l
The drug overdose crisis in the US has been characterized by 3 waves, with different types of opioids driving mortality in each. The first was driven by prescription opioids from 1999-2017, followed by heroin from 2010-2017. The third and current wave started in 2014 and was driven by synthetic opioids, primarily fentanyl and its analogs. However, a fourth wave is emerging that is being characterized by use of opioids and stimulants at the same time, or co-use, which is typically methamphetamine and cocaine. Mortality in this wave is further increased by the addition of other toxic substances to the drug supply, such as xylazine (i.e., a veterinary drug often used for sedation and pain relief, also known by its street name, tranq).
Public health vending machines have been implemented to help address the overdose crisis. These machines offer supplies to reduce the harms associated with drug use (e.g., sterile syringes, naloxone, drug testing kits), as well as other items that can help decrease transmission of infectious disease, such as first aid supplies and reproductive health kits. In the US, the first public health vending machines were installed in Clark County, Nevada, in 2017 by Trac-B, the non-profit arm of the Harm Reduction Center-Las Vegas. Trac-B currently operates 6 vending machines in Las Vegas that are located near community organizations and clinics that serve people who use drugs.
More knowledge about who is using public health vending services can provide data on recent drug use trends and also inform prevention and intervention efforts. Researchers in this study used such data to examine the demographics and drug use behaviors of people who registered for these vending machine services, including co-use of opioids and stimulants.
The research team examined the demographics and drug use behaviors of people who have registered to use the public health vending machines in Nevada. This information was pulled from completed registration forms for vending machine services and a survey that was completed during registration.
To register to access the vending machine, individuals must be 18 years old or older. Anyone over this age can register, regardless of reported drug use. Individuals must register online or in-person at a vending machine site and complete a consent form, which indicates that their data may be used for research purposes. In addition to the registration form, registrants were asked to complete an optional survey starting in 2021.
The variables of interest included demographics, drug use behaviors, and interest in services to reduce the harms associated with drug use, and other substance use services. Demographic information was collected from registration forms that were completed between 1/1/2021 and 6/30/2023 and included date of birth, sex assigned at birth, gender identity, race, ethnicity, zip code, and homelessness. Drug use behaviors and interest in services to reduce the harms associated with drug use were assessed via the survey completed during registration and asked participants about the following behaviors during the last 3 months: frequency of drug injection; specific drugs or drug combinations injected; frequency of using sterile or re-used needles; needle sharing behaviors; other routes of drug use (e.g., snorting, smoking); interest in detox or treatment; overdose experiences and familiarity with Narcan; and interest in HIV or hepatitis C testing, including prior positive results or treatment.
For the statistical analyses, the research team tested for group differences between those with and without history of injection drug use. They also ran models to examine the association between types of injection drug use (e.g., using stimulants only vs. co-use of stimulants and opioids) with overdose and needle or supply re-use. These models were adjusted for sociodemographic factors and frequency of injection drug use. Such statistical adjustments help to isolate the effect of interest – i.e., whether type of injection drug use is independently related to overdoses and risky drug use behaviors.
Among 637 participants, just over half were men (56%), with an average age of 36 years old. Nearly two-thirds (63%) identified as non-Hispanic White and 32.5% reported that they were homeless. Most participants reported injection drug use (85%). The most reported non-injection route of drug use was smoking (74%).
Demographic and drug use behavior among people who inject drugs
Out of the 637 registrants, 550 reported injection drug use. When compared to the group of registrants without a history of injection drug use, the group of registrants who reported a history of injection drug use were, on average, 2 years older, had 2 times greater odds of being male, 4 times greater odds of being white vs. black, and 2 times greater odds of being white vs. Hispanic, and 7 times greater odds of being homeless. There were also differences in routes of drug use, with 2.5 greater odds of snorting and 8 times greater odds of smoking among those who reported a history of drug use than those without.
Also, among people who reported injection drug use in the last 3 months, 69% reported injecting daily and 64% reported injecting at a frequency of 2-4 times per day. Methamphetamine and heroin were the most commonly injected substances, with 74% and 56% of people reporting that they injected these substances. Other commonly reported injected substances included goofball (i.e., a combination of methamphetamine and heroin; 22%), fentanyl (14%), and speedball (i.e., a combination of heroin and cocaine; 11%). Opioids, cocaine, benzodiazepines, steroids, hormones, and other amphetamines were all reported to be injected by less than 10% of registrants. Injection of 2 drugs at the same time, or co-use, was also common among people who reported injection drug use in the last 3 months, with 41% reporting co-use of opioids and stimulants.
Needle/supply behavior and infections among people who inject drugs
The majority of people who reported injection drug use in the last 3 months reported that “always” or “most of the time” they discarded their used needles in a puncture-proof container (61%) and used a new, sterile needle (62%). Most also reported that they “rarely” or “never” used a needle that had been used but sterilized (77%).
However, 22% reported that they shared needles to divide drugs, 19% reported sharing needles in general, 30% reported sharing supplies, 78% reported reusing their own needles, and 66% reported reusing their own supplies. Of the 19% of people that shared needles, 64% reported that they shared needles received from others. Of the 30% of individuals that shared supplies, 49% shared the supplies of others. Approximately 10% of respondents reported that they had an overdose in the last 3 months, 15% reported hepatitis C infection, and 6% reported HIV infection.
Overdoses, needle/supply re-use, and co-use of drugs among people who inject drugs
Almost all of the overdoses experienced in the last 3 months were among people who inject drugs (98%). Of those reporting an overdose in the last 3 months, 52% identified as men with an average age of 36 years old. The majority identified as non-Hispanic White (74%) and 38% reported homelessness. Fentanyl (62%) and heroin (59%) were the drugs that were most frequently used during an overdose. Co-use of opioid and stimulant injection was common, with 63% of people who experienced an overdose reporting this co-use of drugs. Most reported that they used naloxone during their overdose and 33% reported more than 1 overdose in the last 3 months.
Compared to people who inject drugs using stimulants only, people who inject drugs co-using opioids and stimulants had 4.5 times greater odds of overdose and those who used opioids only had 3 times greater odds. People who inject drugs co-using opioids and stimulants were also twice as likely to re-use injection supplies, compared to people who inject drugs using stimulants only. There were no differences between groups for the likelihood of re-using needles.
Interest in services to reduce the harms associated with drug use and treatment among people who inject drugs
Among people who inject drugs, 15% reported that they were interested in treatment/detox, 29% in naloxone education, 55% in obtaining naloxone, 14% in rapid hepatitis C testing, 4% in referral for hepatitis C medical treatment, 16% in rapid HIV testing, 1% in referral for HIV medical treatment, and 14% in referral for STD testing. A total of 40% of people who inject drugs reported ever using naloxone.
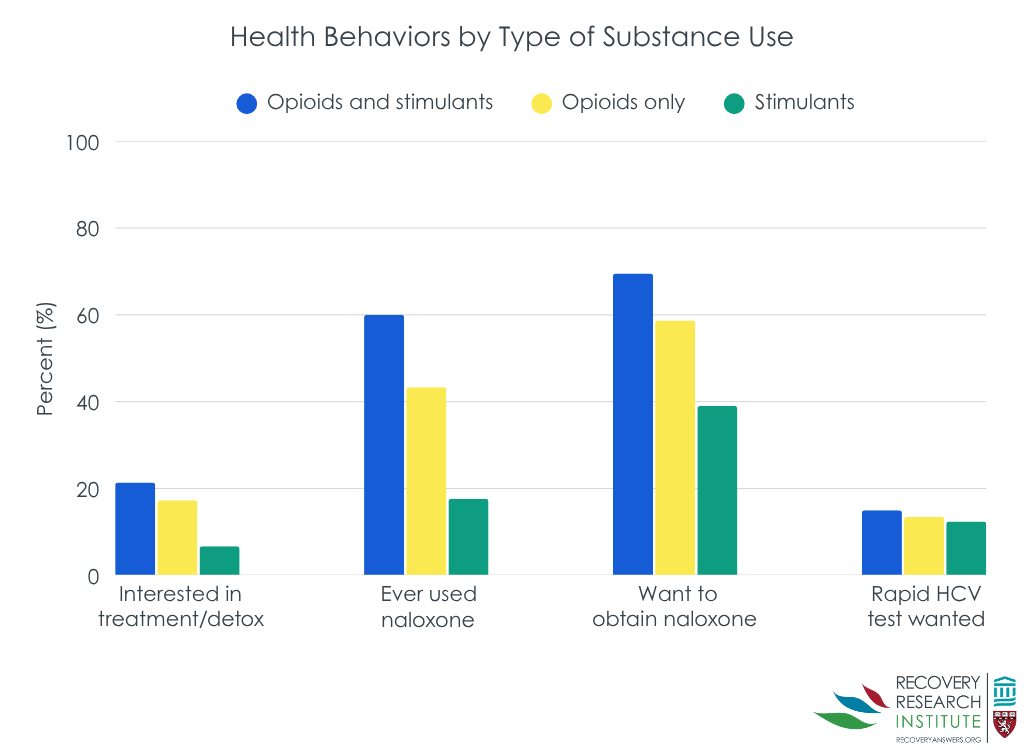
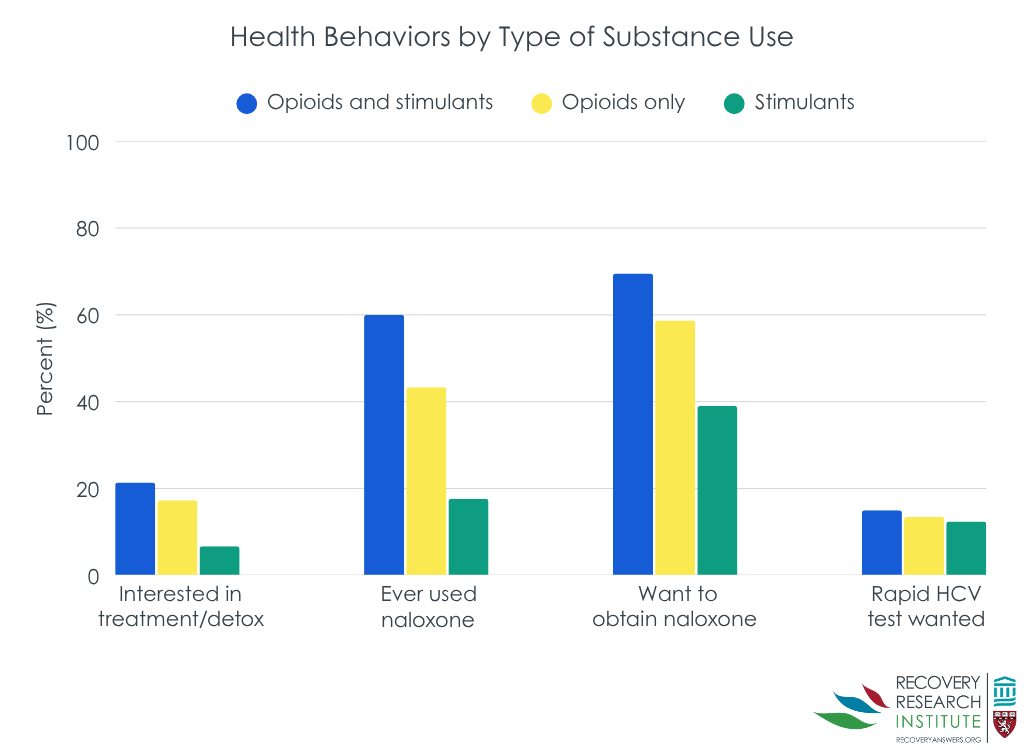
As shown in the graph below, compared to people who inject drugs using opioids only, people who inject drugs co-using opioids and stimulants had 2 times greater odds of using naloxone and 2.5 times greater odds of interest in a rapid HIV test. Compared to people who inject drugs using stimulants only, people who inject drugs co-using opioids and stimulants had 7 times greater odds of using naloxone and 4 times greater odds of interest in treatment/detox.
The research team examined the demographics and drug use behaviors of people who registered to use public health vending machines in Clark County, Nevada. Results showed that almost all people who registered reported injection use and that the majority of them were non-Hispanic White men in their 30s. Important drug use trends were also identified, with 41% of people who reported injection drug use and 63% of people who have experienced an overdose reporting that they have co-used opioids and stimulants. When compared with people who reported using only stimulants, co-use of opioids and stimulants were associated with a higher likelihood of overdoses and re-using supplies. However, people who inject drugs and reported co-use of opioids and stimulants also reported greater interest in services to reduce the harms associated with drug use and attending treatment.
The demographic profile of the vending machine registrants mirrors the profile of people who inject drugs nationwide in the US, with recent data showing that the estimated prevalence of injection drug use in the US is highest among non-Hispanic White men between the ages of 18 and 39. Further, the drug use patterns reported by the registrants is also consistent with those observed nationwide. Methamphetamine, heroin, goofball, and fentanyl were the most reported substances that were injected by the vending machine registrants, which is consistent with data from the Treatment Episode Data Set. These findings suggest that the demographic composition and drug use behaviors of public health vending machine clients are representative of the broader population of people who use drugs. Additionally, these results highlight the utility of using registration data for surveillance of the population of people who use public health vending machine services, which can help ensure the program is meeting the needs of their clients and inform prevention, intervention, and services to reduce the harms associated with drug use more broadly.
The high frequency of reported co-use of opioids and stimulants, and its association with overdoses, is consistent with a recent report showing that there was a 97% increase in overdose deaths involving fentanyl and stimulant co-use from 2020 to 2023 in Nevada. Together, these trends contribute additional evidence to the emergence of a fourth overdose wave that is characterized by drug co-use and further underscore the utility of using vending machine registration data for surveillance of drug use trends. Observing such trends can help alert county officials and treatment/services to reduce the harms associated with drug use organizations how efforts to serve people who inject drugs need to be tailored.
The demographic and drug use profiles of people who registered to use public health vending machines in Nevada mirrored that observed nation-wide, with almost all reporting injection use and the majority of them being non-Hispanic White men in their 30s. Important drug use trends were also identified, with a high prevalence of stimulant and opioid co-use being reported and its strong association with overdoses and re-use of injection supplies. At the same time, stimulant and opioid co-use was also associated with the greatest likelihood of services to reduce the harms associated with drug use practices and interest in treatment. These findings highlight the utility of public health vending machine registration data for surveillance of the population of people who inject drugs and emerging drug trends, which can inform prevention, intervention, and services to reduce the harms associated with drug use efforts.
Bryant, R. Q., Reich, K., Johnson, J. A., Delise, B., Zhang, Y., Lockett, C., & Allen, S. T. (2025). Drug use and harm reduction practices of applicants to a public health vending machine service in Clark County, NV, 2021–2023. Harm Reduction Journal, 22(52). doi: 10.1186/s12954-025-01207-x.
l
The drug overdose crisis in the US has been characterized by 3 waves, with different types of opioids driving mortality in each. The first was driven by prescription opioids from 1999-2017, followed by heroin from 2010-2017. The third and current wave started in 2014 and was driven by synthetic opioids, primarily fentanyl and its analogs. However, a fourth wave is emerging that is being characterized by use of opioids and stimulants at the same time, or co-use, which is typically methamphetamine and cocaine. Mortality in this wave is further increased by the addition of other toxic substances to the drug supply, such as xylazine (i.e., a veterinary drug often used for sedation and pain relief, also known by its street name, tranq).
Public health vending machines have been implemented to help address the overdose crisis. These machines offer supplies to reduce the harms associated with drug use (e.g., sterile syringes, naloxone, drug testing kits), as well as other items that can help decrease transmission of infectious disease, such as first aid supplies and reproductive health kits. In the US, the first public health vending machines were installed in Clark County, Nevada, in 2017 by Trac-B, the non-profit arm of the Harm Reduction Center-Las Vegas. Trac-B currently operates 6 vending machines in Las Vegas that are located near community organizations and clinics that serve people who use drugs.
More knowledge about who is using public health vending services can provide data on recent drug use trends and also inform prevention and intervention efforts. Researchers in this study used such data to examine the demographics and drug use behaviors of people who registered for these vending machine services, including co-use of opioids and stimulants.
The research team examined the demographics and drug use behaviors of people who have registered to use the public health vending machines in Nevada. This information was pulled from completed registration forms for vending machine services and a survey that was completed during registration.
To register to access the vending machine, individuals must be 18 years old or older. Anyone over this age can register, regardless of reported drug use. Individuals must register online or in-person at a vending machine site and complete a consent form, which indicates that their data may be used for research purposes. In addition to the registration form, registrants were asked to complete an optional survey starting in 2021.
The variables of interest included demographics, drug use behaviors, and interest in services to reduce the harms associated with drug use, and other substance use services. Demographic information was collected from registration forms that were completed between 1/1/2021 and 6/30/2023 and included date of birth, sex assigned at birth, gender identity, race, ethnicity, zip code, and homelessness. Drug use behaviors and interest in services to reduce the harms associated with drug use were assessed via the survey completed during registration and asked participants about the following behaviors during the last 3 months: frequency of drug injection; specific drugs or drug combinations injected; frequency of using sterile or re-used needles; needle sharing behaviors; other routes of drug use (e.g., snorting, smoking); interest in detox or treatment; overdose experiences and familiarity with Narcan; and interest in HIV or hepatitis C testing, including prior positive results or treatment.
For the statistical analyses, the research team tested for group differences between those with and without history of injection drug use. They also ran models to examine the association between types of injection drug use (e.g., using stimulants only vs. co-use of stimulants and opioids) with overdose and needle or supply re-use. These models were adjusted for sociodemographic factors and frequency of injection drug use. Such statistical adjustments help to isolate the effect of interest – i.e., whether type of injection drug use is independently related to overdoses and risky drug use behaviors.
Among 637 participants, just over half were men (56%), with an average age of 36 years old. Nearly two-thirds (63%) identified as non-Hispanic White and 32.5% reported that they were homeless. Most participants reported injection drug use (85%). The most reported non-injection route of drug use was smoking (74%).
Demographic and drug use behavior among people who inject drugs
Out of the 637 registrants, 550 reported injection drug use. When compared to the group of registrants without a history of injection drug use, the group of registrants who reported a history of injection drug use were, on average, 2 years older, had 2 times greater odds of being male, 4 times greater odds of being white vs. black, and 2 times greater odds of being white vs. Hispanic, and 7 times greater odds of being homeless. There were also differences in routes of drug use, with 2.5 greater odds of snorting and 8 times greater odds of smoking among those who reported a history of drug use than those without.
Also, among people who reported injection drug use in the last 3 months, 69% reported injecting daily and 64% reported injecting at a frequency of 2-4 times per day. Methamphetamine and heroin were the most commonly injected substances, with 74% and 56% of people reporting that they injected these substances. Other commonly reported injected substances included goofball (i.e., a combination of methamphetamine and heroin; 22%), fentanyl (14%), and speedball (i.e., a combination of heroin and cocaine; 11%). Opioids, cocaine, benzodiazepines, steroids, hormones, and other amphetamines were all reported to be injected by less than 10% of registrants. Injection of 2 drugs at the same time, or co-use, was also common among people who reported injection drug use in the last 3 months, with 41% reporting co-use of opioids and stimulants.
Needle/supply behavior and infections among people who inject drugs
The majority of people who reported injection drug use in the last 3 months reported that “always” or “most of the time” they discarded their used needles in a puncture-proof container (61%) and used a new, sterile needle (62%). Most also reported that they “rarely” or “never” used a needle that had been used but sterilized (77%).
However, 22% reported that they shared needles to divide drugs, 19% reported sharing needles in general, 30% reported sharing supplies, 78% reported reusing their own needles, and 66% reported reusing their own supplies. Of the 19% of people that shared needles, 64% reported that they shared needles received from others. Of the 30% of individuals that shared supplies, 49% shared the supplies of others. Approximately 10% of respondents reported that they had an overdose in the last 3 months, 15% reported hepatitis C infection, and 6% reported HIV infection.
Overdoses, needle/supply re-use, and co-use of drugs among people who inject drugs
Almost all of the overdoses experienced in the last 3 months were among people who inject drugs (98%). Of those reporting an overdose in the last 3 months, 52% identified as men with an average age of 36 years old. The majority identified as non-Hispanic White (74%) and 38% reported homelessness. Fentanyl (62%) and heroin (59%) were the drugs that were most frequently used during an overdose. Co-use of opioid and stimulant injection was common, with 63% of people who experienced an overdose reporting this co-use of drugs. Most reported that they used naloxone during their overdose and 33% reported more than 1 overdose in the last 3 months.
Compared to people who inject drugs using stimulants only, people who inject drugs co-using opioids and stimulants had 4.5 times greater odds of overdose and those who used opioids only had 3 times greater odds. People who inject drugs co-using opioids and stimulants were also twice as likely to re-use injection supplies, compared to people who inject drugs using stimulants only. There were no differences between groups for the likelihood of re-using needles.
Interest in services to reduce the harms associated with drug use and treatment among people who inject drugs
Among people who inject drugs, 15% reported that they were interested in treatment/detox, 29% in naloxone education, 55% in obtaining naloxone, 14% in rapid hepatitis C testing, 4% in referral for hepatitis C medical treatment, 16% in rapid HIV testing, 1% in referral for HIV medical treatment, and 14% in referral for STD testing. A total of 40% of people who inject drugs reported ever using naloxone.
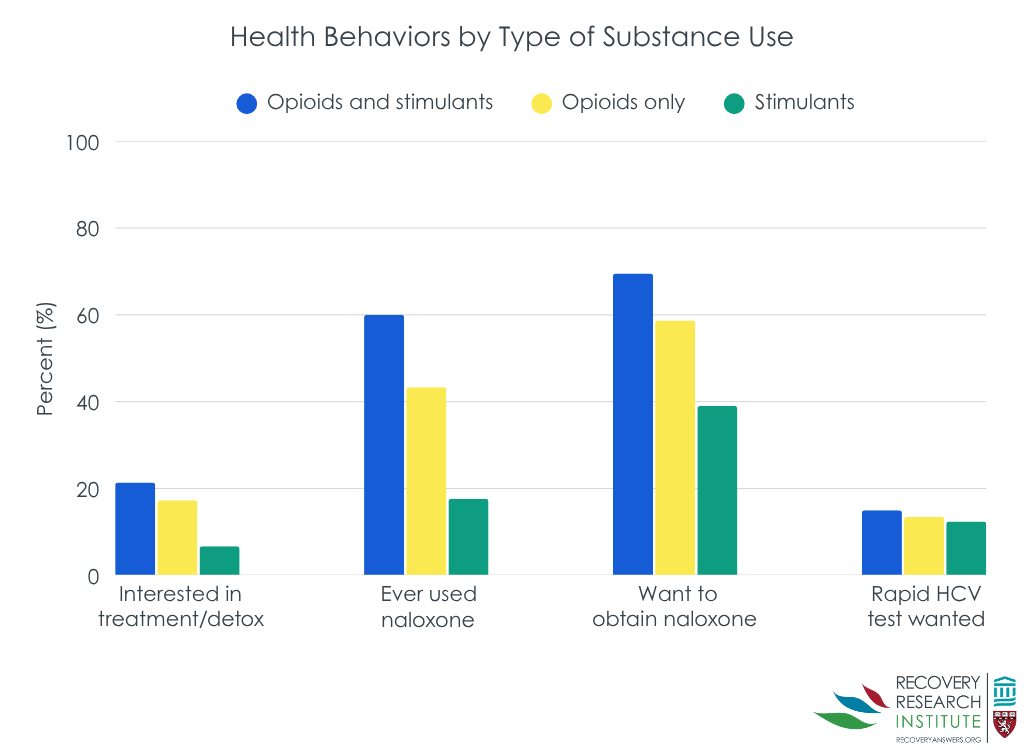
As shown in the graph below, compared to people who inject drugs using opioids only, people who inject drugs co-using opioids and stimulants had 2 times greater odds of using naloxone and 2.5 times greater odds of interest in a rapid HIV test. Compared to people who inject drugs using stimulants only, people who inject drugs co-using opioids and stimulants had 7 times greater odds of using naloxone and 4 times greater odds of interest in treatment/detox.
The research team examined the demographics and drug use behaviors of people who registered to use public health vending machines in Clark County, Nevada. Results showed that almost all people who registered reported injection use and that the majority of them were non-Hispanic White men in their 30s. Important drug use trends were also identified, with 41% of people who reported injection drug use and 63% of people who have experienced an overdose reporting that they have co-used opioids and stimulants. When compared with people who reported using only stimulants, co-use of opioids and stimulants were associated with a higher likelihood of overdoses and re-using supplies. However, people who inject drugs and reported co-use of opioids and stimulants also reported greater interest in services to reduce the harms associated with drug use and attending treatment.
The demographic profile of the vending machine registrants mirrors the profile of people who inject drugs nationwide in the US, with recent data showing that the estimated prevalence of injection drug use in the US is highest among non-Hispanic White men between the ages of 18 and 39. Further, the drug use patterns reported by the registrants is also consistent with those observed nationwide. Methamphetamine, heroin, goofball, and fentanyl were the most reported substances that were injected by the vending machine registrants, which is consistent with data from the Treatment Episode Data Set. These findings suggest that the demographic composition and drug use behaviors of public health vending machine clients are representative of the broader population of people who use drugs. Additionally, these results highlight the utility of using registration data for surveillance of the population of people who use public health vending machine services, which can help ensure the program is meeting the needs of their clients and inform prevention, intervention, and services to reduce the harms associated with drug use more broadly.
The high frequency of reported co-use of opioids and stimulants, and its association with overdoses, is consistent with a recent report showing that there was a 97% increase in overdose deaths involving fentanyl and stimulant co-use from 2020 to 2023 in Nevada. Together, these trends contribute additional evidence to the emergence of a fourth overdose wave that is characterized by drug co-use and further underscore the utility of using vending machine registration data for surveillance of drug use trends. Observing such trends can help alert county officials and treatment/services to reduce the harms associated with drug use organizations how efforts to serve people who inject drugs need to be tailored.
The demographic and drug use profiles of people who registered to use public health vending machines in Nevada mirrored that observed nation-wide, with almost all reporting injection use and the majority of them being non-Hispanic White men in their 30s. Important drug use trends were also identified, with a high prevalence of stimulant and opioid co-use being reported and its strong association with overdoses and re-use of injection supplies. At the same time, stimulant and opioid co-use was also associated with the greatest likelihood of services to reduce the harms associated with drug use practices and interest in treatment. These findings highlight the utility of public health vending machine registration data for surveillance of the population of people who inject drugs and emerging drug trends, which can inform prevention, intervention, and services to reduce the harms associated with drug use efforts.
Bryant, R. Q., Reich, K., Johnson, J. A., Delise, B., Zhang, Y., Lockett, C., & Allen, S. T. (2025). Drug use and harm reduction practices of applicants to a public health vending machine service in Clark County, NV, 2021–2023. Harm Reduction Journal, 22(52). doi: 10.1186/s12954-025-01207-x.
l
The drug overdose crisis in the US has been characterized by 3 waves, with different types of opioids driving mortality in each. The first was driven by prescription opioids from 1999-2017, followed by heroin from 2010-2017. The third and current wave started in 2014 and was driven by synthetic opioids, primarily fentanyl and its analogs. However, a fourth wave is emerging that is being characterized by use of opioids and stimulants at the same time, or co-use, which is typically methamphetamine and cocaine. Mortality in this wave is further increased by the addition of other toxic substances to the drug supply, such as xylazine (i.e., a veterinary drug often used for sedation and pain relief, also known by its street name, tranq).
Public health vending machines have been implemented to help address the overdose crisis. These machines offer supplies to reduce the harms associated with drug use (e.g., sterile syringes, naloxone, drug testing kits), as well as other items that can help decrease transmission of infectious disease, such as first aid supplies and reproductive health kits. In the US, the first public health vending machines were installed in Clark County, Nevada, in 2017 by Trac-B, the non-profit arm of the Harm Reduction Center-Las Vegas. Trac-B currently operates 6 vending machines in Las Vegas that are located near community organizations and clinics that serve people who use drugs.
More knowledge about who is using public health vending services can provide data on recent drug use trends and also inform prevention and intervention efforts. Researchers in this study used such data to examine the demographics and drug use behaviors of people who registered for these vending machine services, including co-use of opioids and stimulants.
The research team examined the demographics and drug use behaviors of people who have registered to use the public health vending machines in Nevada. This information was pulled from completed registration forms for vending machine services and a survey that was completed during registration.
To register to access the vending machine, individuals must be 18 years old or older. Anyone over this age can register, regardless of reported drug use. Individuals must register online or in-person at a vending machine site and complete a consent form, which indicates that their data may be used for research purposes. In addition to the registration form, registrants were asked to complete an optional survey starting in 2021.
The variables of interest included demographics, drug use behaviors, and interest in services to reduce the harms associated with drug use, and other substance use services. Demographic information was collected from registration forms that were completed between 1/1/2021 and 6/30/2023 and included date of birth, sex assigned at birth, gender identity, race, ethnicity, zip code, and homelessness. Drug use behaviors and interest in services to reduce the harms associated with drug use were assessed via the survey completed during registration and asked participants about the following behaviors during the last 3 months: frequency of drug injection; specific drugs or drug combinations injected; frequency of using sterile or re-used needles; needle sharing behaviors; other routes of drug use (e.g., snorting, smoking); interest in detox or treatment; overdose experiences and familiarity with Narcan; and interest in HIV or hepatitis C testing, including prior positive results or treatment.
For the statistical analyses, the research team tested for group differences between those with and without history of injection drug use. They also ran models to examine the association between types of injection drug use (e.g., using stimulants only vs. co-use of stimulants and opioids) with overdose and needle or supply re-use. These models were adjusted for sociodemographic factors and frequency of injection drug use. Such statistical adjustments help to isolate the effect of interest – i.e., whether type of injection drug use is independently related to overdoses and risky drug use behaviors.
Among 637 participants, just over half were men (56%), with an average age of 36 years old. Nearly two-thirds (63%) identified as non-Hispanic White and 32.5% reported that they were homeless. Most participants reported injection drug use (85%). The most reported non-injection route of drug use was smoking (74%).
Demographic and drug use behavior among people who inject drugs
Out of the 637 registrants, 550 reported injection drug use. When compared to the group of registrants without a history of injection drug use, the group of registrants who reported a history of injection drug use were, on average, 2 years older, had 2 times greater odds of being male, 4 times greater odds of being white vs. black, and 2 times greater odds of being white vs. Hispanic, and 7 times greater odds of being homeless. There were also differences in routes of drug use, with 2.5 greater odds of snorting and 8 times greater odds of smoking among those who reported a history of drug use than those without.
Also, among people who reported injection drug use in the last 3 months, 69% reported injecting daily and 64% reported injecting at a frequency of 2-4 times per day. Methamphetamine and heroin were the most commonly injected substances, with 74% and 56% of people reporting that they injected these substances. Other commonly reported injected substances included goofball (i.e., a combination of methamphetamine and heroin; 22%), fentanyl (14%), and speedball (i.e., a combination of heroin and cocaine; 11%). Opioids, cocaine, benzodiazepines, steroids, hormones, and other amphetamines were all reported to be injected by less than 10% of registrants. Injection of 2 drugs at the same time, or co-use, was also common among people who reported injection drug use in the last 3 months, with 41% reporting co-use of opioids and stimulants.
Needle/supply behavior and infections among people who inject drugs
The majority of people who reported injection drug use in the last 3 months reported that “always” or “most of the time” they discarded their used needles in a puncture-proof container (61%) and used a new, sterile needle (62%). Most also reported that they “rarely” or “never” used a needle that had been used but sterilized (77%).
However, 22% reported that they shared needles to divide drugs, 19% reported sharing needles in general, 30% reported sharing supplies, 78% reported reusing their own needles, and 66% reported reusing their own supplies. Of the 19% of people that shared needles, 64% reported that they shared needles received from others. Of the 30% of individuals that shared supplies, 49% shared the supplies of others. Approximately 10% of respondents reported that they had an overdose in the last 3 months, 15% reported hepatitis C infection, and 6% reported HIV infection.
Overdoses, needle/supply re-use, and co-use of drugs among people who inject drugs
Almost all of the overdoses experienced in the last 3 months were among people who inject drugs (98%). Of those reporting an overdose in the last 3 months, 52% identified as men with an average age of 36 years old. The majority identified as non-Hispanic White (74%) and 38% reported homelessness. Fentanyl (62%) and heroin (59%) were the drugs that were most frequently used during an overdose. Co-use of opioid and stimulant injection was common, with 63% of people who experienced an overdose reporting this co-use of drugs. Most reported that they used naloxone during their overdose and 33% reported more than 1 overdose in the last 3 months.
Compared to people who inject drugs using stimulants only, people who inject drugs co-using opioids and stimulants had 4.5 times greater odds of overdose and those who used opioids only had 3 times greater odds. People who inject drugs co-using opioids and stimulants were also twice as likely to re-use injection supplies, compared to people who inject drugs using stimulants only. There were no differences between groups for the likelihood of re-using needles.
Interest in services to reduce the harms associated with drug use and treatment among people who inject drugs
Among people who inject drugs, 15% reported that they were interested in treatment/detox, 29% in naloxone education, 55% in obtaining naloxone, 14% in rapid hepatitis C testing, 4% in referral for hepatitis C medical treatment, 16% in rapid HIV testing, 1% in referral for HIV medical treatment, and 14% in referral for STD testing. A total of 40% of people who inject drugs reported ever using naloxone.
As shown in the graph below, compared to people who inject drugs using opioids only, people who inject drugs co-using opioids and stimulants had 2 times greater odds of using naloxone and 2.5 times greater odds of interest in a rapid HIV test. Compared to people who inject drugs using stimulants only, people who inject drugs co-using opioids and stimulants had 7 times greater odds of using naloxone and 4 times greater odds of interest in treatment/detox.
The research team examined the demographics and drug use behaviors of people who registered to use public health vending machines in Clark County, Nevada. Results showed that almost all people who registered reported injection use and that the majority of them were non-Hispanic White men in their 30s. Important drug use trends were also identified, with 41% of people who reported injection drug use and 63% of people who have experienced an overdose reporting that they have co-used opioids and stimulants. When compared with people who reported using only stimulants, co-use of opioids and stimulants were associated with a higher likelihood of overdoses and re-using supplies. However, people who inject drugs and reported co-use of opioids and stimulants also reported greater interest in services to reduce the harms associated with drug use and attending treatment.
The demographic profile of the vending machine registrants mirrors the profile of people who inject drugs nationwide in the US, with recent data showing that the estimated prevalence of injection drug use in the US is highest among non-Hispanic White men between the ages of 18 and 39. Further, the drug use patterns reported by the registrants is also consistent with those observed nationwide. Methamphetamine, heroin, goofball, and fentanyl were the most reported substances that were injected by the vending machine registrants, which is consistent with data from the Treatment Episode Data Set. These findings suggest that the demographic composition and drug use behaviors of public health vending machine clients are representative of the broader population of people who use drugs. Additionally, these results highlight the utility of using registration data for surveillance of the population of people who use public health vending machine services, which can help ensure the program is meeting the needs of their clients and inform prevention, intervention, and services to reduce the harms associated with drug use more broadly.
The high frequency of reported co-use of opioids and stimulants, and its association with overdoses, is consistent with a recent report showing that there was a 97% increase in overdose deaths involving fentanyl and stimulant co-use from 2020 to 2023 in Nevada. Together, these trends contribute additional evidence to the emergence of a fourth overdose wave that is characterized by drug co-use and further underscore the utility of using vending machine registration data for surveillance of drug use trends. Observing such trends can help alert county officials and treatment/services to reduce the harms associated with drug use organizations how efforts to serve people who inject drugs need to be tailored.
The demographic and drug use profiles of people who registered to use public health vending machines in Nevada mirrored that observed nation-wide, with almost all reporting injection use and the majority of them being non-Hispanic White men in their 30s. Important drug use trends were also identified, with a high prevalence of stimulant and opioid co-use being reported and its strong association with overdoses and re-use of injection supplies. At the same time, stimulant and opioid co-use was also associated with the greatest likelihood of services to reduce the harms associated with drug use practices and interest in treatment. These findings highlight the utility of public health vending machine registration data for surveillance of the population of people who inject drugs and emerging drug trends, which can inform prevention, intervention, and services to reduce the harms associated with drug use efforts.
Bryant, R. Q., Reich, K., Johnson, J. A., Delise, B., Zhang, Y., Lockett, C., & Allen, S. T. (2025). Drug use and harm reduction practices of applicants to a public health vending machine service in Clark County, NV, 2021–2023. Harm Reduction Journal, 22(52). doi: 10.1186/s12954-025-01207-x.
151 Merrimac St., 4th Floor. Boston, MA 02114