The Impact of Personal Views on Naltrexone Prescribing Patterns
Naltrexone, a medication used for the treatment of alcohol and opioid use disorders, has gained support from the scientific community since its approval by the U.S. Food and Drug Administration (FDA) in 1994.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Research has shown naltrexone has small to medium effects (meaning the average study patient getting naltrexone has better alcohol outcomes than 58 to 69% of patients getting a placebo medication), and, in some programs, it is considered a first-line option for individuals with alcohol use disorder (as well as opioid use disorder in certain cases) when combined with psychosocial treatment.
Despite the general consensus that naltrexone can be useful in reducing drinking (see here for a Cochrane review), there is an implementation gap with low rates of use by treatment facilities—only 18% of facilities surveyed by SAMHSA for the National Survey of Substance Abuse Treatment Services reported any use of naltrexone.
HOW WAS THIS STUDY CONDUCTED?
Overall, the study sought to explore counselor attitudes on addiction responsibility and naltrexone use through the use of a vignette-based survey. The authors recruited participants through an online survey and screened for trained addiction counselors who worked with persons with various substance addictions currently or in the past.
92% of participants completed a survey assessing agreement on a scale from 1(strongly disagree) to 5 (strongly agree) with six objections to the use of naltrexone:
- Paul will be unlikely to comply with taking the medication.
- The medication’s side effects (which include nausea, headache, dizziness, anxiety and a small risk of withdrawal symptoms) are not worth its benefits.
- There’s a risk that Paul will use opioids that interfere with the medication and cause serious side effects.
- Naltrexone will treat the symptoms of Paul’s alcoholism, but it will not improve the underlying causes of his alcohol abuse.
- Overcoming alcoholism without the use of medication will strengthen Paul’s resolve and willpower.
- The medication will diminish Paul’s motivation to help himself and participate in the 12-step program
Additionally, the survey assessed views about responsibility for onset of alcohol use and views about responsibility for recovery, and how these views related to the extent to which counselors agreed with these six objections.
WHAT DID THIS STUDY FIND?
Clinician’s attitudes toward addiction & medications approved to treat it are critical for treatment delivery & recovery.
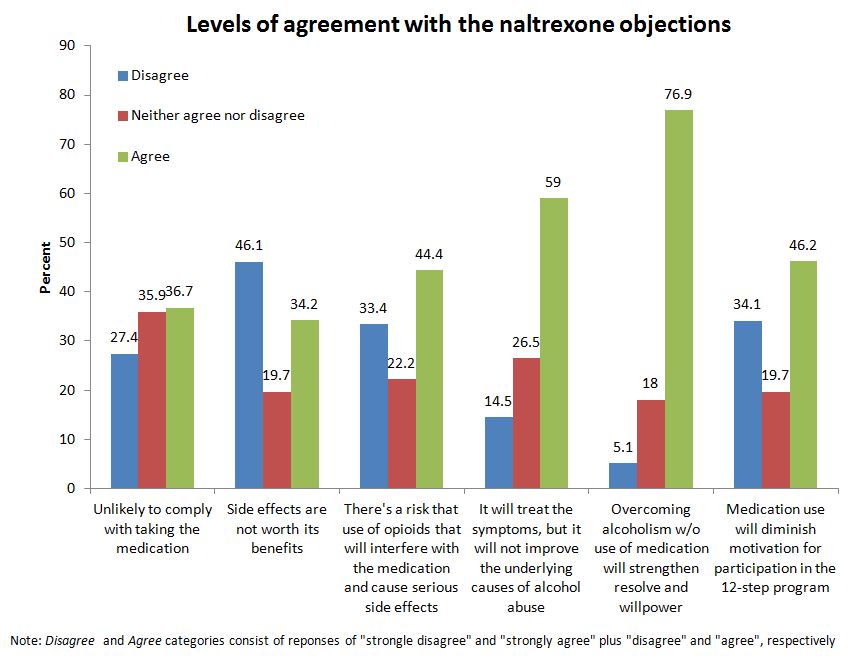
While most counselor characteristics (e.g., gender, age, years working in substance use treatment) failed to predict agreement with the naltrexone objections, treating a higher percentage of out of pockets clients was significantly associated with greater agreement with the objection that naltrexone will treat the symptoms of alcohol addiction but will not treat the underlying causes (number 4), over and above views about responsibility.
This means the relationship between having clients that self-pay and this objection to naltrexone is not likely due to chance alone.
When examining views about responsibility as predictors of objection to the naltrexone statements, the authors found that assigning more responsibility to a person for becoming addicted to alcohol or other drugs was significantly associated with stronger agreement with objections 1, 2, 4, and 6. Assigning higher responsibility to a person for recovery from their addiction was only related to stronger agreement to objection 5.
This study adds to our understanding of recovery by examining provider’s attitudes as well as the connection between their beliefs about addiction onset and offset and their attitudes toward the use of medications in substance use disorder (SUD) treatment.
While assignment of greater responsibility for alcohol addiction was associated with multiple objections to the use of naltrexone, this relationship was largely driven by assigning responsibility for addiction onset rather than recovery which is consistent with the disease model of addiction.
A study in Ukranian jails found that only 25% viewed medication as an effective treatment. Another study assessing attitudes of policy makers and treatment providers in Ohio found that negative attitudes about agonist medications was a main barrier for implementing buprenorphine-naloxone (Suboxone) treatment. Studies such as these show that, despite the existence of evidence-based treatments, there are still implementation barriers such as negative attitudes by providers that must be addressed before they can reach their full potential.
WHY IS THIS STUDY IMPORTANT
There are two main conceptual models characterizing addiction:
- The first recognizes addiction as a symptom of a disease; the individual is responsible for the initial choice to begin to use drugs but their genetics influences their experience of the drug (e.g., the degree to which it is rewarding) and then drug-induced biological changes in the brain affect their ability to control use of the drug.
- The second portrays the individual as an addict with lack of willpower and self-control. In this view, the individual is wholly responsible for initiating and failing to discontinue use, and thus more personally to blame. Addiction counselors may align with either model—or a combination—depending on personal beliefs.
With this framework in mind, this study examined if these views were related to objections to the use of naltrexone in treatment facilities. Since naltrexone uptake in clinical practice is currently low, it is important to determine how these viewpoints may ultimately impede or facilitate patient care.
In this study, assigning higher individual responsibility for addiction was associated with having more negative views about naltrexone, suggesting counselor views of addiction responsibility may impact how they choose to deliver care. For example, some counselors holding negative opinions of naltrexone may fail to discuss this treatment option. This can be particularly harmful for patients who are unaware of this medication but could benefit from its use.
Interventions targeting counselors’ beliefs about the nature of addiction could influence their attitudes toward naltrexone and ultimately their facilitation of its use.
- LIMITATIONS
-
- The findings from this study are correlational and should be interpreted as such. This does not mean that certain viewpoints about addiction responsibility will necessarily cause a provider to object to the use of naltrexone.
- Additionally, the direction of this relationship cannot be determined; it is unknown if views about addiction responsibility may create negative opinions about naltrexone or vice versa. More information is needed about the relationship between these beliefs and and real-world behaviors such as experience prescribing or referring a patient to a physician who can prescribe naltrexone.
NEXT STEPS
Future research should focus on how negative views of naltrexone, and the exact nature of those views, might impact actual prescriptions of naltrexone. More work is needed to understand reasons for why only 18% of programs actually use it.
Additionally, information is needed on providers’ past experiences with naltrexone. If this is a pervasive issue in treatment centers, researchers may seek to develop training programs to help standardized practices with a focus on the disease model of addiction.
BOTTOM LINE
- For individuals & families seeking recovery: If you have an alcohol or opioid use disorder, naltrexone may be a treatment option worth considering. Explore different treatment options if a provider is not presenting the full scope of options for substance use disorder treatment.
- For scientists: More research is needed to determine how to scale up the use of naltrexone and what specific factors may make providers reluctant to prescribe it. More research is needed on how willing patients are to take naltrexone if offered and reasons why they may not take it.
- For policy makers: In a cost-effectiveness analysis of naltrexone for the treatment of alcohol dependence (see here), cognitive-behavioral therapy (CBT) plus naltrexone demonstrated an advantage over CBT alone when factoring in superior abstinence rates. While more expensive up front, introducing pharmacotherapy to treatment facilities is likely to save money over time.
- For treatment professionals and treatment systems: Naltrexone is an FDA approved medication for alcohol and opioid use disorders. Exploring this treatment option with your patients may increase the chances that your patients will be exposed to a greater range of effective treatment options that could ultimately be life-saving.
CITATIONS
Johnson, R. A., Lukens, J. M., Kole, J. W., & Sisti, D. A. (2015). Views about responsibility for alcohol addiction and negative evaluations of naltrexone. Subst Abuse Treat Prev Policy, 10, 10. doi: 10.1186/s13011-015-0004-7

