l
Cannabis is one of the most commonly used psychoactive substances worldwide. With greater availability in retail locations and higher potency cannabis strains as a function of legalized recreational cannabis in many US states and Canada more broadly, more hazardous forms of cannabis use – such as daily use – are on the rise. While public perception of cannabis use is that it is relatively harmless and can even be beneficial, research shows that people who use cannabis are at a higher risk of fatal car accidents when driving under the influence and are at higher risks of self-harm and suicide. Cannabis use has also been linked to the development of mental health disorders, with the largest associations being shown with psychosis and schizophrenia.
Cannabis use may also increase the risk of early death. Indeed, research from Denmark, the UK, and Sweden have all found elevated mortality risks among people who use cannabis heavily or frequently, and who have cannabis use disorder. The current study examined whether people who received hospital-based care for a cannabis-related reason in Ontario, Canada had a higher risk of death over a 10-year period at the population-level. This research can help shed light on the potential association between cannabis use and mortality.
The research team examined whether receiving hospital-based care for a cannabis-related reason was associated with an increased risk of death. This was a retrospective, population-level study in which the general population in Ontario, Canada, was compared to those receiving hospital-based care for cannabis between 2006 and 2021.
The main predictor in the study was receiving hospital-based care for cannabis use, which was defined as visiting the emergency department or being hospitalized for cannabis-related causes. These included “mental and behavioral disorders due to use of cannabis” or “poisoning by or adverse effects of cannabis, including derivatives,” as classified by the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). Adverse effects may include, for example, psychotic symptoms and cannabis hyperemesis syndrome, which is characterized by gastrointestinal symptoms like nausea and vomiting. The researchers also used diagnoses of cannabis use disorder, as classified by the ICD-10 and Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), to identify psychiatric hospitalizations related, at least in part, to cannabis use disorder. Because the research team was also interested in comparing the risk of death between other types of substance use disorders, they identified individuals receiving hospital-based care with the main or contributing reason for the visit being related to other substances, such as alcohol, opioids, and stimulants, as defined by the ICD-10 and DSM-5.
The main outcomes of interest were death for any reason and death for a specific cause. Data on overall mortality was pulled from the Registered Persons Database and was examined until December 2022, reflecting data availability. Data on causes of death were pulled from the Office of the Registrar General Vital Statistics and was examined until December 2018, also reflecting data availability. Causes of death were identified using ICD-10 diagnostic codes on death certificates. Both immediate and underlying causes of death were included. The following causes were examined: alcohol poisoning, opioid poisoning, poisoning by other drugs, trauma (subdivided into motor vehicle collisions, fire, drowning, and falls and other accidental injuries), intentional self-harm, cancer (subdivided into lung cancer), infection, and diseases of the circulatory system, respiratory system, and gastrointestinal system.
Covariates, or variables included in the statistical models to adjust for their potential influence, included sociodemographic information and co-morbid mental health, substance use, and chronic health conditions, and was obtained from government and public databases. Sociodemographic information included age, sex, rural residence, neighborhood income, and whether they immigrated to Canada since 1985. Mental health and substance use conditions were assessed in the 3 years prior to the hospital-based index episode of care in the current study and included outpatient mental health visits and visiting the emergency department or being hospitalized for any other substance use and for any mental disorders. Chronic health conditions were also assessed in the prior 3 years and included hypertension, diabetes, asthma, cardiovascular disease, chronic obstructive pulmonary disease (COPD), cancer, kidney failure, and dementia.
For the primary statistical analyses, the research team matched individuals with a cannabis use disorder with members of the general population on age, sex, and date of hospital-based care in 1 to 4 ratio. They first compared the risk of death for any reason between individuals who received hospital-based care for a cannabis-related reason to the matched general population who did not receive hospital-based care. Then, they adjusted the models for the 3 categories of covariates (socio-demographics, mental health and substance use, and chronic health conditions). In secondary analyses, the researchers compared the risk of death between individuals who received hospital-based care for a cannabis-related reason to those who received hospital-based care for a different type of substance use disorder.
A total of 106,994 individuals who received hospital-based care for a cannabis-related reason were included in the analyses. These individuals were matched with 420,978 members of the general population. The annual number of people who received hospital-based for cannabis use increased by 6-fold during the study period, with 456 individuals receiving care in 2006 and 3,263 individuals receiving care in 2021.
A total of 519,528 individuals who received hospital-based care for a different type of substance use disorder were included in the secondary analyses. Of these, the majority had a diagnosis of alcohol use disorder (72%), while 15% had a stimulant use disorder and 14% had an opioid use disorder.
Differences between those who received hospital-based care for a cannabis-related reason and those in the general population
There were no differences between the hospital and general population groups for age and sex. In both groups, approximately 62.5% were men and their average age was 30 years old. Also, in both groups, the risk of death was higher among men and increased with age.
People who received hospital-based care for a cannabis-related reason were more likely to live in low-income neighborhoods than those in matched general population, with 29% of individuals who received hospital-based care living in the lowest income quintile compared to 20% from the matched general population. They were also more likely to be long-term residents of Canada than those in the matched general population, with 91% who received hospital-based care being a long-term resident compared to 82% from the matched general population.
Additionally, people who received hospital-based care for a cannabis-related reason were more
likely to have visited the emergency department or have been hospitalized for any substance use-related reason (39% vs 2%) or a mental disorder (including self-harm; 35% vs. 3%) in the past 3 years than those in the matched general population. They were also more likely to have been diagnosed with several chronic conditions in the past 3 years, including hypertension, asthma, COPD, cardiovascular disease, and kidney failure than those in the matched general population. However, there were no differences in cancer diagnoses between groups.
Risk of death for people who received hospital-based care for a cannabis-related reason was higher than for the general population, but lower than for other substance use
Among those receiving hospital-based care for a cannabis-related reason, 3.5% died from any reason within 5 years of care and 5% died within 10 years, compared with less than 1% of individuals from the matched general population at both 5 and 10 years (Figure below). After adjustment for the covariates (i.e., socio-demographics, prior substance use, mental health care, and chronic conditions), the risk of death was still greater for people who received hospital-based care relative to the general population, with almost a 3-fold increased risk within 5 years for those who received hospital-based care in the fully adjusted model.
Additionally, people who received hospital-based care for a cannabis-related reason had a higher risk of death from all of the causes examined than those in the matched general population, but the causes associated with the highest risks for death were death by suicide, with almost a 10-fold increased risk, trauma, with a 4.5-fold increased risk, and opioid poisoning, with a 5-fold increased risk.
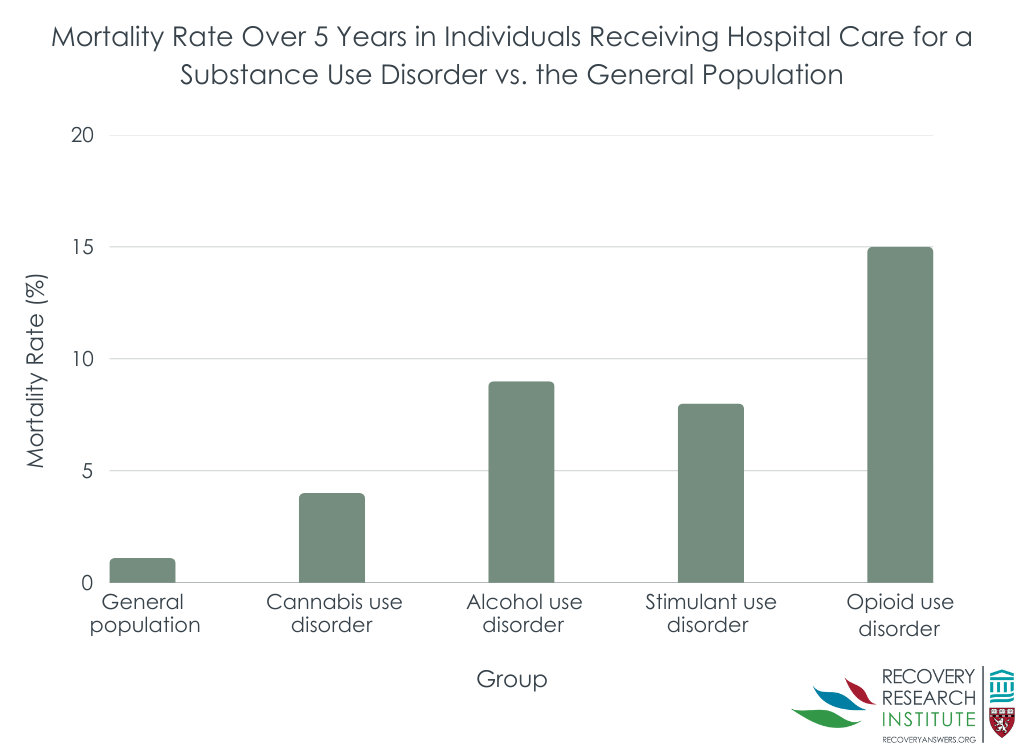
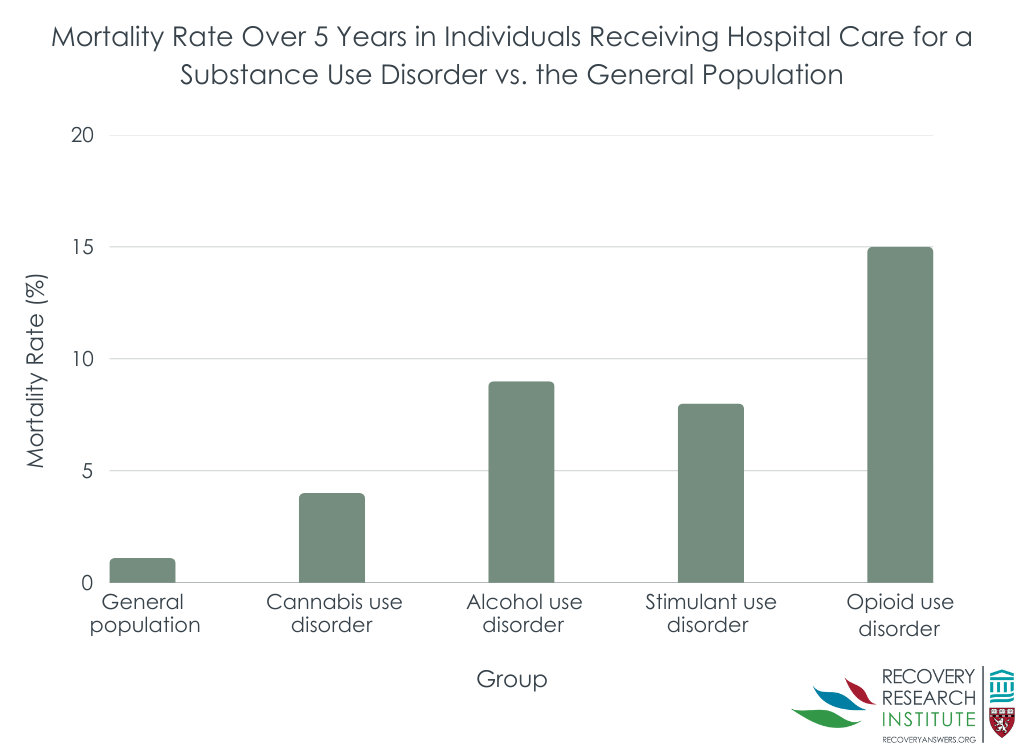
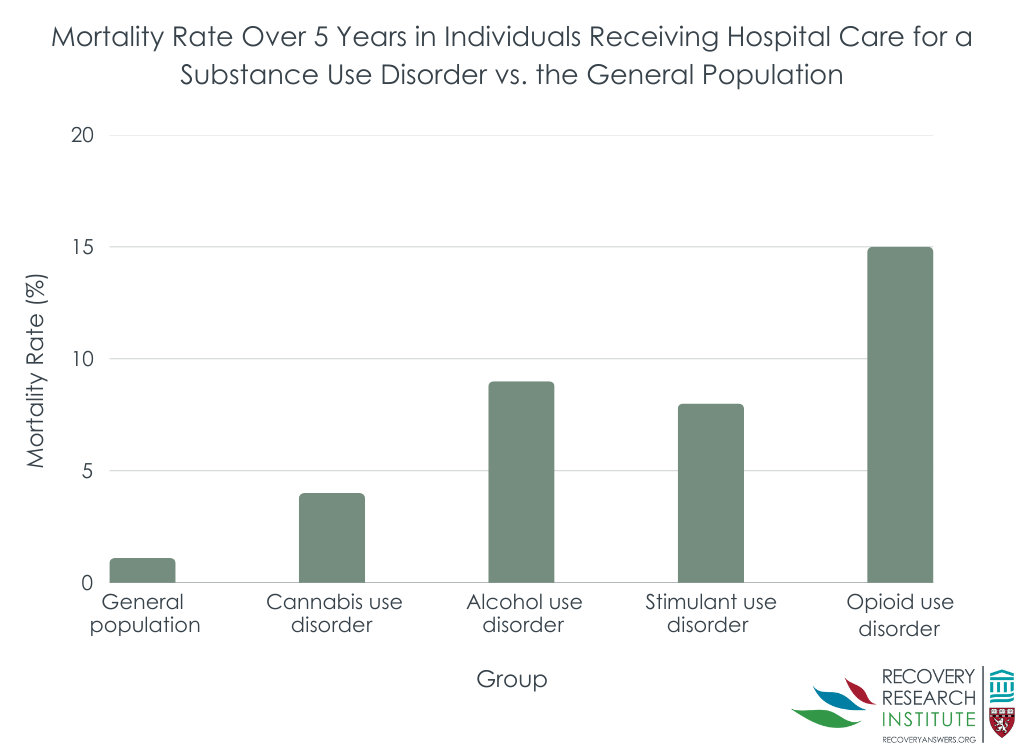
People who received hospital-based care for a different substance use disorder were at a higher risk of death within 5 years of care than those who received hospital-based care for a cannabis-related reason (Figure below). Those who received care for an alcohol-, stimulant-, and opioid-related reasons were at a 1.3-fold, 1.7-fold, and 2-fold increased risk, respectively, than those who received care for a cannabis-related reason.
The research team study examined whether receiving hospital-based care for a cannabis-related reason is associated with an increased risk of death within 5 and 10 years of care and how the risk of death compares to receiving hospital-based care for a different substance-related reason. Results showed that people who received hospital-based care for a cannabis-related reason were more likely to die within 5 and 10 years than the general population, even after adjusting for socio-demographics and comorbid conditions. Further, people who received hospital-based care for a substance other than cannabis were at a higher risk of death than those who received care for a cannabis-related reason. This latter finding is not surprising as substances like alcohol can cause greater harms through intoxication and toxicity while opioid use increases risk for drug overdose. It is worth noting that alcohol hospitalizations were associated with higher absolute mortality risk than stimulant hospitalizations, but its mortality odds were slightly lower after adjusting statistically for age (by using a matched comparison group). This is because people hospitalized for alcohol are likely older than those hospitalized for stimulants, and older people overall have greater mortality risk than younger people. Controlling for this general mortality risk of older age somewhat muted the association between alcohol hospitalization and mortality.
This study demonstrated a link between cannabis use-related hospital admissions and increased risk of death that is significantly higher than the general population mortality rate, yet cannabis use may not cause death directly (e.g., through overdose), and the increased risk of death may occur through a variety of other mechanisms. The nature of this observational study precludes making firm conclusions, but the results are consistent with prior research that has shown that exposure to cannabis and intoxication from it is associated with increased risks of death from fatal car accidents and suicide. This suggests that cannabis use may indirectly increase risk of death and that it is associated with risky behaviors and mental health conditions which, in turn, also increase the risk of death (e.g., by suicide).
However, the direction of effect is unclear. For instance, cannabis use may increase depression symptoms or experiencing depression symptoms may lead to self-medication through cannabis use. While some research suggests that cannabis use increases depression symptoms, this direction of effect was reversed in young adults who have experienced adverse childhood events. Accordingly, future research is needed that uses study designs that allow researchers to draw conclusions regarding the direction of effects and causality. Irrespective of the direction of effects, cannabis-related hospitalizations are a marker for mortality risk, clinically warranting in-depth assessment for both addiction and mental health treatment.
People who received hospital-based care for a cannabis-related reason had a considerably higher risk of mortality than the general population, but lower risk than others receiving hospital-based care for a substance other than cannabis such as alcohol or opioids. Given that suicide and opioid poisoning were among the most common reasons why those with cannabis-related hospitalizations died prematurely, this reflects a need to holistically address the needs and health/mental health conditions of people who use cannabis and other drugs.
Myran, D. T., Pugliese, M., McDonald, A. J., Xiao, J., Fischer, B., Finkelstein, Y., Tanuseputro, P., Firth, J., Pakpour, A., Hsu, C., Chang, W., & Solmi, M. (2025). Cannabis use disorder emergency department visits and hospitalizations and 5-year mortality. JAMA Network Open, 8(2). doi: 10.1001/jamanetworkopen.2024.57852.
l
Cannabis is one of the most commonly used psychoactive substances worldwide. With greater availability in retail locations and higher potency cannabis strains as a function of legalized recreational cannabis in many US states and Canada more broadly, more hazardous forms of cannabis use – such as daily use – are on the rise. While public perception of cannabis use is that it is relatively harmless and can even be beneficial, research shows that people who use cannabis are at a higher risk of fatal car accidents when driving under the influence and are at higher risks of self-harm and suicide. Cannabis use has also been linked to the development of mental health disorders, with the largest associations being shown with psychosis and schizophrenia.
Cannabis use may also increase the risk of early death. Indeed, research from Denmark, the UK, and Sweden have all found elevated mortality risks among people who use cannabis heavily or frequently, and who have cannabis use disorder. The current study examined whether people who received hospital-based care for a cannabis-related reason in Ontario, Canada had a higher risk of death over a 10-year period at the population-level. This research can help shed light on the potential association between cannabis use and mortality.
The research team examined whether receiving hospital-based care for a cannabis-related reason was associated with an increased risk of death. This was a retrospective, population-level study in which the general population in Ontario, Canada, was compared to those receiving hospital-based care for cannabis between 2006 and 2021.
The main predictor in the study was receiving hospital-based care for cannabis use, which was defined as visiting the emergency department or being hospitalized for cannabis-related causes. These included “mental and behavioral disorders due to use of cannabis” or “poisoning by or adverse effects of cannabis, including derivatives,” as classified by the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). Adverse effects may include, for example, psychotic symptoms and cannabis hyperemesis syndrome, which is characterized by gastrointestinal symptoms like nausea and vomiting. The researchers also used diagnoses of cannabis use disorder, as classified by the ICD-10 and Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), to identify psychiatric hospitalizations related, at least in part, to cannabis use disorder. Because the research team was also interested in comparing the risk of death between other types of substance use disorders, they identified individuals receiving hospital-based care with the main or contributing reason for the visit being related to other substances, such as alcohol, opioids, and stimulants, as defined by the ICD-10 and DSM-5.
The main outcomes of interest were death for any reason and death for a specific cause. Data on overall mortality was pulled from the Registered Persons Database and was examined until December 2022, reflecting data availability. Data on causes of death were pulled from the Office of the Registrar General Vital Statistics and was examined until December 2018, also reflecting data availability. Causes of death were identified using ICD-10 diagnostic codes on death certificates. Both immediate and underlying causes of death were included. The following causes were examined: alcohol poisoning, opioid poisoning, poisoning by other drugs, trauma (subdivided into motor vehicle collisions, fire, drowning, and falls and other accidental injuries), intentional self-harm, cancer (subdivided into lung cancer), infection, and diseases of the circulatory system, respiratory system, and gastrointestinal system.
Covariates, or variables included in the statistical models to adjust for their potential influence, included sociodemographic information and co-morbid mental health, substance use, and chronic health conditions, and was obtained from government and public databases. Sociodemographic information included age, sex, rural residence, neighborhood income, and whether they immigrated to Canada since 1985. Mental health and substance use conditions were assessed in the 3 years prior to the hospital-based index episode of care in the current study and included outpatient mental health visits and visiting the emergency department or being hospitalized for any other substance use and for any mental disorders. Chronic health conditions were also assessed in the prior 3 years and included hypertension, diabetes, asthma, cardiovascular disease, chronic obstructive pulmonary disease (COPD), cancer, kidney failure, and dementia.
For the primary statistical analyses, the research team matched individuals with a cannabis use disorder with members of the general population on age, sex, and date of hospital-based care in 1 to 4 ratio. They first compared the risk of death for any reason between individuals who received hospital-based care for a cannabis-related reason to the matched general population who did not receive hospital-based care. Then, they adjusted the models for the 3 categories of covariates (socio-demographics, mental health and substance use, and chronic health conditions). In secondary analyses, the researchers compared the risk of death between individuals who received hospital-based care for a cannabis-related reason to those who received hospital-based care for a different type of substance use disorder.
A total of 106,994 individuals who received hospital-based care for a cannabis-related reason were included in the analyses. These individuals were matched with 420,978 members of the general population. The annual number of people who received hospital-based for cannabis use increased by 6-fold during the study period, with 456 individuals receiving care in 2006 and 3,263 individuals receiving care in 2021.
A total of 519,528 individuals who received hospital-based care for a different type of substance use disorder were included in the secondary analyses. Of these, the majority had a diagnosis of alcohol use disorder (72%), while 15% had a stimulant use disorder and 14% had an opioid use disorder.
Differences between those who received hospital-based care for a cannabis-related reason and those in the general population
There were no differences between the hospital and general population groups for age and sex. In both groups, approximately 62.5% were men and their average age was 30 years old. Also, in both groups, the risk of death was higher among men and increased with age.
People who received hospital-based care for a cannabis-related reason were more likely to live in low-income neighborhoods than those in matched general population, with 29% of individuals who received hospital-based care living in the lowest income quintile compared to 20% from the matched general population. They were also more likely to be long-term residents of Canada than those in the matched general population, with 91% who received hospital-based care being a long-term resident compared to 82% from the matched general population.
Additionally, people who received hospital-based care for a cannabis-related reason were more
likely to have visited the emergency department or have been hospitalized for any substance use-related reason (39% vs 2%) or a mental disorder (including self-harm; 35% vs. 3%) in the past 3 years than those in the matched general population. They were also more likely to have been diagnosed with several chronic conditions in the past 3 years, including hypertension, asthma, COPD, cardiovascular disease, and kidney failure than those in the matched general population. However, there were no differences in cancer diagnoses between groups.
Risk of death for people who received hospital-based care for a cannabis-related reason was higher than for the general population, but lower than for other substance use
Among those receiving hospital-based care for a cannabis-related reason, 3.5% died from any reason within 5 years of care and 5% died within 10 years, compared with less than 1% of individuals from the matched general population at both 5 and 10 years (Figure below). After adjustment for the covariates (i.e., socio-demographics, prior substance use, mental health care, and chronic conditions), the risk of death was still greater for people who received hospital-based care relative to the general population, with almost a 3-fold increased risk within 5 years for those who received hospital-based care in the fully adjusted model.
Additionally, people who received hospital-based care for a cannabis-related reason had a higher risk of death from all of the causes examined than those in the matched general population, but the causes associated with the highest risks for death were death by suicide, with almost a 10-fold increased risk, trauma, with a 4.5-fold increased risk, and opioid poisoning, with a 5-fold increased risk.
People who received hospital-based care for a different substance use disorder were at a higher risk of death within 5 years of care than those who received hospital-based care for a cannabis-related reason (Figure below). Those who received care for an alcohol-, stimulant-, and opioid-related reasons were at a 1.3-fold, 1.7-fold, and 2-fold increased risk, respectively, than those who received care for a cannabis-related reason.
The research team study examined whether receiving hospital-based care for a cannabis-related reason is associated with an increased risk of death within 5 and 10 years of care and how the risk of death compares to receiving hospital-based care for a different substance-related reason. Results showed that people who received hospital-based care for a cannabis-related reason were more likely to die within 5 and 10 years than the general population, even after adjusting for socio-demographics and comorbid conditions. Further, people who received hospital-based care for a substance other than cannabis were at a higher risk of death than those who received care for a cannabis-related reason. This latter finding is not surprising as substances like alcohol can cause greater harms through intoxication and toxicity while opioid use increases risk for drug overdose. It is worth noting that alcohol hospitalizations were associated with higher absolute mortality risk than stimulant hospitalizations, but its mortality odds were slightly lower after adjusting statistically for age (by using a matched comparison group). This is because people hospitalized for alcohol are likely older than those hospitalized for stimulants, and older people overall have greater mortality risk than younger people. Controlling for this general mortality risk of older age somewhat muted the association between alcohol hospitalization and mortality.
This study demonstrated a link between cannabis use-related hospital admissions and increased risk of death that is significantly higher than the general population mortality rate, yet cannabis use may not cause death directly (e.g., through overdose), and the increased risk of death may occur through a variety of other mechanisms. The nature of this observational study precludes making firm conclusions, but the results are consistent with prior research that has shown that exposure to cannabis and intoxication from it is associated with increased risks of death from fatal car accidents and suicide. This suggests that cannabis use may indirectly increase risk of death and that it is associated with risky behaviors and mental health conditions which, in turn, also increase the risk of death (e.g., by suicide).
However, the direction of effect is unclear. For instance, cannabis use may increase depression symptoms or experiencing depression symptoms may lead to self-medication through cannabis use. While some research suggests that cannabis use increases depression symptoms, this direction of effect was reversed in young adults who have experienced adverse childhood events. Accordingly, future research is needed that uses study designs that allow researchers to draw conclusions regarding the direction of effects and causality. Irrespective of the direction of effects, cannabis-related hospitalizations are a marker for mortality risk, clinically warranting in-depth assessment for both addiction and mental health treatment.
People who received hospital-based care for a cannabis-related reason had a considerably higher risk of mortality than the general population, but lower risk than others receiving hospital-based care for a substance other than cannabis such as alcohol or opioids. Given that suicide and opioid poisoning were among the most common reasons why those with cannabis-related hospitalizations died prematurely, this reflects a need to holistically address the needs and health/mental health conditions of people who use cannabis and other drugs.
Myran, D. T., Pugliese, M., McDonald, A. J., Xiao, J., Fischer, B., Finkelstein, Y., Tanuseputro, P., Firth, J., Pakpour, A., Hsu, C., Chang, W., & Solmi, M. (2025). Cannabis use disorder emergency department visits and hospitalizations and 5-year mortality. JAMA Network Open, 8(2). doi: 10.1001/jamanetworkopen.2024.57852.
l
Cannabis is one of the most commonly used psychoactive substances worldwide. With greater availability in retail locations and higher potency cannabis strains as a function of legalized recreational cannabis in many US states and Canada more broadly, more hazardous forms of cannabis use – such as daily use – are on the rise. While public perception of cannabis use is that it is relatively harmless and can even be beneficial, research shows that people who use cannabis are at a higher risk of fatal car accidents when driving under the influence and are at higher risks of self-harm and suicide. Cannabis use has also been linked to the development of mental health disorders, with the largest associations being shown with psychosis and schizophrenia.
Cannabis use may also increase the risk of early death. Indeed, research from Denmark, the UK, and Sweden have all found elevated mortality risks among people who use cannabis heavily or frequently, and who have cannabis use disorder. The current study examined whether people who received hospital-based care for a cannabis-related reason in Ontario, Canada had a higher risk of death over a 10-year period at the population-level. This research can help shed light on the potential association between cannabis use and mortality.
The research team examined whether receiving hospital-based care for a cannabis-related reason was associated with an increased risk of death. This was a retrospective, population-level study in which the general population in Ontario, Canada, was compared to those receiving hospital-based care for cannabis between 2006 and 2021.
The main predictor in the study was receiving hospital-based care for cannabis use, which was defined as visiting the emergency department or being hospitalized for cannabis-related causes. These included “mental and behavioral disorders due to use of cannabis” or “poisoning by or adverse effects of cannabis, including derivatives,” as classified by the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10). Adverse effects may include, for example, psychotic symptoms and cannabis hyperemesis syndrome, which is characterized by gastrointestinal symptoms like nausea and vomiting. The researchers also used diagnoses of cannabis use disorder, as classified by the ICD-10 and Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), to identify psychiatric hospitalizations related, at least in part, to cannabis use disorder. Because the research team was also interested in comparing the risk of death between other types of substance use disorders, they identified individuals receiving hospital-based care with the main or contributing reason for the visit being related to other substances, such as alcohol, opioids, and stimulants, as defined by the ICD-10 and DSM-5.
The main outcomes of interest were death for any reason and death for a specific cause. Data on overall mortality was pulled from the Registered Persons Database and was examined until December 2022, reflecting data availability. Data on causes of death were pulled from the Office of the Registrar General Vital Statistics and was examined until December 2018, also reflecting data availability. Causes of death were identified using ICD-10 diagnostic codes on death certificates. Both immediate and underlying causes of death were included. The following causes were examined: alcohol poisoning, opioid poisoning, poisoning by other drugs, trauma (subdivided into motor vehicle collisions, fire, drowning, and falls and other accidental injuries), intentional self-harm, cancer (subdivided into lung cancer), infection, and diseases of the circulatory system, respiratory system, and gastrointestinal system.
Covariates, or variables included in the statistical models to adjust for their potential influence, included sociodemographic information and co-morbid mental health, substance use, and chronic health conditions, and was obtained from government and public databases. Sociodemographic information included age, sex, rural residence, neighborhood income, and whether they immigrated to Canada since 1985. Mental health and substance use conditions were assessed in the 3 years prior to the hospital-based index episode of care in the current study and included outpatient mental health visits and visiting the emergency department or being hospitalized for any other substance use and for any mental disorders. Chronic health conditions were also assessed in the prior 3 years and included hypertension, diabetes, asthma, cardiovascular disease, chronic obstructive pulmonary disease (COPD), cancer, kidney failure, and dementia.
For the primary statistical analyses, the research team matched individuals with a cannabis use disorder with members of the general population on age, sex, and date of hospital-based care in 1 to 4 ratio. They first compared the risk of death for any reason between individuals who received hospital-based care for a cannabis-related reason to the matched general population who did not receive hospital-based care. Then, they adjusted the models for the 3 categories of covariates (socio-demographics, mental health and substance use, and chronic health conditions). In secondary analyses, the researchers compared the risk of death between individuals who received hospital-based care for a cannabis-related reason to those who received hospital-based care for a different type of substance use disorder.
A total of 106,994 individuals who received hospital-based care for a cannabis-related reason were included in the analyses. These individuals were matched with 420,978 members of the general population. The annual number of people who received hospital-based for cannabis use increased by 6-fold during the study period, with 456 individuals receiving care in 2006 and 3,263 individuals receiving care in 2021.
A total of 519,528 individuals who received hospital-based care for a different type of substance use disorder were included in the secondary analyses. Of these, the majority had a diagnosis of alcohol use disorder (72%), while 15% had a stimulant use disorder and 14% had an opioid use disorder.
Differences between those who received hospital-based care for a cannabis-related reason and those in the general population
There were no differences between the hospital and general population groups for age and sex. In both groups, approximately 62.5% were men and their average age was 30 years old. Also, in both groups, the risk of death was higher among men and increased with age.
People who received hospital-based care for a cannabis-related reason were more likely to live in low-income neighborhoods than those in matched general population, with 29% of individuals who received hospital-based care living in the lowest income quintile compared to 20% from the matched general population. They were also more likely to be long-term residents of Canada than those in the matched general population, with 91% who received hospital-based care being a long-term resident compared to 82% from the matched general population.
Additionally, people who received hospital-based care for a cannabis-related reason were more
likely to have visited the emergency department or have been hospitalized for any substance use-related reason (39% vs 2%) or a mental disorder (including self-harm; 35% vs. 3%) in the past 3 years than those in the matched general population. They were also more likely to have been diagnosed with several chronic conditions in the past 3 years, including hypertension, asthma, COPD, cardiovascular disease, and kidney failure than those in the matched general population. However, there were no differences in cancer diagnoses between groups.
Risk of death for people who received hospital-based care for a cannabis-related reason was higher than for the general population, but lower than for other substance use
Among those receiving hospital-based care for a cannabis-related reason, 3.5% died from any reason within 5 years of care and 5% died within 10 years, compared with less than 1% of individuals from the matched general population at both 5 and 10 years (Figure below). After adjustment for the covariates (i.e., socio-demographics, prior substance use, mental health care, and chronic conditions), the risk of death was still greater for people who received hospital-based care relative to the general population, with almost a 3-fold increased risk within 5 years for those who received hospital-based care in the fully adjusted model.
Additionally, people who received hospital-based care for a cannabis-related reason had a higher risk of death from all of the causes examined than those in the matched general population, but the causes associated with the highest risks for death were death by suicide, with almost a 10-fold increased risk, trauma, with a 4.5-fold increased risk, and opioid poisoning, with a 5-fold increased risk.
People who received hospital-based care for a different substance use disorder were at a higher risk of death within 5 years of care than those who received hospital-based care for a cannabis-related reason (Figure below). Those who received care for an alcohol-, stimulant-, and opioid-related reasons were at a 1.3-fold, 1.7-fold, and 2-fold increased risk, respectively, than those who received care for a cannabis-related reason.
The research team study examined whether receiving hospital-based care for a cannabis-related reason is associated with an increased risk of death within 5 and 10 years of care and how the risk of death compares to receiving hospital-based care for a different substance-related reason. Results showed that people who received hospital-based care for a cannabis-related reason were more likely to die within 5 and 10 years than the general population, even after adjusting for socio-demographics and comorbid conditions. Further, people who received hospital-based care for a substance other than cannabis were at a higher risk of death than those who received care for a cannabis-related reason. This latter finding is not surprising as substances like alcohol can cause greater harms through intoxication and toxicity while opioid use increases risk for drug overdose. It is worth noting that alcohol hospitalizations were associated with higher absolute mortality risk than stimulant hospitalizations, but its mortality odds were slightly lower after adjusting statistically for age (by using a matched comparison group). This is because people hospitalized for alcohol are likely older than those hospitalized for stimulants, and older people overall have greater mortality risk than younger people. Controlling for this general mortality risk of older age somewhat muted the association between alcohol hospitalization and mortality.
This study demonstrated a link between cannabis use-related hospital admissions and increased risk of death that is significantly higher than the general population mortality rate, yet cannabis use may not cause death directly (e.g., through overdose), and the increased risk of death may occur through a variety of other mechanisms. The nature of this observational study precludes making firm conclusions, but the results are consistent with prior research that has shown that exposure to cannabis and intoxication from it is associated with increased risks of death from fatal car accidents and suicide. This suggests that cannabis use may indirectly increase risk of death and that it is associated with risky behaviors and mental health conditions which, in turn, also increase the risk of death (e.g., by suicide).
However, the direction of effect is unclear. For instance, cannabis use may increase depression symptoms or experiencing depression symptoms may lead to self-medication through cannabis use. While some research suggests that cannabis use increases depression symptoms, this direction of effect was reversed in young adults who have experienced adverse childhood events. Accordingly, future research is needed that uses study designs that allow researchers to draw conclusions regarding the direction of effects and causality. Irrespective of the direction of effects, cannabis-related hospitalizations are a marker for mortality risk, clinically warranting in-depth assessment for both addiction and mental health treatment.
People who received hospital-based care for a cannabis-related reason had a considerably higher risk of mortality than the general population, but lower risk than others receiving hospital-based care for a substance other than cannabis such as alcohol or opioids. Given that suicide and opioid poisoning were among the most common reasons why those with cannabis-related hospitalizations died prematurely, this reflects a need to holistically address the needs and health/mental health conditions of people who use cannabis and other drugs.
Myran, D. T., Pugliese, M., McDonald, A. J., Xiao, J., Fischer, B., Finkelstein, Y., Tanuseputro, P., Firth, J., Pakpour, A., Hsu, C., Chang, W., & Solmi, M. (2025). Cannabis use disorder emergency department visits and hospitalizations and 5-year mortality. JAMA Network Open, 8(2). doi: 10.1001/jamanetworkopen.2024.57852.
151 Merrimac St., 4th Floor. Boston, MA 02114