Should we Combine Smoking Cessation & Substance Use Disorder Treatments?
Despite commonly held beliefs in the substance use disorder (SUD) treatment community, studies have shown substance use disorder treatment-seeking cigarette smokers have similar outcomes regardless of whether or not they choose to engage in smoking cessation interventions during substance use disorder (SUD) treatment.
Smoking cessation treatments have had limited impact on long-term smoking outcomes in this vulnerable population.
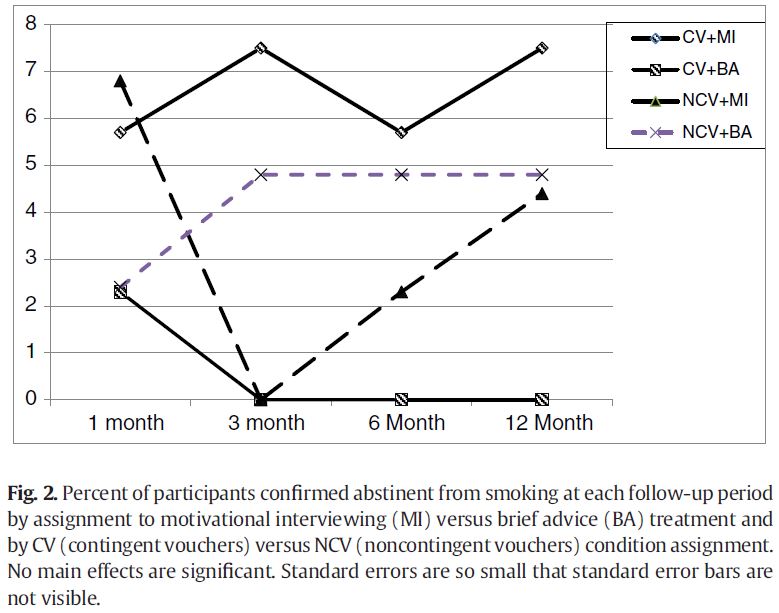
Rohsenow and colleagues tested whether adding motivational interviewing to contingency management improved smoking outcomes among individuals attending residential substance use disorder (SUD) treatment, and whether treatments had differential impact on SUD outcomes. Participants received one of four treatment combinations: Contingent Vouchers + Motivational Interviewing; (n = 53); Contingent Vouchers + Brief Advice (n = 44); Non-contingent vouchers + Motivational Interviewing (n = 45); or Non-contingent vouchers + Brief Advice (n = 42).
Motivational interviewing (MI) and brief advice (BA) were both 4-session interventions conducted over 3 weeks. MI offers personalized feedback, pros/cons of smoking, relationships of smoking to alcohol use and sobriety, discussion around barriers to change, and individualized goal setting. BA, in contrast, is a more directive approach asking patients to set a quit date within 2 weeks of the initial session. The contingent voucher (CV) intervention also occurred during these 3 weeks. Patients could earn vouchers toward store gift cards initially for reduced carbon monoxide levels and then for abstinence. Including various bonuses, they could earn a maximum of $433. Non-contingent voucher (NCV) participants earned prizes on the same schedule irrespective of whether or not they were abstinent from smoking.
In addition to the 3 week treatment, participants were measured at 1-month, 3-month-, 6-month, and 12-month follow-ups on 7-day cigarette abstinence (confirmed by carbon monoxide and/or urine cotinine levels; cotinine is the predominant metabolite of nicotine) and cigarettes per day. Primary substance use disorder (SUD) outcome was self-reported abstinence from alcohol and other drugs (confirmed by urine toxicology screen).
On average, participants were 35 years old, had 12 years of education, and earned $9,500 during the year before treatment entry. Approximately 85% were White, 9.2% were African American, and 6.6% were Latino; 55% were female and 11% were married. They smoked 22 cigarettes per day and had been smoking daily for 18 years. Regarding SUDs, 71% met criteria for alcohol use disorder, 74% for cocaine use disorder, 53% for opioid use disorder, and 37% for marijuana use disorder. None of these demographic or clinical characteristics differed by condition.
Source: (Rohsenow et al., 2015)
Thus although neither contingent vouchers (CV) nor motivational interviewing (MI) had better outcomes than non-contingent vouchers or brief advice, respectively, there was an interaction effect such that participants receiving both CV and MI had the best outcomes.
Although cigarettes per day did not differ by condition, there was an overall significant decrease in number of cigarettes per day from baseline to 12-months (23 to 14). These smoking cessation outcomes were similar across levels of motivation to quit, minutes until first cigarette of the day, and drug use days (during the prior 6 months) upon study entry. Importantly, regarding substance use disorder (SUD) outcomes, groups were not found to differ on relapse rates (and drug/heavy drinking days) across follow-ups for all four conditions. Specifically, 90% remained abstinent at 1 month, 66% at 3 months, 56% at 6 months, and 36% at 12 months.
IN CONTEXT
Up to 75% of patients receiving treatment for alcohol use disorder are also nicotine dependent, placing them at risk for a host of negative cigarette-related health outcomes, compounding overall health risk.
This study showed that although cigarette smoking is likely to decrease over time, a state-of-the-art psychosocial intervention is unlikely to result in substantially greater likelihood of quitting cigarettes during the year following treatment.
substance use disorder (SUD) treatment patients who smoke cigarettes remain a medically vulnerable group – more research is needed to understand motivation and the timing of quitting efforts and optimal intervention time points among these patients.
BOTTOM LINE
- For individuals & families seeking recovery: Attempting to quit cigarettes may not affect recovery from other substances if you choose to tackle both at the same time.
- For scientists: More research is needed to better understand patterns of cigarette smoking in substance use disorder (SUD)-treatment seeking individuals. The current study used a 1 year window. This is far longer than many other similar studies but still may be insufficient to understand what is likely a multi-year trajectory.
- For policy makers: Support the inclusion of smoking cessation treatments as an option in substance use disorder (SUD) programs to give those interested the option of quitting smoking in addition to alcohol and other drugs.
- For treatment professionals and treatment systems: Offering smoking cessation services in addiction treatment is unlikely to increase your patients’ risk of relapse.
CITATIONS
Rohsenow, D. J., Tidey, J. W., Martin, R. A., Colby, S. M., Sirota, A. D., Swift, R. M., & Monti, P. M. (2015). Contingent Vouchers and Motivational Interviewing for Cigarette Smokers in Residential Substance Abuse Treatment. Journal of substance abuse treatment.

