Meditation helps heal the brain during opioid addiction treatment
Mindfulness-based intervention is shown to target brain regions that are implicated in addictive behaviors. Recognizing its potential to rehabilitate these brain structures during addiction treatment, the current study examines the effects of mindfulness on brain structure and clinically relevant behavioral measures in opioid use disorder patients.
WHAT PROBLEM DOES THIS STUDY ADDRESS?
Mindfulness-based intervention is a therapeutic practice that is gaining attention among addiction researchers and clinicians. This intervention is aimed at altering negative patterns of thought and behavior. By discouraging automatic reactions to difficult situations and, instead, approaching them with acceptance and without judgement, individuals learn new ways to think about and react to negative experiences. Studied in a variety of populations, mindfulness is shown to bring about brain changes in regions that play a role in emotion regulation, behavioral control, and reward.
Many of these regions are also implicated in addictive behaviors. Although mindfulness-based intervention may enhance addiction recovery outcomes (e.g., lower rates of substance use and craving), we know less about the structural brain changes that specifically occur in substance use disorder patients after such interventions. To address this gap in the literature, the current study assessed the effects of mindfulness-based intervention on brain structure and clinically relevant behavioral measures (impulsivity, mindfulness, and distress tolerance) in individuals with opioid use disorder.
HOW WAS THIS STUDY CONDUCTED?
The authors conducted an investigation of mindfulness-based intervention in 19 individuals receiving inpatient treatment for opioid use disorder (opioid dependence determined with the Diagnostic and Statistical Manual of Mental Disorders (DSM, 4th edition)). The inpatient addiction treatment unit was located in Cairo, Egypt.
- READ MORE ON STUDY METHODS
-
None of the participants were diagnosed with comorbid psychiatric or neurological disorders.
Upon entry to the treatment facility, patients were assigned to receive inpatient treatment as usual (control group; n=9), or inpatient treatment as usual plus a mindfulness-based intervention (experimental group; n=10). Mindfulness-based intervention began once patients were stabilized (no significant withdrawal symptoms) and occurred over 16 sessions (4 sessions per week 4 weeks).
Treatment as usual consisted of individual and group cognitive behavioral therapy, as well as motivational and social support groups. The mindfulness-based intervention was administered according to an Arabic version of the Mindfulness-Based Stress Reduction workbook, which consists of exercises (e.g., guided meditation, mindful eating) and theoretical teachings that introduced mindfulness, mind and body awareness, mental attitudes and mindful breathing, stress-reduction techniques, impact of stress and anxiety, self-awareness, dealing with difficult emotions, and transforming negative emotions.
Within 48 hours of treatment admission (baseline) and discharge (follow-up after 16 intervention sessions), participants completed a brain scan and various self-report questionnaires. Questionnaires included the Distress Tolerance Questionnaire, which addressed four domains of emotional distress tolerance (tolerance, appraisal, absorption, regulation), and the UPPS-P Impulsive Behavior Scale that assessed four domains of impulsivity (urgency, premeditation, perseverance, and sensation seeking). Brain scans were performed with Magnetic Resonance Imaging (MRI), which produces detailed images of the brain that allow for the measurement of various structural attributes (e.g., size, shape, integrity) in specific brain regions and their networks (regions within the brain that are collectively involved in particular behavioral domains, such as the ‘reward network’).
WHAT DID THIS STUDY FIND?
Mindfulness-based intervention was associated with changes to specific domains of distress tolerance and impulsivity. Although all participants showed improvement on the ‘tolerance’ (i.e. ability to tolerate distressing situations) and ‘absorption’ (i.e. ability to not let distressing thoughts and feelings overwhelm you) scale of the distress tolerance questionnaire, improvements on the ‘regulation’ (i.e. regulating and appropriately responding to distressing feelings) scale were only observed among the mindfulness-based intervention group. A similar pattern was observed for the ‘negative urgency’ (i.e. tendency to act rashly while in a negative mood) scale of the impulsivity questionnaire, with only the intervention group showing significant improvement over time.
Mindfulness-based intervention resulted in increased strength of two structural neural networks. After four weeks of mindfulness, the intervention group showed changes in brain structure that reflected improvement in two networks:
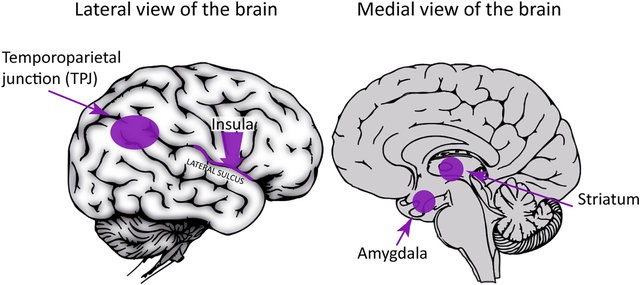
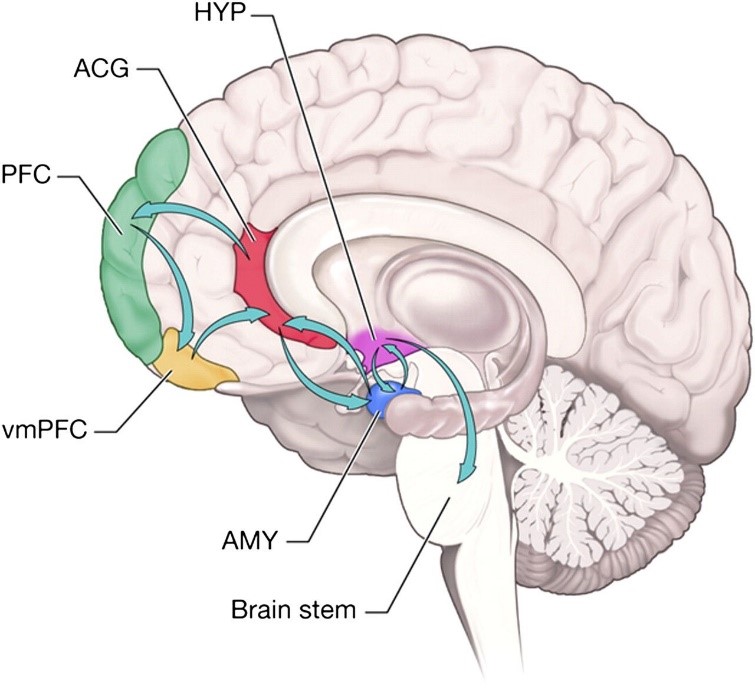
1) Striatal/insular network: regions associated with self-control, inhibition, and stress regulation. Regarding addiction, the striatum is implicated in impulsivity and reward (impulsive pleasure seeking), habit formation and compulsive behavior (compulsive drug seeking). The insula contributes to the regulation of awareness of emotionally salient things in the environment and thought and feelings within one’s self.
CITATION: Lahti, T., Halko, M. L., Karagozoglu, N., & Wincent, J. (2018). Why and how do founding entrepreneurs bond with their ventures? Neural correlates of entrepreneurial and parental bonding. Journal of Business Venturing.
2) Prefrontal cortex / anterior cingulate cortex network: regions that regulate reward systems and play a role in salience, higher-order executive functions, self-control, and awareness. Addiction and impulsivity are often associated with dysfunction of this network.
The control group did not exhibit any significant structural changes to either of these networks after four weeks of treatment as usual.
CITATION: Lahti, T., Halko, M. L., Karagozoglu, N., & Wincent, J. (2018). Why and how do founding entrepreneurs bond with their ventures? Neural correlates of entrepreneurial and parental bonding. Journal of Business Venturing.
Structural network strength was related to impulsivity. In the intervention group, greater prefrontal cortex / anterior cingulate cortex network strength was associated with lower levels of negative urgency, as measured by the impulsivity questionnaire. No significant relationships were observed for the control group.
WHAT ARE THE IMPLICATIONS OF THE STUDY FINDINGS?
This study demonstrates that even short-term mindfulness-based interventions might benefit opioid use disorder patients. Repeated drug use induces changes to frontal and striatal brain circuits that contribute to impulsivity, reward, and self-control. This relatively inexpensive and non-invasive intervention targets these neural networks, thereby enhancing their structural integrity.
By facilitating neural repair during recovery, mindfulness might ultimately aid positive treatment outcomes. In the current study, self-report questionnaires suggested that some of these brain changes were related to decreased impulsivity, a behavior often linked to addiction. Reductions in impulsive behavior can ultimately act as a protective factor for promoting long-term recovery.
Although no additional relationships were revealed between brain structure and behavioral measures, there are several behavioral phenomena that have yet to be investigated and these neural changes have the potential to induce a variety of positive behavioral outcomes. Studies like this are essential for gaining a better understanding of the mechanisms that underlie the effects of behavioral interventions. Mindfulness could ultimately prove a relatively simple and inexpensive adjunct for standard treatment to enhance neural and behavioral recovery. Although further investigation is needed, mindfulness-based interventions show promise for aiding in the rehabilitation of opioid use disorder patients in recovery.
- LIMITATIONS
-
- Given the small sample size and lack of a healthy control group, further investigation is needed to conclude that outcomes were a direct result of the mindfulness-based intervention and that more subtle but meaningful effects were not missed. Prospective studies are especially needed to determine how much mindfulness practice may be needed to induce changes and if these neurobehavioral changes are sustained past the intervention period.
- This study was conducted in Egypt and it is unclear whether these findings would translate cross-culturally, in other nations. Differences between geographic regions with regard to political, cultural, and social beliefs, as well as the primary opioid of use within them could potentially lead to different outcomes and requires further investigation.
- Behavioral measures were limited to select domains and assessed via self-report questionnaires. Therefore, it is unclear whether observed neurostructural improvement can facilitate other beneficial behavioral changes. Additionally, all participants were inpatients and whether or not these outcomes would translate to outpatient populations is unclear.
BOTTOM LINE
- For individuals & families seeking recovery: Although substance use disorders are accompanied by neurobehavioral impairment, treatments are available to rehabilitate the brain and associated behaviors. This area of study is in its early stages, but mindfulness-based intervention has the potential to rehabilitate parts of the brain that are harmed after repeated substance use. This neural rehabilitation may thereby help to reduce negative impulsive behaviors, and has the potential to ultimately aid in the prevention of relapse. More research is needed to determine the full potential of mindfulness, but this line of study shows promise.
- For scientists: Mindfulness-based interventions are shown to bring about brain changes in regions that play a role in emotion regulation, behavioral control, and addiction, but few studies have assessed these changes in substance use disorder patients. This study suggests that mindfulness has significant potential to facilitate the rehabilitation of frontal and striatal neural networks, which can ultimately lessen impulsive traits that are risk factors for addiction. Given the observation of strengthened neural networks post intervention, it is necessary to advance this line of research and determine the various behavioral changes that accompany this neurostructural improvement, whether findings can be replicated in larger controlled trials, in different cultural contexts, and treatment settings. Prospective research will also help determine the extent to which these neurobehavioral benefits last beyond treatment.
- For policy makers: Neural and behavioral deficits commonly accompany substance use disorders and these impairments can negatively impact recovery processes. Mindfulness-based interventions have the potential to enhance standard treatment and facilitate successful recovery. Studies like this emphasize the relationship between treatment, the rehabilitation of neural and behavioral aspect critical to addiction recovery, and suggest the therapeutic potential of mindfulness intervention for opioid use disorder. Additional funding is needed to explore whether these outcomes extend to opioid use disorder patients in the United States and whether outcomes are consistent with a large scale randomized controlled trial. Doing so could ultimately reveal an effective and relatively inexpensive therapeutic adjunct to standard addiction treatment.
- For treatment professionals and treatment systems: This study provides preliminary evidence that mindfulness-based interventions may be a useful adjunct to standard inpatient addiction treatment for opioid use disorder. Engaging in mindfulness activates brain networks that are dysfunctional after chronic repeated substance use and implicated in addiction, such as …. By activating these networks, we may be able to facilitate their structural recovery and help to alleviate the negative behaviors in which they play a role (e.g., impulsivity). Although this line of work is relatively new and needs to be replicated in different treatment settings and cultural contexts, findings like these are encouraging and suggest a potential means for enhancing opioid addiction treatment and recovery.
CITATIONS
Fahmy, R., Wasfi, M., Mamdouh, R., Moussa, K., Wahba, A., Wittemann, M., … & Wolf, R. C. (2018). Mindfulness-based interventions modulate structural network strength in patients with opioid dependence. Addictive behaviors, 82, 50-56.

