SSRI Citalopram to Treat Patients with Alcohol Use Disorder?
10% of all American adolescents and adults take an antidepressant
However, it is important to understand the effectiveness of antidepressants for individuals with alcohol use disorder, because they are at higher risk for depressive symptoms and major depressive disorder.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Prior meta-analyses have found that the most popular class of antidepressants, selective serotonin reuptake inhibitors (SSRIs), appear not to be effective in treating alcohol use or depressive symptoms among patients with alcohol use disorders (see here and here).
However, some of the more recently developed SSRIs were not included in those studies. In the current study, Charney and colleagues tested in a randomized controlled trial whether the relatively new SSRI, citalopram, is effective for treating depression symptoms among individuals with alcohol use disorders.
HOW WAS THIS STUDY CONDUCTED?
- READ MORE ON STUDY METHODS
-
Authors compared the efficacy of citalopram (40mg per day) to placebo in 265 adult patients (n = 138 vs. 127, respectively) with alcohol use disorder who were receiving psychosocial addiction treatment (one individual and one group session weekly) across 12 weeks. Those with other substance use disorders as well as those taking a psychotropic or anti-craving medication (e.g., naltrexone) were not able to participate. The groups were similar when beginning the study, apart from greater likelihood of requiring alcohol detoxification prior to entering the study in the citalopram condition (44 vs. 26%).
WHAT DID THIS STUDY FIND?
Only 141 of 265 among the study sample remained in treatment across the entire 12 week study. (Though 63 of those who dropped out still provided post-treatment data).
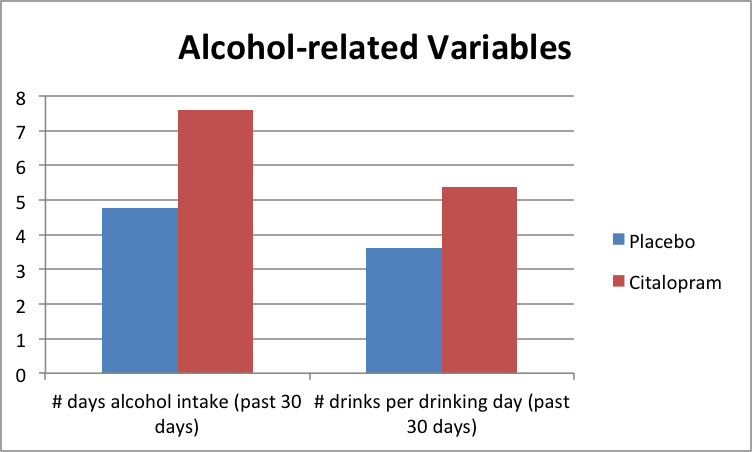
The primary findings were that patients in the citalopram condition did worse than placebo on drinking days and drinks per drinking day & spent more money on alcohol in the month before the post-treatment follow-up interview ($248 vs. 148).
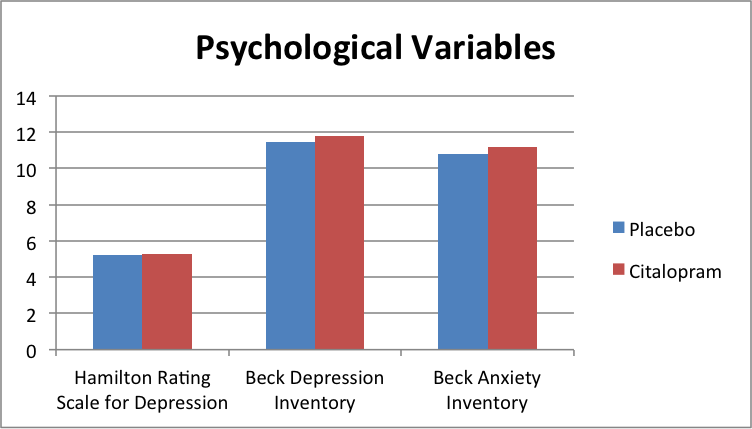
Like prior research on other SSRIs, the citalopram group did no better than the placebo on patients’ self-reported and staff-rated measures of depression and anxiety.
The placebo and citalopram groups were similar on all other markers of severity, and although the citalopram group had a greater proportion of patients that needed detoxification prior to treatment, suggesting they may have been more severe to start, detoxification did not predict whether a patient had a complete vs. partial/no response to treatment (100% reduction in drinking days and drinks per drinking day).
Although SSRIs may be a commonly prescribed medication, this study adds to the body of literature suggesting:
a) they are not effective in helping reduce alcohol consumption among individuals with alcohol use disorder
b) they may not be effective in reducing depressive symptoms for this group of patients either.
WHY IS THIS STUDY IMPORTANT
Approximately 20% of patients that seek treatment for alcohol use disorder have a co-occurring depressive disorder, and countless more present with depressive symptoms that may be related to their alcohol use, or do not quite meet clinical thresholds.
It is important to determine what types of interventions, both pharmacological and psychosocial, can be most helpful.
In combination with many other studies on SSRIs in patients with alcohol use disorder (see meta-analyses mentioned above), available evidence suggests SSRIs are unlikely to perform better than a placebo medication, on average, for alcohol use and depressive symptoms in patients receiving treatment for AUD.
Other antidepressants (e.g., tricyclic) appear to be more effective medications in treating depressive symptoms in those with alcohol use disorder. As the study authors suggest, however, SSRIs still could be considered once patients are abstinent for a period of time (e.g., 30 days).
- LIMITATIONS
-
- Only about half of the patients completed the treatment suggesting medication adherence may not have been adequate. However, because the trial’s findings were generally consistent with other studies of SSRIs, it increases confidence that the effect was not due to poor medication adherence. More importantly, poor medication adherence among those with AUD in research studies may reflect what happens in real-world clinical settings.
- Also, the study authors only were able to assess 77% of participants at the end of treatment; however, they used a sophisticated statistical procedure called “multiple imputation” to fill in these missing data. The pattern of study findings were similar whether authors used this multiple imputation procedure or analyzed only those who provided complete data. Again, this raises confidence that the research was methodologically sound and the findings were an accurate reflection of how patients responded to citalopram.
BOTTOM LINE
- For individuals & families seeking recovery: An SSRI antidepressant like citalopram is unlikely to improve alcohol use and may actually make it worse. In the case of comorbidity, these antidepressants may not help improve your depression either. If you are interested in a medication to help with your depression, consider asking your doctor about a non-SSRI antidepressant medications.
- For scientists: More research on non-SSRI antidepressants for individuals with alcohol use disorder and depressive symptoms or co-occurring depressive disorders is needed (see here for results of a recent pilot study) to see if multimodal therapy can enhance remission rates.
- For policy makers: Consider funding research to develop and evaluate novel pharmacological treatments for patients with co-occurring alcohol use and depressive symptoms and disorders.
- For treatment professionals and treatment systems: SSRIs are unlikely to be effective for patients with alcohol use disorder; other antidepressant medications may be considered in patients with clinically significant depression but will need to weighed against other potential side effects and risk associated with taking these medications.
CITATIONS
Charney, D. A., Heath, L. M., Zikos, E., Palacios-Boix, J., & Gill, K. J. (2015). Poorer Drinking Outcomes with Citalopram Treatment for Alcohol Dependence: A Randomized, Double-Blind, Placebo-Controlled Trial. Alcohol Clin Exp Res. doi:10.1111/acer.12802

