The Relationship Between Poly-drug Use & Mental Distress
A majority of people seeking treatment for a substance use disorder (SUD) also report clinically significant psychiatric symptoms or have a co-occurring mental health condition.
While it is unknown if substance use influences development of these symptoms or vice versa, the two are interconnected as greater psychiatric severity is correlated with higher frequency of drug use and patients reporting poly-drug use tend to have greater depressive and suicidal symptomatology.
Burdzovic Andreas and colleagues conducted a 10-year longitudinal study to investigate changes in mental distress over time and its association with illicit poly-drug use among patients seeking treatment for substance use disorder (SUD).
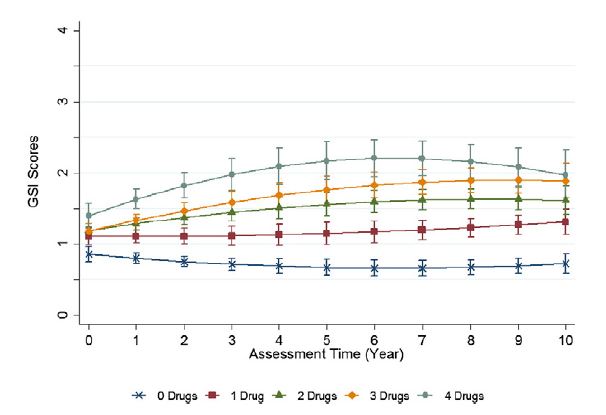
Patients were recruited from residential, outpatient, and opioid substitution therapy (OST) treatment programs from 20 facilities in Oslo, Norway. Participants were eligible if they were admitted for treatment due to illicit drug use. Patients were initially interviewed within two weeks of treatment initiation (n = 481), and again 1 year (n = 428), 2 years (n = 410), 7 years (n = 348), and 10 years (n = 296) after enrolling in the study. Mental distress (anxiety and depression) in the past 7 days was measured with the Hopkins Symptom Checklist. Scores were averaged to obtain Global Severity Index (GSI) scores ranging from 0 to 4 with higher scores indicating greater mental distress.
The authors used the Addiction Severity Index, European version to collect information on substance use during the 30 days prior to each study visit. The four most commonly used illicit substances—heroin, cannabis, sedatives/hypnotics, and amphetamines—were quantified such that a score of 0 indicated use of none of the four drugs in the past month and a score of 4 indicated use of all four drugs in the past month.
At baseline, participants were 68% male and 30.7 years on average. Eighty-two percent had a history of injection drug use, 61% had at least one episode of depression in the past, and 59% had previously experienced an overdose. Over two thirds had used more than one drug in the past month with an average of 2 drugs used. Sixty-two percent used heroin, 59% used cannabis, 51% used sedatives/hypnotics, and 34% used amphetamines. Average GSI was 1.18.
Using multilevel statistical models with poly-drug use as a predictor, and controlling for age and gender, to try to better estimate a unique effect of poly-drug use on psychiatric distress, the authors found that all drug use conditions (i.e., using 1, 2, 3 or 4 drugs) were associated with greater mental distress (i.e., higher GSI score) in a dose-response fashion as GSI estimates increased with increasing number of drugs used.
Authors tested whether the relationship between poly-drug use and psychiatric distress was consistent or whether it changed over the course of the 10 year follow-up period.
Source: (Burdzovic et al., 2015)
Results showed that drug use was associated with changes in mental distress over time. Specifically, using 2, 3, or 4 drugs resulted in significantly increased mental distress over time in comparison to using no drugs such that a greater number of drugs used resulted in a greater increase in mental distress over time. Additionally, the mental distress trajectory for those not using drugs declined significantly over time and mental distress trajectory of participants’ using 1 drug was unchanged over time (see graph above).
IN CONTEXT
Individuals using multiple drugs simultaneously are a high risk population.
Previous studies have shown that such patients have earlier onset of use and more severe clinical profiles than their single-drug using counterparts.
Although there are several nuances here, including aggregating participants from four separate studies, this study is an important addition to the adolescent treatment/recovery literature in understanding unique clinical profiles and needs.
The current study investigated temporal associations between drug use and mental distress in treatment seeking illicit drug users over a rare long-term follow-up period.
- LIMITATIONS
-
- The authors found that declines in mental distress over time occurred only for those reporting no drug use. This finding should be interpreted with the poly-drug use variable in mind as no drug use refers to no reported use of heroin, cannabis, sedatives/hypnotics, or amphetamines in the month prior to the study visit. However, patients may have used any of the aforementioned drugs intermittently between visits, or they may have used alcohol or other drugs (e.g., prescription opioids) not captured by this variable. Given the lack of information on several potential substances of misuse, including alcohol, these findings may generalize only to a subset of patients in a subset of clinical settings.
- While the study points out important information about changes in mental distress over time, no inferences can be drawn regarding the direction of the association; it is still undetermined if mental distress results in multiple drug use or if using more drugs increases mental distress.
- There were quite a few patients who initially entered the study who did not complete the follow up assessments (e.g., a little over 60% at the 10 year follow-up assessment). Despite the limitations, this study adds further knowledge surrounding the potential harms of poly-substance use and its relationship with mental health distress.
BOTTOM LINE
- For individuals & families seeking recovery: Poly-substance users with co-occurring mental health distress may have more complex treatment needs and need to seek help for both concurrently. Abstinence may help alleviate this distress and improve physical and emotional health.
- For scientists: Future studies should consider the role of alcohol use (alone and in combination with other drugs) on mental distress. There is also potential for time-lagged designs examining the effects of drug use on future mental distress and current mental distress on future drug use. Other methods such as propensity score matching and instrumental variable (see an example here) analyses can help disentangle causes from effects.
- For policy makers: Patients using 2 or more illicit drugs measured in this study had increasing mental health symptoms across the 10 year follow-up. These individuals are likely to suffer greater health consequences over time and confer a greater burden to the health care system. Consider funding innovative and targeted recovery support programs (e.g., more assertive continuing care and recovery management checkups; see Dennis and Scott, 2012) across several years for this group of patients.
- For treatment professionals and treatment systems: Approaches that address the intersection between substance use and mental health may be necessary for patients to achieve the best outcomes.
CITATIONS
Burdzovic Andreas, J., Lauritzen, G., & Nordfjaern, T. (2015). Co-occurrence between mental distress and poly-drug use: A ten year prospective study of patients from substance abuse treatment. Addict Behav, 48, 71-78. doi: 10.1016/j.addbeh.2015.05.001

