Newly discovered patterns of prescription drug misuse among adolescents and young adults: Who is at greatest risk for substance use disorder in adulthood?
Taking medications like opioids, stimulants, and sedatives without a prescription or not as prescribed (“misuse”) is a significant public health concern worldwide. In this study, authors take a critical look at how prescription drug misuse during teenage and young adult years might lead to substance use disorder in adulthood, and what factors are indicative of these riskier patterns of prescription drug use misuse to identify targets for prevention.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
The high prevalence and rising incidence of prescription drug misuse, particularly among young adults between 18 and 25 in the United States, is a significant public health concern, and opioid, stimulant, and sedative/tranquilizer medications are the mostly frequently misused. While the majority of adolescents and young adults who misuse prescription drugs will subsequently discontinue their use, approximately one out of three will continue misusing them. Unfortunately, very little is known about the characteristics of these individuals or patterns of misuse that predispose them to substance use disorder later in adulthood. In the first known large-scale, population-based longitudinal study of its kind, authors evaluated patterns of prescription drug misuse over time, and predisposing characteristics, during this important developmental period.
HOW WAS THIS STUDY CONDUCTED?
The authors of this study used a naturalistic longitudinal cohort design where groups of people were followed over time and assessed/reassessed prescription drug use as part of the national multicohort and longitudinal Monitoring the Future study. The overarching aim of this study is to monitor and study adolescent behavior. This was accomplished by conducting biennial follow up surveys among a randomly selected sample of 2,450 students from among cohorts of approximately 17,000 18-year-old students recruited annually, beginning in 1975. Each participant was followed until the age of 35. For the current study and analysis, authors analyzed data from 51,223 18-year-old high school students who were also surveyed at ages 19-20, 21-22, 23-24, 25-26, 27-28, 29-30, and a final time at age 35. Prescription drug misuse questions were identical at each assessment period and asked participants to report non-prescribed use of medications in the past year on an interval scale ranging from 1 = “no occasions” up to 7 = “40 or more occasions” scale.
Figure 1.
Follow up substance use disorder questions administered at age 35 included 15 items about substance use and used those responses to map onto eight of the 11 DSM-5 criteria reflecting established alcohol, cannabis, and opioid or other drug use disorder criteria, and in reference to the past five years (i.e., since the age of 30). These criteria included “substance use resulting in failure to fulfill major role obligations”; continued substance use despite physical hazards; continued use despite “persistent and recurrent interpersonal or social problems”; “tolerance”; “withdrawal”; “persistent desire or unsuccessful efforts to cut down”; “health-related issues related due to substance use”; and subjective “craving.” The authors then created a binary score based on whether participants met two or more of these criteria between ages 30 and 35 (no = 0, yes = 1).
The authors also gathered and analyzed sociodemographic characteristics including sex (i.e., male or female), race and ethnicity, geographic region of residence, parent’s educational level, students’ personal educational goals (at age 18), average grade point average while in school, and cohort year they entered the study (between 1976 and 1982, 1983 and 1989, or 1990 and 1996). Behavioral characteristics were assessed at age 18 and included use of cigarettes and marijuana in the last 30 days, binge drinking in the past two weeks, as well as whether participants graduated from a four-year university by the time they reached age 35.
The authors then analyzed the data to create groupings of individuals who were distinguishable on the basis of their combined prescription drug misuse patterns over time (i.e., combined stimulant, opioid, and sedative or tranquilizer medications). The authors also examined separately participants’ specific patterns of use across stimulant, opioid, and sedative or tranquilizer medication classes. The authors then examined the sociodemographic variables and behavioral characteristics to see whether certain characteristics were associated with distinct prescription drug use patterns over time.
Among the 51,223 participants included in the study, 51.7% were women, 48.3% were men. In terms of race/ethnicity, the majority were White (75.6%), followed by African American (12.1%), Hispanic (6.2%), then “other” race/ethnicity (6.1%). Forty-five percent lived in suburban neighborhoods, 25.8% in large urban areas, and 28.9% lived in rural communities. At baseline (age 18), the majority of participants did not have goals to attend college (56.9%) and had parents who earned less than a four-year degree (59.8%). Most performed well in high school, earning a B- or higher on average (74%). At age 35, the majority had less than a four-year degree (59.8%), and 40.2% had a bachelor’s degree or higher. At baseline, 69.5% had not smoked cigarettes, 77% had not smoked marijuana, and 65.5% had not engaged in binge drinking in the last 30 days. Participants came from all areas of the country, with the Southern states being represented at 33.1%, the Western states at 17.5%, Midwest at 28%, and the Northeast at 21.4% of the total sample.
The sample in this study was 18 and older, predominantly male (65%), White/Caucasian (80%), single (unmarried; 66%), and homeless (56%) or “precariously housed” (44%). Educational status was variable, with the average having completed some high school or completing high school. Further, 71% screened positive for major depressive disorder, 17% with a manic or hypomanic episode, 45% with PTSD, 28% with panic disorder, 13% with a mood disorder (with psychotic features), 23% with a psychotic disorder (e.g., schizophrenia), 16% with an alcohol use disorder, and 53% with some other substance use disorder. The vast majority also had one or more co-occurring health condition(s).
WHAT DID THIS STUDY FIND?
The aim of this research was to identify distinct patterns of prescription drug misuse, risk for substance use disorder, and characteristics of individuals associated with distinct prescription drug use patterns over time. Analyzing data from 51,223 participants recruited at age 18 and followed until the age of 35, the authors identified five distinct patterns of combined prescription drug misuse, marked by peak use at different ages, that were associated with different levels of risk for substance use disorder by at 35. The first and most common pattern, which included 90.4% of the sample, was characterized by rare to no prescription drug misuse periods over the 17-year span. Individuals classified into the remaining four combined drug groups evidenced periods of “high frequency” prescription drug misuse, with peak prescription drug misuse at ages 1) 18, 2) 19-20, 3) 23-24, and 4) 27-28.
When each prescription drug class was analyzed separately, distinct patterns of misuse emerged for individuals who reported misuse of opioids and sedatives or tranquilizer medications. Aside from individuals classified as having no prescription drug misuse, the four remaining “high frequency” opioid misuse groups reported peak use at ages 18, 19-20, 21-22, and 29-30. The four groups with reported histories of “high frequency” sedative or tranquilizer medication misuse also evidenced peak misuse at ages 18, 19-20, and 21-22; however, the late onset group did not engage in peak misuse until age 35.
Compared to individuals with rare or no prescription drug misuse, individuals classified as having peak misuse at 18, 19-20, 23-24, and 27-28 evidenced a 28%, 74%, 189%, or 408% increased risk of experiencing two or more substance use disorder symptoms by age 35, respectively. Risk factors for belonging in the latest peak prescription misuse group included White race, having less than a four-year college degree, heavy drinking and use of cigarettes and marijuana in high school, and a history of poly-prescription drug misuse. (i.e., misuse of multiple medications at once).
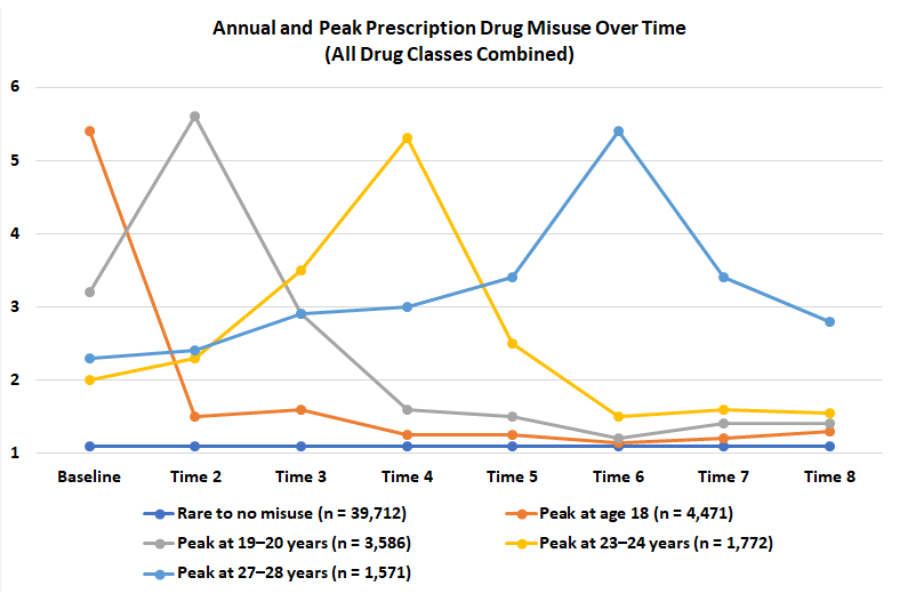
Figure 2. Plot of annual and peak prescription drug misuse for each identified grouping. Self-reported non-prescribed use of prescription medication was measured on a 1 = “no occasions” to 7 = “40 or more occasions” scale.
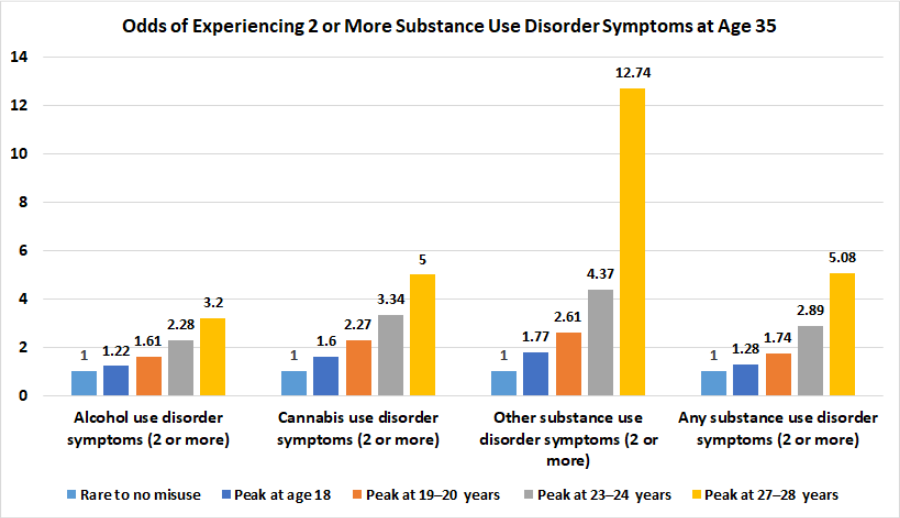
Figure 3. Bar chart displaying the odds of having two or more alcohol, cannabis, other drug (including prescription drugs), or any substance use disorder symptoms at age 35. All odds displayed are relative to 1.0 for individuals in the “rare or no prescription drug misuse” group.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study is the first to document the existence of distinct patterns of prescription drug misuse, which is associated with increased risk for substance use disorder by age 35.
Compared to the majority of individuals with little to no prescription drug misuse history, the remaining 4 groups were all at increased risk for substance use disorder, and individuals with peak prescription misuse after age 27 were at greatest risk.
Implications for prevention and intervention include targeting individuals at risk for “high frequency” prescription drug misuse, particularly individuals at risk for manifesting late peak onset. These individuals include White adolescents and young adults without a college education (or without plans for pursuing college education), and who report heavy drinking and use of cigarettes and marijuana in high school or have a history of poly-prescription drug misuse. This suggests that more assertive interventions might be indicated for youth exhibiting any heavy alcohol or other drug use during high school years to potentially offset increased risk of later SUD in adulthood.
Lower risk among other groups, like African Americans, might reflect lower SES, less access to health care, and, therefore, less access to prescription drugs.
Policies and strategies aimed at preventing prescription drug misuse are critical. The results of this study provide implications for the timing of targeted intervention strategies, as well as insight into the types of individuals who may benefit the most.
- LIMITATIONS
-
- The authors do not include information about treatment receipt or other protective factors that might delay onset of peak misuse or lead to a reduction in misuse following individuals’ period peak misuse.
- The exclusive reliance on self-report measures of past year prescription drug misuse, and a limited scale of 1 = “no occasions” to 7 = “40 or more occasions” offers less sensitivity to the detection of more severe cases of prescription drug misuse.
- The use of self-report measures of substance use and disorder symptoms (collected at age 35) in the last five years is inconsistent with clinical practice of diagnosing substance use disorders based on co-occurrence of symptoms within the past year.
- Relatedly, the authors did not assess substance use disorder domains prior to 35 and only asked participants to recall ages 30-35. This limitation makes it impossible to know to what extent substance use disorder criteria may have been met prior to age 30, or the possibility that participants sought treatment and/or entered early or sustained remission by age 30.
- By limiting measurement of substance use disorder risk between ages 30 and 35, the authors are unable to highlight disorder risk prior to age 30. The lack of recovery time between late peak misuse and substance use disorder risk, assessed at age 35, might account for the association between late peak onset substance use disorder risk at 35.
- The authors do not assess or model other substances of use, including alcohol, cannabis, or other illicit substances that might precede, follow, or coincide with periods of peak prescription drug misuse.
- Limited measurement of demographic characteristics, including such things as income, which the authors indicate is a significant risk factor for having access to prescription medications, as well as using them in a non-prescribed fashion.
BOTTOM LINE
- For individuals and families seeking recovery: This study identified groups of individuals who are distinct in their patterns of prescription drug misuse, with peak levels of misuse in the latter part of their 20s predicting the greatest risk for substance use disorder by age 35. Importantly, heavy alcohol/drug involvement during high school years predicted prescription misuse and SUD problems in adulthood. This underscores opportunities for more screening and assertive intervention for this high-risk group during this critical period of development. While risk for substance use disorder was significantly greater among all groups with a history of prescription drug misuse, the significant decline in prescription drug misuse over time among all groups may be an indication of recovery. Thus, screening, early detection, and intervention are highly recommended to prevent further misuse and/or use of other addictive substances.
- For treatment professionals and treatment systems: The vast majority of individuals (over 90%) did not misuse prescription medications. The prescription drug misuse patterns among those that did were characterized by peak levels of misuse ages 18, 19-20, 23-24, and 27-28, with later ages of peak onset predicting a greater likelihood of exhibiting substance use disorder symptoms by age 35. Clinicians are encouraged to carefully assess prescription drug use patterns of clients/patients to detect changes in use over time and provide psychoeducation to young adults about the potential for addiction by age 35 for individuals who engage in “high frequency” prescription drug misuse. This will be especially important for clients/patients with high frequency misuse after the age of 27. Clinicians should also be mindful of the findings that individuals most at risk for exhibiting substance use disorder symptoms by age 35 in this study were White, did not hold a college degree, and reported binge drinking and use of cigarettes and marijuana in high school. These findings suggest ongoing need for assertive intervention during these critical developmental periods. Finally, the observation that peak prescription drug misuse occurred after a period of gradual increase over time, followed by a precipitous drop in the frequency of misuse, is encouraging. These patterns have implications for early detection and prevention and represent positive prognostic indicators for individuals following periods of peak prescription drug misuse. However, clinicians working with individuals during and/or following peak periods of prescription drug misuse should be mindful of patients’/clients’ use of other substances (unmeasured in the current study), which might explain the drop in prescription drug misuse here and might undermine long-term recovery. Clinicians and treatment systems need to collaborate with educational systems to best meet the health care needs of students, some of whom are going on to engage in prescription drug misuse and encounter additional substance use disorder risks later in life.
- For scientists: Authors in this study discovered latent classes of individuals distinguishable by their prescription drug use patterns between ages 18 and 35, with peak misuse between ages 27-28 predicting elevated substance use disorder risk by age 35. The most typical pattern, characteristic of over 90% of participants, was rare to no prescription drug misuse. The remaining four groups where characterized by onset of peak prescription drug misuse at age 18, 19-20, 23-24, and 27-28 (highest risk for substance use disorder by age 35). It is possible that there is something especially disruptive about peak prescription drug misuse in mid to late 20s (e.g., greater disruption to social or occupational functioning), or that the gradual and more chronic ascent to peak use later on explains the added risk. It is also possible that later peak onset is most associated with substance use disorder symptoms because it is most closely linked in time with age 35, providing less recovery time relative to other groups with younger ages of peak prescription drug misuse. Future research is needed to extend the observation period (e.g., to age 40, 50, 60, etc.) and to determine the causes of elevated risk for individuals in the later age of onset groups. Researchers are encouraged to consider alternative means of assessment of prescription drug use, and other substances, in future research. This could include more sensitive self-report measures (e.g., higher ceiling than 7 = “40 or more occasions”) and more comprehensive assessment of sociodemographic characteristics unmeasured in the current study.
- For policy makers: The identification of different groups of adolescents and young adults with different ages of peak prescription drug misuse onset, with greatest risk for substance use disorder by 35 evidenced by those with peak prescription misuse between ages 27 and 28, has significant implications for healthcare policy and prevention. Prescription practices regarding stimulant, opioid, and sedative or tranquilizer medications could be informed by these findings and adjusted to offset risk for individuals prone to experiencing periods of peak prescription drug misuse. At the same time, it will be important to also implement integrated prescription medication diversion tracking programs to monitor prescription medication use and to prevent diversion. Implications also exist for addressing modifiable behavioral characteristics of individuals who engaged in prescription drug misuse. Strategies might include promoting and decreasing barriers to pursuing university education; and providing evidence-based cigarette, cannabis, and alcohol use prevention programs in high schools. This last point is important in light of the researchers’ finding that use of drugs and alcohol in high school was associated with subsequent prescription drug misuse and SUD risk in adulthood. Lastly, funding and facilitating bridges between treatment, health care, and educational systems could assist efforts at early detection and intervention, as education is not sufficiently resourced to be able identify, prevent, or reverse substance related risks.
CITATIONS
McCabe, S. E., Veliz, P. T., Dickinson, K., Schepis, T. S., & Schulenberg, J. E. (2019). Trajectories of prescription drug misuse during the transition from late adolescence into adulthood in the USA: a national longitudinal multicohort study. The Lancet Psychiatry, 6(10), 840-850. doi: 10.1016/S2215-0366(19)30299-8

