New Quality Indicator for Adolescent Addiction Treatment
Given the lack of quality indicators for adolescent substance use disorder treatment facilities, parents seeking treatment for their child may not know what to look for when deciding on which facility or program is best for their child’s needs.
Quality indicators are practices or services, the presence of which, are known to produce better client outcomes but these are not universally implemented.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
A majority of adolescents entering addiction treatment report having mental health difficulties (see here) or a diagnosed co-occurring psychiatric disorder (e.g., conduct disorder, major depressive disorder, or attention-deficit/hyperactivity disorder; see here), and these adolescents often need more services (e.g., more individual therapy sessions) to achieve outcomes similar to adolescents without co-occurring psychiatric disorders.
One important question is whether facilities that offer mental health services in addition to traditional addiction treatment may be better equipped to address theses adolescents’ needs.
Ramchand and colleagues tested if adolescent substance use disorder (SUD) treatment programs that offered full or partial mental health services had better substance use and mental health outcomes than those receiving services at a facility without mental health services. If results suggest greater benefit from facilities with mental health services, provision of these services may serve as a quality indicator for adolescent SUD treatment facilities.
HOW WAS THIS STUDY CONDUCTED?
This study included 50 facilities receiving funding from the Substance Abuse and Mental Health Services Administration (SAMHSA) Center for Substance Abuse Treatment between 1998 and 2008. Facilities were required to collect data on clients (N = 6,623) at intake and again 12 months later. Administrative or clinical staff at each facility were asked: “Does this location treat both the substance abuse problems and psychiatric problems of dually diagnosed adolescents?”
Based on these answers, facilities were classified into the following groups:
- full mental health services (i.e., treats all psychiatric conditions)
- partial mental health services (i.e., does not treat severe/persistent mental illness)
- no mental health services.
All clients were adolescents ages 12-18 who attended outpatient programs. The authors used a statistical technique known as propensity score matching as a method of adjusting for baseline differences among clients attending facilities in each of the three categories. This method is used to show that an effect is attributable to the actual treatment (provision of mental health services in this case) and not due to any baseline differences that may exist between the adolescent patients in the three categories (e.g., programs offering mental health services may attract adolescents with more severe mental health difficulties, which may negatively affect their treatment response). Any differences remaining after propensity score weights also were adjusted for statistically in the analysis. The authors also adjusted for two facility characteristics in their analyses, 12-step treatment orientation and motivational incentives as a primary care model.
The four outcomes of interest in this study were:
- Substance use frequency (average proportion of the past 90 days on which alcohol or other drugs were used)
- Substance use problems in the past month
- Health and psychological problems
- Substance-induced health and psychological problems
WHAT DID THIS STUDY FIND?
Thirteen facilities (n = 849 clients) offered full mental health services, 18 facilities (n = 1227 clients) offered partial mental health services, and 19 facilities (n = 1159) did not offer mental health services. Clients were three quarters male, half White, and about half were in treatment for marijuana as their primary substance.
Adolescents attending facilities with mental health services had lower rates of substance use and reported fewer substance use problems at 12-months compared to similar adolescents who attended facilities without any mental health services.
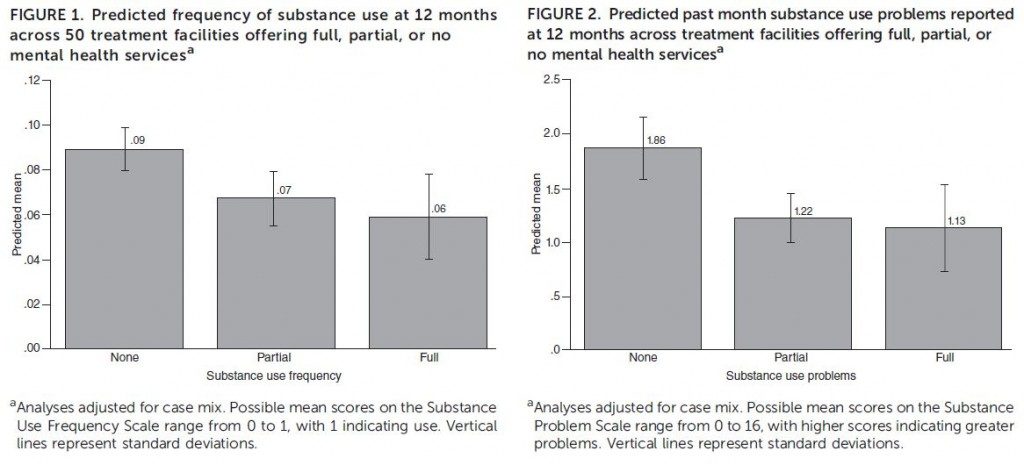
The frequency of substance use problems was significantly different for partial services vs. none and full services vs. none, but there were no significant differences between facilities offering partial or full services. Surprisingly, there were also no significant differences between mental health outcomes across the three types of facilities.
The results of this study showed that attending a facility with full or partial mental health services may result in better client outcomes.
This provides support for using “provision of mental health services” as a quality indicator for assessing adolescent substance use disorder (SUD) treatment facilities.
While there was no apparent benefit for mental health outcomes specifically, the fact that facilities with mental health services are supporting clients in areas beyond substance use disorder (SUD)treatment may be indicative of higher quality care.
Currently, almost half of the adolescent addiction treatment facilities in this study did not provide mental health services. Should this result hold true in other samples, facilities may wish to expand treatment services to address mental health problems in addition to substance use in order to better address addiction.
WHY IS THIS STUDY IMPORTANT
Currently, performance measures indicating quality of substance use disorder (SUD) treatment facilities for adolescents are lacking as client engagement is the only process measure shown to be associated with improved outcomes (see here).
This study is important because it will determine if the provision of mental health services is a quality indicator for adolescent addiction treatment facilities, thus helping adolescents and their families when choosing a treatment program.
For example, a study summarized in a previous RRI Recovery Bulletin showed that adults with post-traumatic stress disorder (PTSD) and substance use disorder (SUD) experienced improved addiction outcomes when receiving an integrated treatment with no differences in mental health symptom improvement when compared to standard care or addiction counseling.
Contrary to these findings, a study on treatment response and outcomes for emerging adults with co-occurring disorders found that those with and without co-occurring disorders had similar post-treatment abstinence rates and psychiatric symptoms. It is possible that the residential treatment program with integrated psychiatric services such as the one described in that study are well equipped to meet the needs of those with co-occurring disorders.
An important treatment implication of this study is that providing mental health services does not mean that mental health outcomes will improve as a result. Rather, it may serve as a “marker”, for better substance use disorder (SUD) treatment outcomes, meaning that a program that provides mental health services may also be providing better quality care for addiction.
Adolescents are a difficult population to treat and high rates of co-occurring disorders should be taken into account when facilities are deciding which evidence-based interventions should be incorporated. Integrated mental health treatments in general have not shown improved mental health outcomes even among adults.
- LIMITATIONS
-
- Despite using several statistical methods to isolate the effect of mental health service provision on client outcomes, some differences remained due to facility level characteristics and possibly due to unmeasured variables that were not accounted for.
- The study also used a single survey question to determine if a facility provided mental health services so there is likely a range in quality and variety of mental health services offered at these facilities.
NEXT STEPS
More research is needed to determine why exactly youth substance use disorder (SUD) treatment programs that also provide mental health services have better SUD treatment outcomes 1 year after patients enter treatment. In addition, more needs to be known about which specific mental health services delivered over what period of time translate into improved mental health outcomes among adolescents. Since the hire and training of staff to deliver adjunctive mental health services can be expensive, future research should determine also if it is cost-effective for the benefits that are achieved and how best to deliver these services (e.g., intensively and/or extensively). Research should also focus on identifying other quality indicators for substance use disorder (SUD) treatment to make it easier for clients to decide which facility or program may be most suitable for their needs.
BOTTOM LINE
- For individuals & families seeking recovery: This study conducted in a sample of adolescents suggests that availability of mental health services may be used as a quality indicator if seeking addiction treatment. Facilities that offer mental health services may also be more effective at increasing abstinence and decreasing substance-related problems than ones that do not offer these services.
- For scientists: The authors of this study used propensity score matching to obtain a best estimate of the isolated effect of mental health service provision on client outcomes. The results showed a benefit for substance use outcomes which supports the use of mental health service provision as a potential marker of greater effectiveness in helping young people with substance use disorders (SUDs).
- For policy makers: Provision of mental health services at adolescent addiction treatment facilities may be a quality indicator that is useful for determining which facilities may provide the most benefit to patients with substance use disorders (SUDs). Consider funding research to better understand why the provision of mental health services does not benefit mental health outcomes but is a marker for greater treatment effectiveness in reducing substance use and related problems.
- For treatment professionals and treatment systems: Although it may be possible to improve your patients’ substance use outcomes by providing mental health services as well, this may simply be a marker for more effective addiction treatment services. Consequently, offering these services does not necessarily translate into improved substance use disorder (SUD) outcomes and we need to know more about what to deliver and how and when to deliver mental health services in order to effect changes in mental health symptoms and functioning.
CITATIONS
Ramchand, R., Griffin, B. A., Hunter, S. B., Booth, M. S., & McCaffrey, D. F. (2015). Provision of mental health services as a quality indicator for adolescent substance abuse treatment facilities. Psychiatr Serv, 66(1), 41-48. doi:10.1176/appi.ps.201300517

