Better Down the Road? The Long-term Outcomes of Opioid Use Disorder Patients Treated with Medication
Research has shown that medications such as methadone and buprenorphine/naloxone (“Suboxone”) are effective at reducing opioid use. But how do patients treated with these medications do over the long-term?
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Of the 20.5 million Americans 12 or older that had a substance use disorder in 2015, 2 million had a substance use disorder involving prescription pain relievers and 591,000 had a substance use disorder involving heroin, referred to in combination as opioid use disorders. Opioid use disorder can be medically treated with pharmacotherapies (i.e., medicines).
The FDA has approved pharmacotherapies for the treatment of opioid use disorder including methadone (opioid agonist) and buprenorphine/naloxone (“Suboxone”; a partial opioid agonist). These medicines have been shown to reduce cravings, mitigate withdrawal symptoms, block the effects of other opioid drugs, prevent lethal overdose, and increase remission rates. These medicines have been shown to reduce cravings, mitigate withdrawal symptoms, block the effects of other opioid drugs, prevent lethal overdose, and increase remission rates.
Despite these beneficial treatment effects the use of non-prescribed opioids or heroin can continue after treatment is initiated (although often at a greatly reduced rate compared to no treatment). Long-term observation of opioid use among individuals receiving medication for opioid use disorder can increase our understanding of disease progression and treatment response to improve care. The present study aimed to identify and describe distinct opioid use patterns and factors associated with these patterns among participants who received medications for opioid use disorder.
HOW WAS THIS STUDY CONDUCTED?
This is a secondary data analysis of a study called Starting Treatment with Agonist Replacement Therapy, or START. START randomly assigned participants with opioid use disorder to receive methadone or Suboxone. The primary outcomes of this study tended to favor the use of either of these medicines for opioid use disorder compared to no medicine, and methadone was slightly better than Suboxone. These results are described in more detail in a previous RRI Bulletin summary.
In this analysis, 795 of the original 1,269 participants enrolled in this multisite trial reported on their continued opioid use. There were a number of reasons why some participants were not included in the study such as logistical problems with study sites. Treatment with medication lasted about 8 months over the follow-up period, on average, with a mean of 20 months for the methadone group and 7 months for the Suboxone group. Enrollment occurred from 2006 to 2009 and follow-up interviews were conducted from 2011-2014 which was an average 4.5 years at follow-up.
Self-report of any opioid use was confirmed with urine toxicology screens (“drug tests”). The researchers used sophisticated statistical modeling (i.e., growth curve trajectories) to identify and group patients’ responses to the medication in terms of days of opioid use and then examined what factors were associated with being in these outcome groups.
WHAT DID THIS STUDY FIND?
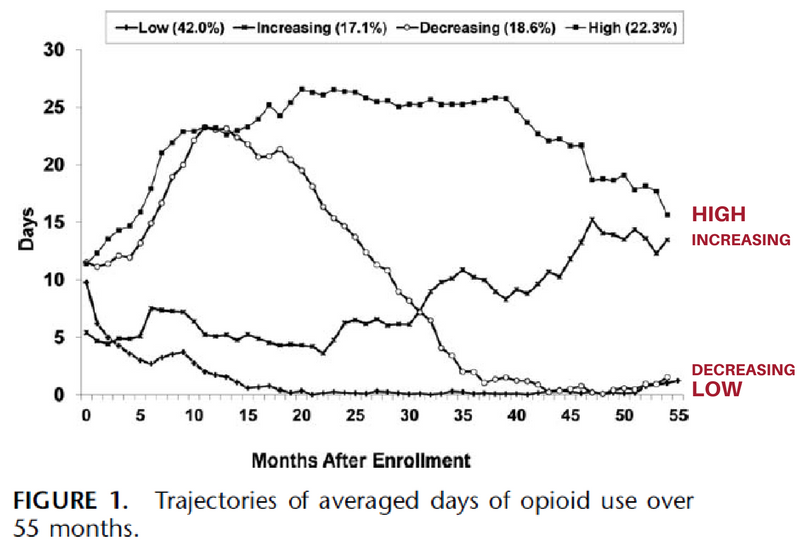
Four distinct trajectory groups were identified based on opioid use over the follow-up period:
- low use (42.0%)
- high use (22.3%)
- increasing use (17.1%)
- decreasing use (18.6%).
The low use group reported a low level of opioid use throughout the whole observation period. Individuals in the high use group remained at a high level of opioid use (more than 15 days per month on average) throughout the 55-month period. Individuals in the increasing use group had a low level of opioid use in the first 6 months, but then reported a consistent increase in opioid use from months 7 to 55. Individuals in the decreasing group reported a decrease in opioid use after an initial increase during the first year (from 13 days to 23 days per month on average during month 1-12), followed by a consistent decrease to almost no use from months 42-55.
Factors associated with being in the high use group were identifying as Hispanic, history of injection drug use, higher mental health functioning at baseline (which decreased by follow-up), location on the West Coast, and randomization to Suboxone (versus methadone). The decreasing drug use group, was associated with being randomized to Suboxone and having a history of injecting drugs.
There were no factors significantly associated with the likelihood of being in the increasing drug use group relative to the low use group. The low use group had the highest number of months in treatment with either type of pharmacotherapy (36.6 months), the high use group had the least amount of time in treatment (16.2 months), and the decreasing and increasing use groups were in between (26.7 and 26.0, respectively). Treatment participation seems to be an important factor in explaining variations in opioid use over time.
WHY IS THIS STUDY IMPORTANT?
This study provided a rare insight into the long-term trajectories of participants randomized to using either methadone or Suboxone. Long-term outcome data is valuable for clinicians, policy makers, and families to make evidence-based decisions and raise critical questions.
There was considerable heterogeneity (i.e., variability) in opioid use trajectories, but a promising finding was that the largest group which consisted of more than 40% of the sample had a consistently low level of opioid use after initiating medication, and another 18.6% eventually decreased to almost no use after the first year. These results are similar to another long-term study that found about two-thirds of patients with a pharmaceutical opioid use disorder (i.e., “painkillers”) were in remission 3.5 years after initially receiving Suboxone as part of a randomized controlled trial. History of injection drug use and randomization to Suboxone were the two most consistent factors associated with worse opioid use. Injection drug use is a marker of a more severe drug use disorder.
A previous study on this sample showed opioid use was higher among participants randomized to Suboxone (42.8% positive opioid urine test at follow-up) versus methadone (32%). More specifically, the Suboxone group had used heroin an average of 5.8 days of the past 30 days at follow-up compared to 4.4 days, on average, in the methadone group. Pharmacological treatment participation was higher in the methadone group for the first 10 months and opioid use was consistently lower compared to Suboxone.
- LIMITATIONS
-
- Many participants dropped out of the study over the course of 4.5 years which can create biases in the estimates of these outcomes for different patient groups. This is because patients who dropout or are unable to be contacted may be doing worse (or possibly better) and consequently, results obtained from those patients who are successfully followed can skew results.
NEXT STEPS
The stable high use group (22% of the sample) not only increased opioid use from the initial level, but continued at a high level over a long period of time. Future research should determine how to identify the people most susceptible to this trajectory and what may be needed to reduce their opioid use and support long-term remission.
BOTTOM LINE
- For individuals & families seeking recovery: After the participants used medication to treat opioid use disorder, the researchers statistically grouped study participants based on their opioid use and found that the largest group (over 40% of the sample) showed consistent low levels of opioid use after treatment and an additional 18.6% also had almost no opioid use after one year. The minority of participants (22%) showed elevated levels of opioid use after receiving treatment. Medicine for opioid use disorder has been shown to reduce cravings, mitigate withdrawal symptoms, block the effects of other opioid drugs, prevent lethal overdose, and increase remission rates . If you or a friend have an opioid use disorder, medication can increase your chances of remission.
- For scientists: Several baseline factors (West coast location, identifying as Hispanic, history of drug use by injection, and higher mental health status) were associated with the high use group suggesting risk factors needing attention for future targeted interventions. Scientists may wish to test what other services should be delivered to a high use group to help reduce opioid use, such as higher medication doses, continuing monitoring, more intensive psychotherapy, or involvement in recovery support services.
- For policy makers: Consider appropriating funding and other resources to create avenues for persons with opioid use disorder to access life-saving medicines, such as Suboxone and methadone. Compared to Suboxone, methadone has more restrictions around treatment access even though it was associated with consistently less opioid use and increased treatment retention for the first 10 months. You may consider promoting policies that are consistent with evidenced-based treatment protocols.
- For treatment professionals and treatment systems: In this analysis, when the participants were grouped based on their opioid use after initiating treatment, the largest of four identified groups (over 40% of the sample) had a low level of use, which diminished to almost no use at all after 4.5 years. An additional 18.6% also had almost no opioid use after the first year. The two most consistent factors associated with worse opioid use trajectories were a history of injection drug use and randomization to Suboxone (versus Methadone); however, both medicines reduced opioid use. Encouraging patients to use some form of medication for opioid use disorder is likely to result in improved outcomes over the long-term with perhaps a slight advantage for methadone (an initial response of 4.4 days of heroin use in the past 30 days at follow-up) compared to Suboxone (5.8 days). That said, Suboxone is empirically supported compared to no treatment and may be a more feasible option in many communities given the restrictions on access to methadone.
CITATIONS
Hser, Y., Huang, D., Saxon, A.J., Woody, G., Moskowitz, A.L., Matthews, A.G. (2017). Distinctive trajectories of opioid use over an extended follow-up of patients in a multisite trial on Buprenorphine + Naloxone and Methadone. Journal Addiction Medicine, January/February 11(1), 63-69. doi: 10.1097/ADM.0000000000000274

