-months and 12-months. The authors conducted a subgroup analysis restricted to patients who reported baseline substance use. This also resulted in no difference between Housing First and Treatment-as-usual indicating that including abstinent patients in the original analysis did not affect results. Participants in Housing First conditions spent a larger percentage of the 24-month follow-up period in stable housing than Treatment-as-usual as seen in the graph below.
While Housing First may not be sufficient for helping homeless individuals reduce daily substance use or achieve abstinence, other trials provided evidence for improved quality of life and reduction in criminal convictions. Provision of housing may help with other risks including accidents, injuries and deaths.
Finding housing may not have a positive impact on substance use in and of itself. Previous research has found that the duration of sobriety was longer for people living in supportive housing facilities that required drug screening. While having no drug screening or treatment requirements was necessary to measure Housing First’s effectiveness, individuals may need a motivating reason to stop using (e.g., weekly engagement in treatment to maintain housing). Adding contingency management could also potentially enhance response to Housing First initiatives.
WHY IS THIS STUDY IMPORTANT?
Homelessness is a major social problem that is strongly associated with substance use disorder and mental illness. Finding effective help for this vulnerable population is critically important and can save lives. Vancouver has one of the highest rates of homelessness among Canadian cities and it has been increasing over time.
Of the almost 3,000 homeless individuals in Vancouver, about half reported having an addiction and over 20% reported having a co-occurring mental disorder (see here). The results of this study may benefit other locations with similar rates of homelessness and addiction as programs will know if Housing First as it stands now is a worthwhile investment of resources.
Despite evidence supporting the effectiveness of two Housing First (HF) interventions—congregate housing with onsite 24×7 supports (CONG) and HF with Assertive Community Treatment (ACT)—no study has included both interventions in comparison to treatment as usual (TAU). Congregate housing in the CONG intervention refers to “project based” housing configurations where units are in a single building. The ACT condition features scattered site housing with an intensive, integrated system of mental health care delivery that addresses several areas of life including employment, relationships, and physical well-being (see here for more on ACT). Additionally, the authors included an intervention, HF with Intensive Case Management (ICM), for individuals whose needs were not severe enough to warrant ACT.
- LIMITATIONS
-
- This study from Vancouver, Canada consisted of participants who were mainly White, male, and over 40; results may not generalize to other geographic regions and populations.
NEXT STEPS
While there was no difference in daily substance use between HF and TAU for either trial, more research is needed into the mechanism behind this finding in order to improve future interventions to support homeless, mentally ill individuals with substance use disorders. Interventions offering support for abstinence and/or formal substance use disorder treatment, such as Contingency Management, in addition to housing should also be considered.
BOTTOM LINE
- For individuals & families seeking recovery: Housing will help on the pathway to recovery, but may not have a direct impact on substance use. Seek additional addiction and mental health services.
- For scientists: More research is needed to determine what additional services should be added to Housing First initiatives to help homeless individuals reduce substance use. Investigations of any community-level benefits that may be accrued by providing Housing First in various cities are needed. Cost savings may be obtained also by reduced burden on law enforcement and fewer accidents and injuries among homeless individuals.
- For policy makers: More affordable housing opportunities are needed to reduce rates of homelessness. Funding for supportive housing to address addiction and mental health needs is also necessary.
- For treatment professionals and treatment systems: Stable housing is important for the overall health of your patient. More formal treatment methods are still needed to address substance use.
CITATIONS
Somers, J. M., Moniruzzaman, A., & Palepu, A. (2015). Changes in Daily Substance Use Among People Experiencing Homelessness and Mental Illness: 24-month Outcomes Following Randomization to Housing First or Usual Care. Addiction. doi: 10.1111/add.13011

