Unplanned Treatment Versus Planned Treatment for Alcohol Use Disorders
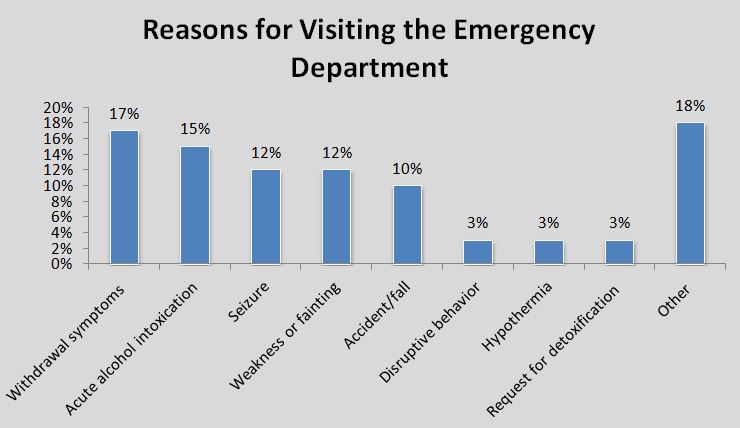
Individuals that have alcohol use disorder are at great risk of ending up in the emergency department, making this setting an ideal place to intervene.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
While current guidelines indicate that patients with alcohol use disorder (AUD) should participate in outpatient services prior to admission to a residential treatment program, admitting patients directly from the emergency department could streamline this process.
This study used a quasi-experimental design to compare the length of hospital stay and 1-year treatment engagement among people who were directly entered into short-term residential treatment (unscheduled patients) to those who received outpatient services prior to admission (scheduled patients).
HOW WAS THIS STUDY CONDUCTED?
This pilot study at a hospital in France allowed patients with alcohol use disorder (AUD) in the emergency department to receive unscheduled 2-week residential treatment directly from the emergency department. The authors referred to this treatment as inpatient detoxification but similar treatment in the United States is considered short-term residential treatment. Enrollment in the pilot program began on January 1, 2011.
Data was collected through retrospective chart review. The unscheduled group consisted of 60 patients who were directly hospitalized from the emergency department. The scheduled group (n=60) followed standard procedures for enrollment in short-term residential treatment, and participants had not visited the emergency department within the last month. Once hospitalized, all individuals participated in a relapse prevention program with group sessions 5x per week.
A monthly outpatient follow-up was offered to all participants after discharge. The authors compared the two groups on length of stay in days and attendance at post-discharge treatment visits.
WHAT DID THIS STUDY FIND?
Study participants in the unscheduled group were found to be significantly older, less frequently employed, less likely to have insurance, and more likely to have a comorbid medical condition than scheduled patients.
Taken together, these differences suggest that the unscheduled group was more clinically severe, on average.
Notably from the study:
- The length of hospital stay was significantly longer for unscheduled patients (20 days) than for scheduled patients (14 days).
- The number of early dropouts was the same between groups with one patient dropping out from each.
- The number of patients attending post-discharge treatment were similar with 34 (57%) of unscheduled and 39 (65%) of scheduled patients attending at least one visit and 13 (22%) of unscheduled and 19 (32%) of scheduled patients attending at least five visits.
- The average number of post-discharge visits was also not statistically different (2.7 visits for the unscheduled group vs. 4.5 visits for the scheduled group).
Despite being more clinically severe and having more medical needs, patients referred to residential treatment directly from the emergency department had similar rates of early dropout and engagement with post-discharge care compared to a group that participated in an outpatient program prior to hospitalization.
This is in contrast to prior studies that found direct emergency referral to residential treatment was associated with higher rates of early dropout (see here). Individuals seeking recovery may be able to bypass the outpatient portion of this process and achieve similar rates of treatment engagement as those who follow standard procedures.
WHY IS THIS STUDY IMPORTANT
A motivational outpatient encounter prior to residential treatment is believed to predict abstinence and higher rates of treatment retention, though these assumptions have not been rigorously tested.
This study will help determine if patients who follow this guideline have better treatment engagement compared to those referred to inpatient treatment directly by the emergency department.
The emergency department may be an ideal place to link people with alcohol use disorder (AUD) directly to residential treatment services.
While this study showed similar rates of treatment engagement for the two groups, it is unknown if this pilot program is effective at reducing drinking and promoting abstinence in this sample of patients with alcohol use disorder (AUD). Treatment engagement is an important outcome to measure but is hard to interpret without more specific information on the nature of this treatment and benefits to the patient.
- LIMITATIONS
-
- This study had a small sample size and may not have had enough statistical power (i.e., the likelihood that a study will detect an effect when there is an effect there to be detected) to detect differences between the two groups in terms of 1-year treatment engagement. For example, 13 (22%) of unscheduled and 19 (32%) of scheduled patients attended at least five outpatient visits, but this result was not statistically significant (i.e., the groups were not considered to be different) despite appearing meaningful to the naked eye.
- Additionally, since this study did not randomize participants, groups may have been different on unmeasured characteristics that could influence detoxification length of stay and post-discharge outpatient attendance. It is unknown how patient characteristics may have impacted results since the authors did not control for any between-group differences in clinical characteristics.
- Other limitations include lack of information on substance use-specific outcomes such as percent days abstinent (i.e., drinking frequency) and number of drinks on each day the individual was not abstinent (i.e., drinking intensity). In other words, while outpatient treatment attendance may help patients stay abstinent, it is difficult to say for sure if this intervention truly benefited patients with alcohol use disorder (AUD).
NEXT STEPS
Future research should investigate the use of immediate linkage to short-term residential treatment from the emergency department with a larger sample size that is adequately powered to detect group differences for relevant outcomes and that uses a prospective and better controlled or randomized controlled trial design.
BOTTOM LINE
- For individuals & families seeking recovery: If seeking recovery from alcohol use disorder (AUD), receiving short-term inpatient treatment directly from the emergency department may result in similar levels of treatment attendance after discharge compared to being referred from outpatient treatment.
- For scientists: This study may not have had adequate statistical power to detect differences between groups in terms of 1-year treatment engagement. Future research on this topic should use a large sample to try to replicate these results.
- For policy makers: Linking individuals with alcohol use disorder (AUD) in the emergency department directly to inpatient treatment is feasible as demonstrated from this pilot program. This may be an ideal place to intervene since having AUD is associated with emergency department visits. Ultimately, effectively assessing and treating AUD, rather than simply addressing the medical consequences of AUD, may help decrease overuse of the emergency department which can avoid unnecessary healthcare spending.
- For treatment professionals and treatment systems: This study showed similar rates of dropout and treatment engagement between groups despite current guidelines suggesting that direct linkage to short-term residential treatment may result in higher rates of dropout. It may be beneficial to allow patients in need to enter inpatient treatment directly from the emergency department.
CITATIONS
Azuar, J., Questel, F., Hispard, E., Scott, J., Vorspan, F., & Bellivier, F. (2016). Hospital Stay and Engagement in Outpatient Follow-Up After Alcohol Emergency Detox: A 1-Year Comparison Study. Alcohol Clin Exp Res, 40(2), 418-421. doi:10.1111/acer.12962

